Atherosclerosis is a chronic inflammatory disease. Research has focused on identifying specific serum biomarkers to detect vulnerable plaques. These markers serve as diagnostic tools for acute coronary syndrome and assist in identifying high-risk patients. However, the existing data are limited and conflicting. This study tested the hypothesis that CD137 levels identify patients with acute coronary syndrome who are at a heightened risk for recurrent cardiac events.
METHODS:The levels of soluble CD137 (sCD137) were measured using ELISA in 180 patients with acute coronary syndrome and 120 patients with acute chest pain. Platelet activation was assessed by flow cytometry. Receiver operating characteristic curve analysis was performed to evaluate the prognostic characteristics of sCD137.
RESULTS:The levels of sCD137 were elevated in 75 patients with acute coronary syndromes and 20 patients with acute chest pain (>35.0 ng/ml). In patients with acute coronary syndrome, elevated sCD137 levels (>35.0 ng/ml) indicated an increased risk for major adverse cardiovascular events (OR = 1.93, 95% CI: 1.39-2.54). Elevated serum levels of sCD137 and cTnT were correlated with a significantly increased risk of major adverse cardiovascular events in both groups after 30 days, six months and nine months of follow-up. The increased sCD137 levels were significantly correlated with the levels of troponin I (r = 0.4799, p<0.001). Importantly, 26 patients with normal cTnI levels had acute coronary syndrome. However, elevated sCD137 levels identified these patients as a being high-risk subgroup (OR = 2.14, 95% CI: 1.25-4.13).
CONCLUSIONS:Elevated sCD137 levels indicate an increased risk of cardiovascular events in patients with acute coronary syndrome. Soluble CD137 may be a useful prognostic marker or indicator for adverse events in patients with acute coronary syndrome.
Acute coronary syndrome (ACS), including unstable angina and non-ST and ST segment elevation myocardial infarction, is the leading cause of mortality and morbidity worldwide (1,2). Despite the use of electrocardiogram and biochemical markers to assist in the diagnosis and monitoring of ACS, patients are still misdiagnosed in the emergency department or suffer an acute coronary event and die without having presented prior symptoms (3,4). Although the use of sensitive troponin assays has improved diagnostic capabilities, additional biomarkers would be particularly useful for identifying patients who are at long-term risk after presentation. Several acute-care markers, such as OX40, PAPP-A, and C-reactive protein, have longer-term predictive value in patients with ACS (5-6). However, other at-risk patients may not be identified because none of these biomarkers indicate unstable plaques. Markers in the bloodstream, such as troponin and creatine kinase-MB, indicate myocardial injury but are not necessarily elevated in patients with unstable angina or early myocardial infarction. A circulating marker that signifies unstable plaques in the coronary arteries could provide additional and powerful diagnostic information for patients with ACS. This type of marker would also improve the prognosis of patients with chest pain and may identify those patients who are at risk for developing ACS.
Several studies have shown that CD137 is expressed in human atherosclerotic plaques and patients with ACS (8-10). Jeon et al. (11) recently reported that CD137 (4-1BB) deficiency reduced atherosclerosis in hyperlipidemic mice. This information suggests that CD137 is potentially related to the development of atherosclerotic plaques. However, the additive predictive value of sCD137 in troponin-negative ACS patients has not been evaluated. The present study assessed whether there is additive diagnostic value by measuring circulating sCD137 levels in patients with suspected ACS and normal troponin values at the time of hospital admission. A cutoff value that could be applied in routine clinical practice was calculated and validated. The study also tested the hypothesis that combined assessment of sCD137 and the validated cTnI marker leads to an improved prognosis.
MATERIALS AND METHODSThe study was reviewed and approved by the institutional review committee, and informed consent was obtained from all patients and control subjects.
ReagentsA sCD137 ELISA kit from Bender MedSystems (Campus Vienna Biocenter, Vienna, Austria) was used (detection limit of 0.1 ng/ml). A troponin I kit was obtained from Triage and Biosite. A CD61-FITC-conjugated antibody was purchased from Pharmingen.
Patients and control subjectsThe trial enrolled 180 patients with ACS who had recurrent chest pain at rest in association with electrocardiographic changes or elevated serum cardiac markers. These patients had substantial coronary artery disease, as documented by coronary angiography, with stenosis of at least 70 percent of the coronary artery diameter at a culprit lesion. All patients were followed for 30 days, six months and nine months for major adverse cardiovascular events (MACEs), including acute myocardial infarction (AMI), sudden death and recurrent angina. A total of 102 patients with acute chest pain lasting less than 6 hours and no ST-segment elevation on electrocardiography were also enrolled. The presence of coronary artery disease was documented by one of the following criteria: electrocardiographic evidence of myocardial ischemia (new ST-segment depression or T-wave inversion) and a history of coronary heart disease (myocardial infarction or coronary revascularization, a positive exercise stress test or narrowing of at least 50% of the luminal diameter of a major coronary artery on a current angiogram). Patients without coronary heart disease had a normal coronary angiogram. Patients with an infection, a tumor, or liver or kidney diseases were excluded.
Blood sampling protocolIn ACS patients, blood samples were collected from the forearm at pre-determined time intervals after admission. In the patients with acute chest pain, peripheral venous blood was drawn into blood collection tubes with sodium citrate to obtain monocytes or without sodium citrate to obtain serum upon arrival in the emergency room. Peripheral venous blood mononuclear cells were obtained by Isopaque-Ficoll gradient centrifugation and placed in plastic flasks. Monocytes were harvested by scraping and collected in RPMI 1640 medium. Non-sodium citrate-treated blood was immersed in melting ice and allowed to clot for 1 h before centrifugation (1500×g for 10 min at 4°C). The supernatant was stored at -80°C until analysis. Samples were only thawed once.
Detection of sCD137 and troponin T by ELISAsCD137 levels were determined by ELISA. The intra-assay and inter-assay coefficients of variation were <9%. The concentrations of troponin I were determined using the Triage and Biosite system (lower detection limit of 0.04 ng/ml).
Detection of platelet activationIn vivo platelet activation was performed as previously described (12). Briefly, peripheral venous blood was collected in tubes containing sodium citrate. Circulating monocyte-platelet aggregates indicated activation of the platelets. Monocyte-platelet aggregates were defined as monocytes that were positive for glycoprotein IIIa using a CD61 monoclonal antibody. The values are expressed as the percent of aggregated monocytes.
Statistical analysisStatistical evaluation was performed using Graph Pad software (Prism 3.0) and the univariate program in SPSS 11.5 software. Data are expressed as the mean±SD. Differences between groups were analyzed by one-way ANOVA (post-hoc LSD). Spearman rank correlation was used to assess the relationship between two quantitative variables with non-normal distribution. The Wilcoxon rank-sum test was used to compare the levels of sCD137 between cases with and without clinical end points. Univariate and multivariate associations were analyzed using the Cox proportional hazards model to evaluate the independent contributions of variables at the nine-month follow-up to the risk of MACEs. All hazard ratios were adjusted for diabetes, hypertension, hypercholesterolemia and cTnI. p-values less than 0.05 were considered to be significant.
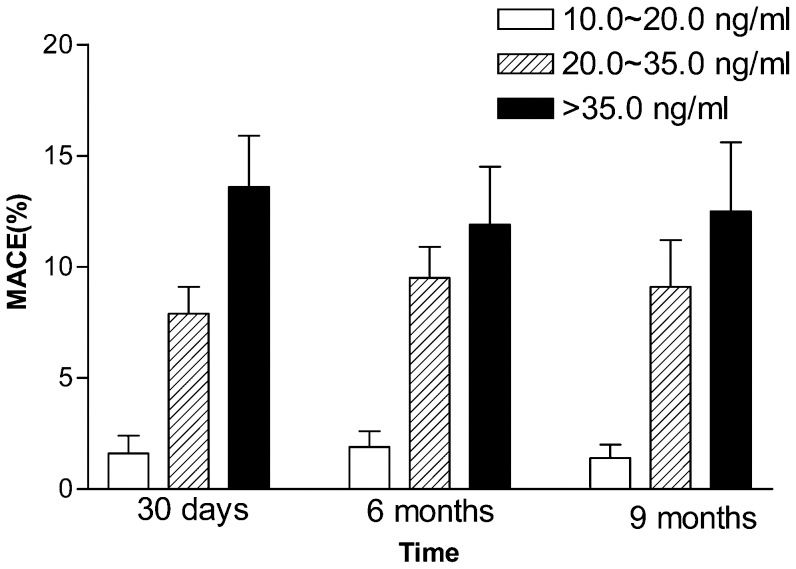
RESULTSBaseline sCD137 and adverse events in patients with ACSThe 180 patients with ACS were classified according to their baseline levels of sCD137. There were 31 patients in the first group (10.0-20.0 ng/ml), 74 patients in the second group (20.0-35.0 ng/ml) and 75 patients in the third group (>35.0 ng/ml). Elevated sCD137 levels (>35.0 ng/ml) indicated an increased risk for MACEs (odd's ratio (OR) = 1.93, 95% confidence interval (CI): 1.39-2.54). There were no significant differences in the baseline characteristics of the three groups (Table 1). At the 30-day, six-month and nine-month follow-ups, the rates of MACE were significantly higher in the second and third groups (Figure 1). Multivariate analysis using sCD137 as a continuous variable revealed that the sCD137 levels (>35.0 ng/ml) were associated with a higher risk of AMI (RR = 2.18, 95% CI: 1.27-4.25, p = 0.011), sudden death (RR = 1.82, 95% CI: 1.13-3.58, p = 0.031) and recurrent angina (RR = 2.63, 95% CI: 1.41-5.03, p = 0.019).
Baseline characteristics according to sCD137 levels.
| Groups | Low (n = 31) | Middle (n = 74) | High (n = 75) | p-value |
|---|---|---|---|---|
| (10.0-20.0 ng/ml) | (20.0-35.0 ng/ml) | (>35.0 ng/ml) | ||
| Age , Y | 62.1±10.4 | 61.7±11.7 | 62.4±11.8 | 0.15 |
| Sex, M/F | 19/12 | 45/29 | 46/29 | 0.34 |
| Risk factors, % | ||||
| Diabetes | 12.9 | 12.2 | 13.4 | 0.86 |
| Hypertension | 25.8 | 25.7 | 26.7 | 0.77 |
| Hypercholesterolemia | 9.7 | 9.5 | 10.7 | 0.53 |
| Smoking | 22.6 | 23.0 | 22.7 | 0.51 |
| Clinical history, % | ||||
| STEMI | 42.0 | 41.9 | 42.7 | 0.61 |
| NSTEMI | 29.1 | 28.4 | 29.4 | 0.47 |
| UA | 28.9 | 29.7 | 27.9 | 0.83 |
| Prior medication, % | ||||
| Aspirin | 93.6 | 93.3 | 93.4 | 0.94 |
| Statin | 22.6 | 23.0 | 22.7 | 0.58 |
| Beta-blockers | 71.0 | 70.3 | 70.7 | 0.61 |
| ACEI | 45.2 | 44.6 | 45.4 | 0.71 |
STEMI: ST-elevation myocardial infarction. NSTEMI: non-ST-elevation myocardial infarction. UA: unstable angina. ACEI: angiotensin-converting enzyme inhibitor.
The relationship between baseline sCD137 levels and the rate of major adverse cardiovascular events (MACEs) at 30 days, 6 and 9 months in 180 patients with ACS. Data are presented as bars; the bar length represents the mean value for each group, and the error bars show the standard error of the mean.
We observed a significant correlation between sCD137 levels and cTnI levels (r = 0.4799, p<0.001 n = 154, Figure 2A). At the 30 day, six month and nine month follow-ups, patients with high levels of sCD137 and cTnI had a markedly increased risk of MACE. Patients with low levels of sCD137L and cTnI had a low rate of MACE. Of the 26 cTnI-negative subjects (<0.04 ng/ml) with ACS, increased sCD137 levels identified a subgroup of high-risk patients within these cTnI-negative patients (OR = 2.14, 95% CI: 1.25-4.13) (Figure 2B).
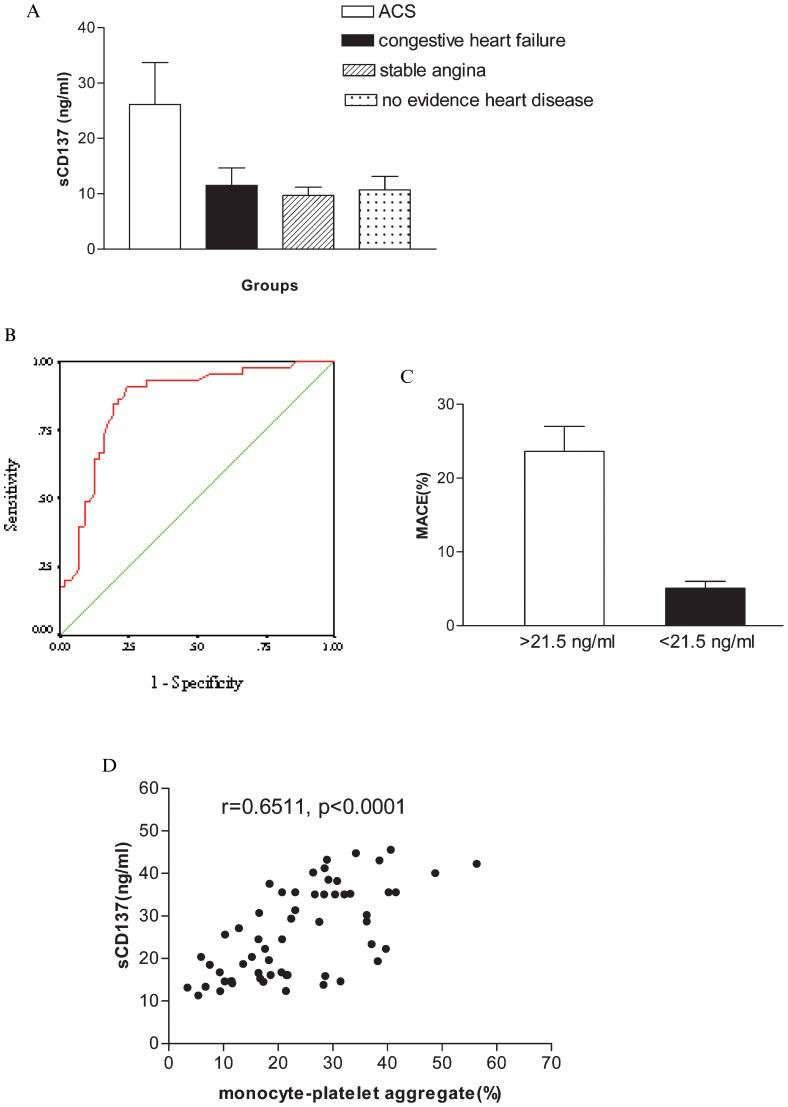
Prospective validation of patients with acute chest pain in the emergency roomOf the 102 patients with acute chest pain, 59 patients had ACS. The remaining 43 patients had congestive heart failure, stable angina or no evidence of heart disease. Serum sCD137 levels were significantly higher in the 59 patients with ACS (Figure 3A). A total of 20 patients had high levels of sCD137 (>35.0 ng/ml). Using receiver operating characteristic (ROC) curves, we identified a positive value for predicting ACS using the sCD137 level. The area under the curve (AUC) was 0.858±0.04 (95% CI, 0.783-0.934; p<0.001, Figure 3B). Based on the ROC curve, we derived an optimal cutoff value of 21.5 ng/ml for sCD137. Levels of sCD137 above or below this cutoff value were associated with MACE rates of 23.6% and 5.1%, respectively (p<0.001, Figure 3C). The sensitivity was 76.3%, the specificity was 78.3%, and the negative predictive value was 99%. We observed a strong correlation between platelet activation, as evidenced by the percent of monocyte-platelet aggregates, and sCD137 levels in the subgroup of 59 ACS patients (r = 0.6511, p<0.0001, n = 59, Figure 3D).
Baseline sCD137 levels and platelet activation in patients with acute chest pain. A) The baseline sCD137 levels in patients with ACS, congestive heart failure, stable angina and no evidence of heart disease. B) ROC curves for predicting ACS using sCD137. C: MACE rate relative to sCD137 values. D: The correlation between baseline sCD137 levels and monocyte-platelet aggregates.
After adjusting for baseline characteristics, the patients with sCD137 levels >21.5 ng/ml continued to be at increased risk for MACE (HR 2.32, 95% CI 1.72-3.18, p<0.001). After adding cTnI to the multivariable model, the relationship between sCD137 and MACE remained significant (HR 2.61, 95% CI 1.93-3.52, p<0.001) (Table 2).
Hazard ratios (HRs) (95% CI) associated with sCD137 >21.5 ng/ml for MACE after multivariable adjustments.
| Model | HR (95% CI) | p-value |
|---|---|---|
| Unadjusted | 2.34 (1.71-3.15) | <0.0001 |
| Baseline characteristics (adjusted for age, gender, Smoking, diabetes, hypertension, hypercholesterolemia, clinical history and prior medication) | 2.31 (1.72-3.18) | <0.0001 |
| Baseline characteristics+cTnI | 2.61 (1.93-3.52) | <0.0001 |
A number of biochemical markers provide important insights into different aspects of the pathobiology of ACS and are used to assist in risk stratification following a cardiovascular event. In this study, sCD137 levels assisted in identifying patients who were at an increased risk of MACE. This marker may provide an additional pathophysiological procedure for evaluating patients with ACS.
Increasing evidence has suggested that the CD137-CD137L system plays an important role in coronary disease progression and plaque destabilization. In vitro and in vivo studies have demonstrated a crucial role for CD137 at multiple stages of atherosclerosis and ACS (11,13). We recently demonstrated that patients with ACS showed increased expression of soluble and membrane-bound CD137 (which marks peripheral). We also observed a significant correlation between CD137 levels and complex coronary stenoses in patients with ACS (10). These data suggest that increased CD137 may be a reliable biomarker for coronary disease and may also play an important role in disrupting vulnerable atherosclerotic plaques in ACS.
In the present study, the rates of MACE were significantly higher in the second (sCD137, 20.0-35.0 ng/ml) and third ACS groups (sCD137, >35.0 ng/ml). The levels of sCD137L were significantly correlated with cTnI levels in ACS patients. However, in the 26 cTnI-negative subjects with ACS, high sCD137 levels identified patients who were at risk for MACE and were not detected by cTnI (<0.04 ng/ml) alone. Patients with normal cTnI levels and increased sCD137 levels were at an increased risk for cardiovascular events. In the cTnI-negative ACS patients, the cumulative nine-month MACE was 7.9%. These results suggest that measuring circulating sCD137 can provide efficient risk assessments in such patients. A single measurement of sCD137 at the time of hospital admission showed significant predictive power for future cardiovascular events. However, the kinetics of sCD137 release and the corresponding optimal sampling protocols for ACS should be standardized.
Cardiac troponin markers for myocardial necrosis have become the gold standard biochemical marker for diagnosing and determining the prognosis in patients with ACS (1,14,15). However, these markers are not indicative of the pathophysiology of ACS and unstable plaques. In contrast, CD137 may be directly involved in the underlying mechanisms that disrupt the vulnerable plaques in ACS. Recent evidence suggests that CD137-CD137L interactions contribute to the progression of atherosclerotic plaques (16,17). In this study, sCD137 was a reliable prognostic marker that provided additional information to the troponin I results. Multivariable modeling suggested that sCD137 offers prognostic information independent of other clinical predictors. After cTnI was added to the multivariable model, the relationship between sCD137 and MACE remained significant.
ACS results from the disruption of atherosclerotic plaques, leading to coronary thrombosis. Platelet activation is the core of thrombus formation, which precipitates the majority of unstable plaques and coronary syndromes. A previous study demonstrated that circulating monocyte-platelet aggregates are a more sensitive marker of in vivo platelet activation than platelet surface P-selectin, which is considered to be the “gold standard” marker of platelet activation (12). In the acute chest pain group, platelet activation was closely correlated with sCD137 levels in patients with ACS. Thus, sCD137 not only contributes to the pathophysiology of ACS but also represents a reliable and powerful clinical marker for identifying patients with high-risk atherosclerotic lesions and coronary thrombosis.
In summary, the results of the present study demonstrate that elevated levels of sCD137 are associated with increased cardiac risk. The predictive value of sCD137 levels was independent of elevated troponin I levels. Increased sCD137 levels are a marker of plaque instability that favors progression to ACS and are indicative of a poor prognosis even after the occurrence of an acute ischemic event caused by plaque instability. However, the use of elevated sCD137 as a tool to guide therapy should be further elucidated. The relatively small number of patients in this study should be taken into account. Studies using a larger cohort of patients should be performed to establish the clinical use of sCD137 independently of or in combination with other markers to predict cardiovascular events after ACS.
This project was supported by the Natural Science Foundation and the development health engineering Foundation in Jiangsu Province (BK2011486, LJ201116), the National Natural Science Foundation of China (81170279) and Social Development in Zhenjiang (SH2010012).
No potential conflict of interest was reported.
Yan JC was responsible for the study planning and execution, data collection and manuscript writing. Wang CP designed the study, wrote and reviewed the manuscript. Chen R was responsible for clinical follow-ups and data collection. Yang HB performed the statistical analyses.