Diabetic foot is considered to be one of the most serious complications for patients suffering from Diabetes Mellitus (DM). Approximately 20–25% of all diabetic patients will present with lower extremity ulceration at some time in their lives. Diabetic foot is the leading cause of non-traumatic lower limb amputations in the world, resulting in an amputation risk for diabetic patients that is approximately 40 times greater than that of the general population. Post-amputation mortality is extremely high, with a three-year survival rate of 65% and a five-year survival rate of 41%. It is a health issue affecting several countries and represents a significant socioeconomic problem.1–4 In Brazil, amputation, admission, ulceration, and cost data are similar to other Western countries.5–7 Recognition of individuals at risk for ulceration, followed by adequate intervention, may reduce the chance of unfavorable results up to 80%.8
Peripheral sensory-motor neuropathy, which is responsible for the progressive loss of protective and proprioceptive sensations, is considered the main agent of the clinical abnormalities found in diabetic foot patients. It is important to consider that in the final phases of the disease the patient may present with a completely insensitive foot.9,10 One of the first studies looking to improve touch sensitivity screening dates back to 1898 and used a horsehair attached to a thorn.11 This method was refined and currently a 10g nylon monofilament, developed by Semmes and Weinstein, is accepted as the gold standard for detecting ulcer risk.12 Its reproducibility and predictive value lead the World Health Organization (WHO) and the International Diabetes Federation (IDF) to recommend its use in clinical practice.1,2
In 2006, Bourcier et al. showed the effectiveness of the “house made” monofilament, constructed from a fishing line, for screening for diabetic foot. The main characteristic of this line is that it exerts a 10 g pressure when bent (4 cm length by 500 μm diameter N° M-1425, South Bend Inc. North Brook, EUA).13 In Brazil, the 10 g monofilament is produced locally, but is not always available for purchase.
The objective of this study was to identify a similar nylon line and compare it to the commercially available one.
METHODOLOGYThis was a prospective, investigative, non-interventionist study with minimal risk to the participants. It was approved by the Local Ethics in Research Committee (CAPPesq n° 1184/09) and informed consent was obtained from all subjects who agreed to participate.
The study consisted of three phases. Initially, we assessed the fishing lines available in the national market that presented bending characteristics similar to the 10 g monofilament. If possible, we identified lines that did not require any other device for clinical use, i.e. the only holding structures could be the thumb and index finger of the examiner. This step was done inside the laboratory using a precision digital scale (OHAUS Max model – capacity = 210 g/d = 1 mg).
In the second phase, we evaluated the chosen line, referred to here as the “white-line”, in relation to the commercially available (SORRI-BAURU), referred to here as the “yellow-line”. We proceeded with the clinical evaluation of this filament in 100 healthy (56 male and 44 female), non-diabetic medical students and physicians from the State University of Sao Paulo who volunteered for the study. The diabetes criteria used to select this group followed the ADA (American Diabetes Association) diabetes diagnosis criteria. To exclude the presence of abnormalities in lower limb sensations in this group, all individuals submitted to a clinical evaluation using vibration perception (128 Hz tuning fork) at two sites (hallux pulp and malleolus) and point pressure (Semmes-Weinstein 10 g monofilament) at five sites (halux, 3rd toe, 1st, 3rd, and 5th metatarsal heads). No individuals presented with any kind of insensitivity.
Evaluation with the new monofilament was compared to the commercially available monofilament. Subjects were evaluated in the sitting position. Each filament was initially applied to the back of the hand so that it could be identified and then randomly applied to the foot sole at the following sites (3 times each): halux, 3rd toe, 1st, 3rd, and 5th metatarsal heads. Individuals were asked to close their eyes and identify which filament was being used at each time.
The third phase was carried out in two distinct diabetic foot reference units (Diabetic Foot Unit, Endocrinology and Metabolism Division at the State University of São Paulo and the Medical Specialties Centre of Aracaju-CEMAR). We invited 190 diabetic subjects (80 male and 110 female) with a history of at least 5 years of disease (according to the ADA diabetes diagnosis criteria) to participate in this study. One hundred of the subjects had a previous diagnosis of clinical diabetic neuropathy and 90 did not. One patient declined to participate. All patients were re-examined to confirm their diagnosis and no discordance with the cited criteria was found.
The neuropathy criteria used in both diabetic foot units were the absence of vibration perception (128 Hz tuning fork) in at least one site (hallux pulp and/or malleolus), insensitivity to plantar point pressure (Semmes-Weinstein 10 g monofilament in at least one of seven sites), ankle reflex reduction, and/or absent answer.2 We again evaluated both filaments, as described above. Answers were recorded as present/absent.
Data from phases 2 and 3 was organized into tables of contingency and analyzed by the Chi-Square method after Pearson's correction. Significance value was fixed at 5%. The kappa coefficient was used as a measure of inter-annotator agreement for qualitative (categorical) items. Kappa coefficient was expected to be equal to 1 if the 2 evaluation methods were in complete agreement.
RESULTSPhase 1: We initially investigated the physical characteristics of lines with diameters and raw materials that allowed compression in “grams”. There were 6 lines that fulfilled such criteria. We obtained a 10 g bend in the Nylon 6 (homopolymer) line, which had a diameter of 0.50 mm cut at a length of 4 cm (Table 1). This result was confirmed in 100 consecutive tests by 2 different examiners (50 tests per examiner), who used the thumb and index finger to hold the line. This line used in the fabrication of fishing nets and rod sport fishing (TREVO brand, Equipesca, SP-Brazil) and is available in 250 g reels.
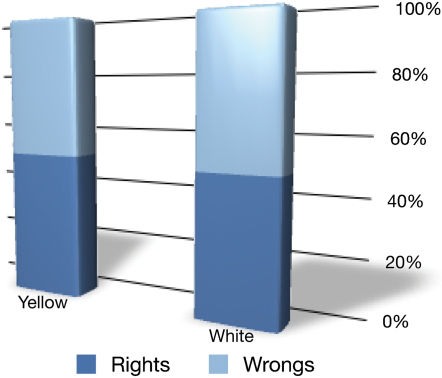
Phase 2: Chi-Square analysis of the 5 sites studied showed that the individuals were incapable of differentiating between the touch of the 2 filaments (p<0.05, Figure 1).
Phase 3: The patient analysis showed a satisfactory concordance between answers for both monofilaments. There was no difference in results at any site evaluated. Correlation coefficients (k) confirmed the equivalence of both nylon filaments with a variation of 0.96 to 1.00. This value was 0.96±0.02 (p<0.05) and 0.98±0.01 (p<0.05) for the right and left foot, respectively (Table 2).
Correlation coefficients for the sites studied.
| Right Foot | Halux | 3rd toe | 1st metatarsal head | 3rd metatarsal head | 5th metatarsal head |
|---|---|---|---|---|---|
| kappa | 0.96 | 1.00 | 0.97 | 0.97 | 0.98 |
| Standard Error | 0.02 | 0.019 | 0.17 | 0.013 |
| Left Foot | Halux | 3rd toe | 1st metatarsal head | 3rd metatarsal head | 5th metatarsal head |
|---|---|---|---|---|---|
| kappa | 0.97 | 0.98 | 1.00 | 0.98 | 1.00 |
| Standard Error | 0.016 | 0.012 | 0.012 |
The present study shows that it is possible to reduce the cost of detecting ulcer risk of the foot in diabetic patients. In the initial phase of the research we sought to find a fishing line available in the nation market that had characteristics similar to the 10 g internationally standardized monofilament in terms of composition and bending. We subjected these lines to evaluation of their physical and tonometric characteristics. Non-diabetic individuals were not capable of differentiating one monofilament from the other. A previous study found similar results with a different line that also reproduced the necessary characteristics.12–20 When we tested, in a patient-blind way, both monofilaments in diabetic patients with and without neuropathy, we found similar results. The kappa values revealed the strong concordance of the lines. It is worth noting that the population studied was multicentric, representative, and homogeneous, with no demographic differences from other local populations previously described.21,22
Bourcier et al.13 developed their fishing line instrument to foment patient auto-examination. We had a very distinct socioeconomic goal for addressing this public health concern. Our study was conducted in a country with a developing economy that has huge inter-regional, social, and economic differences. Performing routine foot screening in the various health units in Brazil faces a lack of capacitation and adequate material. Thus, with the exception of a few reference centers, the great majority of health services across the country, particularly primary care units, do not perform screening for the risk of diabetic foot. Therefore, we are justified to repeat a study already done in another country but with a line that is easy to obtain locally.
The present cost of the commercially available monofilament is R$7.00 (USD 3.68) per unit (two lines in a kit). The studied line is produced commercially on large scale for exportation and is also sold all over the country. Its unit cost is only R$0.00053 (USD 0.00029). The cost savings this line may generate are significant, potentially allowing access to this instrument at locations with few resources as well as supporting its day-to-day use. Indirectly, it can also reduce the costs of diabetic foot complications through early detection.
The line was developed to not need any support instruments. The examiner's fingers act as the necessary pincer. Any attempt to modify this technique, such as fixation to paper or plastic, will alter the line's physical properties and, in so doing, will necessitate new studies. It is also noteworthy that lines from other brands could also be used, but similar studies are necessary to validate their equivalence.
This study has its limitations. We used the same materials to fabricate the monofilaments and all were made by the same person. For large-scale use, caution should be taken in regards to the line's fabrication in order to avoid use of lines of different brands and measures, preventing inadequate accuracy. We also realize that in the present study there were no new findings: a 10 g monofilament derived from a fishing line performs as a 10-gram nylon monofilament. However, at the public health policy level, this confirmation was critical. The encouraging results of Bourcier et al. can be expanded to include locally available materials.
CONCLUSIONWe have demonstrated that a low cost instrument developed from a fishing line is equivalent to instrument used internationally to evaluate ulcer risk of the foot in diabetic patients. It can be used as the standard line to screening for diabetic neuropathy.
The authors would like to thank the engineer Mr. Milton Xavier, who helped us in the first phase of this work, related to the search of fishing line suitable for this study, Dr. Karla Melo for her continuous encouragement and stimulus to this paper realization and Dr. Arnaldo Moura Neto who revised the last version.