Vulvar Paget's disease is very rare malignancy originating in vulvar apocrine-gland-bearing skin cells or as a manifestation of adjacent primary anal, rectal or bladder adenocarcinoma.1 It is also called extramammary Paget's disease and affects both sexes, in the vulvar, perineal or scrotal areas. Vulvar Paget's disease is most commonly seen in postmenopausal Caucasian females and appears clinically as red, eczematous and pruriginous – and sometimes painful – lesions. In most cases it is an intraepidermal adenocarcinoma in which tumor cells involve the epidermis and sometimes the underlying skin appendage, but sometimes there is focal dermal invasion.2
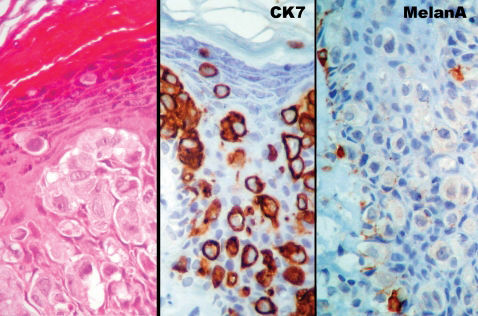
Probably because of its multicentric nature, Paget's disease has a chronic and relapsing course. Surgery has been the treatment of choice, but disease frequently extends far from the visible lesion and surgical margins are frequently positive. The Paget's cells are larger than keratinocytes, have clear chromatin, a prominent nucleolus and gray–blue cytoplasm and they may appear vacuolated with hematoxylin and eosin staining.3 All these characteristics are consistent with their glandular nature.
Many patients undergo multiple surgical procedures, including wide local excision, simple vulvectomy or radical vulvectomy. However, the margins of primary surgical specimens are positive in more than half of the patients.3 Consequently, the recurrence rate is about 47%.4
The disappointing results of surgical treatment and the high morbidity and side-effects of extensive vulvar resection have encouraged many authors to try innovative clinical treatment for vulvar Paget's disease.
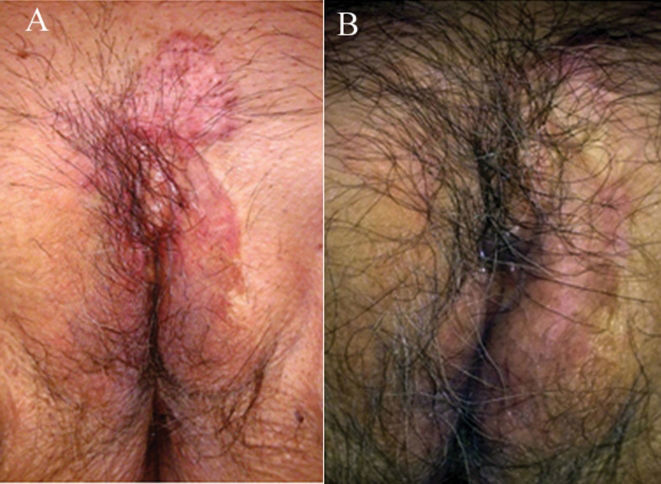
CASE REPORTAn 84-year-old female patient sought treatment with the complaint of itching in the pubic area. She presented with a large hyper-pigmented to pink plaque extending through the pubic area and left great labia (Figure 1A). Biopsy resulted in a diagnosis of Paget's disease based on hematoxylin–eosin staining and the immunohistochemical profile (negative Melan-A and positive cytokeratin 7) (Figure 2).
The treatment proposed was surgery with wide local resection and margin control by frozen section examination. The patient refused any kind of surgical treatment. As an alternative treatment, we proposed topical imiquimod 5% cream, to be applied every other day, on the affected area for at least 16 weeks.
In the first two weeks of treatment she reported local burning, small erosion areas, two episodes of fever (38°C) and flu-like symptoms, which lasted until the fourth week. By the end of 16 weeks, there was clinical reduction of the lesion. The patient agreed to be subjected to multiple control biopsies. Pathological examination showed that the tissue remained positive for Paget's disease. We decided to continue with another course of imiquimod 5% cream treatment for a further nine weeks. At the end of 25 weeks of treatment we performed other multiple biopsies, which showed no residual disease (Figure 1B).
DISCUSSIONFor a long time, the standard treatment for vulvar Paget's disease has been surgery with intraoperative margin control, but results have been very disappointing. Positive margins and recurrence rates are greater than 50%. Otherwise, wide local resection brings major functional anogenital–vulvar defects.
Alternative non-surgical or combined treatments have been proposed, including radiotherapy, topical chemotherapy with intralesional interferon alfa-2b, CO2 laser ablation, photodynamic therapy with topical aminolevulinic acid, topical fluorouracil (5-FU), and imiquimod 5% cream.5
Radiotherapy has been used both as a definitive treatment as well as in the postoperative setting to prevent local recurrence, mainly in the management of anogenital Paget's disease. Moreno-Arias et al.6 reported a dosage of radiotherapy in the range 40–50 Gy resulting in low recurrence rates, but others have observed recurrences in patients treated with slightly lower radiotherapy total doses.5
Tanaka et al.7 reported 14 cases of extramammary Paget's disease, four of which involved women with disease in the vulvar, groin or perianal areas. Treatment included surgery, radiation therapy, photodynamic therapy, CO2 laser therapy and, in one case, imiquimod cream application. All four cases of female genital Paget's disease recurred or persisted. Imiquimod 5% cream appears to be a promising option for clinical treatment of vulvar Paget's disease. The case that was treated with imiquimod cream 5%, reported by Tanaka et al.,7 was a very extensive vulvo-perineal lesion that showed more than 50% local regression after only 5 weeks of treatment. The residual lesion was subjected to other kinds of treatment.
Wang et al.8 reported a six-week course of nightly treatment with imiquimod 5% cream for a recurrent case of vulvar Paget's disease. The patient reported marked local irritation, erosions, and tenderness, but did not report flu-like symptoms, nausea or diarrhea. Two weeks after completion of therapy, the patient did not have symptoms of itching or burning and there was no clinical evidence of residual Paget's disease. A post-treatment skin-biopsy specimen showed no atypia in the epidermis.
Hatch and Davis9 reported two women with vulvar Paget's disease who achieved biopsy-confirmed resolution of their disease after topical application of imiquimod 5% cream.
Geisler and Manahan10 reported the case of an 80-year-old woman with recurrent Paget's disease of the vulva. She had undergone multiple resections for the disease over a 12-year period. After a course of topical imiquimod, a post-treatment biopsy proved histological regression of the disease. Bertozzi et al.11 reported on a 71-year-old patient with recurrent disease treated successfully with imiquimod cream. Within eight weeks, complete clinical remission was achieved.
Sendagorta et al.12 reported on three patients diagnosed with vulvar Paget's disease who were each treated with a daily application of imiquimod 5% cream for three weeks, followed by a further three weeks of application every other day. Complete clinical and histological remission of the disease was achieved in the three patients. Mild irritation and tenderness were observed as the only side-effects.
Tonguc et al.13 reported on the case of a 65-year-old woman initially treated by means of a wide vulvar excision: she had experienced two recurrences of the disease. Our patient also refused any kind of surgical treatment with imiquimod cream 5%.
Our patient, however, had refused any kind of surgical treatment, so she was convinced to try local treatment with 5% imiquimod cream instead. At the end of a total of 25 weeks of treatment (16 weeks followed by 9 weeks), multiple vulvar biopsies showed no residual disease. Our excellent results are in accord with the literature reports and suggest that imiquimod cream appears to be an effective and safe therapeutic agent for vulvar Paget's disease.
Until now, most patients treated with imiquimod cream have been those with recurrent disease. Our patient, however, experienced initial treatment with imiquimod cream. These promising results warrant further studies to determine the real efficacy and safety of imiquimod 5% cream for the treatment of extramammary Paget's disease.