The aim of this article was to determine the effects of minimally invasive percutaneous plates versus interlocking intramedullary nailing in the treatment of tibial shaft fractures in adults.
METHOD:Literature searches of the Cochrane Library, PubMed, EMBASE, the Chinese Biomedical Literature database, the CNKI database, Wanfang Data, and the Weipu Journal database were performed up to August 2013. Only randomized and quasi-randomized controlled clinical trials comparing the use of percutaneous plates and interlocking intramedullary nails for tibial shaft fractures were included. Data collection and extraction, quality assessment, and data analyses were performed according to the Cochrane standards.
RESULTS:Eleven trials were included. Compared with interlocking intramedullary nailing, minimally invasive percutaneous plates shortened fracture healing time and resulted in lower rates of postoperative delayed union and pain. There was no significant difference between the two methods with regard to the rates of excellent and good Johner-Wruh scoring, the rate of reoperation, and other complications.
CONCLUSIONS:Overall, insufficient evidence exists regarding the effects of minimally invasive percutaneous plates versus interlocking intramedullary nailing in the treatment of tibial shaft fractures in adults. Low-quality evidence suggests that minimally invasive percutaneous plates could shorten fracture healing time, decrease the rate of postoperative delayed union, and decrease pain levels compared with interlocking intramedullary nailing. There is no significant difference between the two groups in terms of functional recovery scores, reoperation, and other complications. Further research that includes high-quality randomized controlled, multicenter trials is required to compare the effects of minimally invasive percutaneous plates versus interlocking intramedullary nailing in the treatment of tibial shaft fractures in adults.
Tibial shaft fractures are primarily caused by high-energy trauma, such as motor vehicle accidents, sports injuries, and falls from a height; they are the most common diaphyseal fractures in adults. Although there are several treatment methods for tibial shaft fractures, no one method is appropriate for all types of tibial shaft fractures (1). Because of its positive features, interlocking intramedullary nailing is considered to be the preferred method for tibial fractures that require surgical intervention. The insertion point is distant from the traumatized tissues at the injury site, and the nail has a mechanical advantage by being at the load-bearing axis (2). Minimally invasive percutaneous plates provide an alternative to manage these lesions. Minimally invasive percutaneous plating is inserted percutaneously through a small incision, thereby providing stability and minimizing any intraoperative iatrogenic soft tissue damage (3-4). This technique is widely applied in clinics, with excellent results (5-7). The objective of this systematic review and meta-analysis is to determine the effects of minimally invasive percutaneous plates versus interlocking intramedullary nailing in treating tibial shaft fractures in adults.
MATERIALS AND METHODSThis study was performed with guidance from the Cochrane Handbook for Systematic Reviews of Interventions (8) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (9). The literature search was performed in PubMed, the Cochrane Library, EMBASE, the Chinese Biomedical Literature database, the CNKI database, Wanfang Data and the Weipu Journal database (up to August 2013). The search strategies used in the PubMed, Cochrane Library and EMBASE databases are shown in Table1. The search strategies applied in the other databases used the following search terms: (‘Tibial Fractures’ or 'Tibial Shaft Fractures') and 'intramedullary nailing' and (‘percutaneous plating’ or ‘minimally invasive percutaneous plate osteosynthesis‘). The search was performed without language restrictions but was limited to human subjects. In addition, the reference lists of identified studies were manually checked to include other potentially eligible trials. This process was performed iteratively until no additional articles could be identified.
Search strategy.
| CENTRAL | EMBASE | PUBMED |
|---|---|---|
| #1. MeSH descriptor [Tibial Fractures] this term only | #1. “Tibial Fractures” | #1. “Tibial Fractures”[MeSH] |
| #2. MeSH descriptor [Fracture Fixation] explode all trees | #2. (“Fractures, Bone” OR “fracture healing”) AND tibia | #2. “Fractures, Bone” [MeSH] OR “fracture healing”[MeSH] |
| #3. MeSH descriptor [Fractures, Bone] explode all trees | #3. #1 OR #2 | #3. “tibia”[ MeSH] |
| #4. #2 OR #3 | #4. tibia* AND fracture* | #4. #2 AND #3 |
| #5. MeSH descriptor [Tibia] this term only | #5. shaft or diaphys* | #5. #1 OR #4 |
| #6. #4 AND #5 | #6. #3 AND #5 | #6. tibia*[ti] |
| #7. (tibia*):ti | #7. #4 AND #5 | #7. fracture*[tw] |
| #8. (fracture*):ti,ab,kw | #8. #6 OR #7 | #8. shaft [tw] or diaphys*[tw] |
| #9. (shaft or diaphys*):ti,ab,kw | #9. “fracture fixation, internal” OR “surgical procedures, minimally invasive” OR “bone screws” OR “bone plates” OR “bone nails” | #9. #6 AND #7 AND #8 |
| #10. #7 AND #8 AND #9 | #10. pin OR nail* OR screw* OR plat* OR fix* | #10. #5 AND #8 |
| #11. (#1 OR #6 ) AND #9 | #11. #9 OR #10 | #11. #9 OR #10 |
| #12. #10 OR #11 | #12. #8 AND #11 | #12. “fracture fixation, internal”[MeSH] OR “surgical procedures, minimally invasive”[MeSH] OR “bone screws”[MeSH] OR “bone plates”[MeSH] OR “bone nails”[MeSH] |
| #13. MeSH descriptor [Internal Fixators] this term only | #13. random* OR blind* | #13. pin[tw] OR nail*[tw] OR screw*[tw] OR plat*[tw] OR fix*[tw] |
| #14. MeSH descriptor [Bone Screws] explode all trees | #14. #12 AND #13 | #14. #12 OR #13 |
| #15. MeSH descriptor [Fracture Fixation, Internal] explode all trees | #15. #14 AND “randomized controlled trial”/de AND “human”/de | #15. #11 AND #14 |
| #16. MeSH descriptor [Surgical Procedures, Minimally invasive] explode all trees | #16. (“randomized controlled trial”[pt] OR “controlled clinical trial”[pt] OR randomized [tiab] OR “clinical trials as topic”[mesh: noexp] OR randomly[tiab] OR trial [ti]) NOT (animals[mh] NOT humans[mh]) | |
| #17. MeSH descriptor [Bone Plates] this term only | #17. #15 AND #16 | |
| #18. MeSH descriptor [Bone Nails] this term only | #18. #17 Filters: Clinical Trial; Humans | |
| #19. #13 OR #14 OR #15 OR #16 OR #17 OR #18 | ||
| #20. (pin or nail* or screw* or plate* or fix*):ti,ab,kw | ||
| #21. #19 OR #20 | ||
| #22. #12 AND #21 | ||
| #23. #22 Filters: trials |
The title, journal name, year of publication, authors, and abstract of each article were independently screened in duplicate by two authors (He GC and Wang QF). Inclusion decisions were made according to the following predetermined eligibility criteria: (i) Randomized and quasi-randomized controlled clinical trials were included (i.e., the study design); (ii) Skeletally mature patients (older than 18 years old) with tibial shaft fractures were included (i.e., the study population). The tibial shaft was defined as the segment of the tibia excluding the proximal and distal segments using the square rule based on the comprehensive classification of fractures of long bones. The proximal and distal segments of the tibial long bones were circumscribed by a square, the sides of which had the same length as the widest portion of the epiphysis (10); (iii) Studies that compared minimally invasive percutaneous plating versus locked intramedullary nailing to treat tibial shaft fractures in adults were included (i.e., the intervention). Additionally, studies in which minimally invasive percutaneous plating and interlocking intramedullary nailing were compared with other surgical interventions (e.g., external fixation) or with non-surgical interventions were also included; (iv) The outcome measures assessed using a predefined protocol included the functional score of Johner-Wruh criteria for evaluation of final results (the rate of excellent and good) (11), fracture healing time, reoperation, and complications. Moreover, full-text versions of the articles were obtained to assess the eligibility for all records, if it was uncertain. Disagreement between the authors was resolved by consensus, and a third author (Chen ZH) was consulted, as necessary.
Two reviewers independently extracted the following data from each included study: first author, year of publication, number of patients, number of patients lost to follow-up, type of internal fixation, functional outcomes, fracture healing time, rate of reoperation, and complications (e.g., delayed union and postoperative pain, infection/osteomyelitis, superficial infection, nonunion, internal fixation loosening or breakage, and limited ankle mobility). Methodological quality assessments of the included papers were independently performed by two reviewers following the recommendations of the Cochrane Collaboration and other experts to combine the Jadad scale with the allocation concealment evaluation method (8,12-13). Disagreement between the authors was resolved by consensus, and a third author was consulted, as necessary.
The statistical analysis was conducted using Review Manager (Version 5.2.8. The Nordic Cochrane Centre, Rigshospitalet, Denmark. download address: http://tech.cochrane.org/revman/download.). Dichotomous data are presented as risk ratios (RR), and continuous outcomes are presented as the weighted mean difference (WMD), both with 95% confidence intervals (CIs). The chi-squared test was performed, and heterogeneity was determined to be significant at I2>50% or p<0.1. Graphical exploration with funnel plots was used to evaluate publication bias. A random effects model was used if the heterogeneity was significant, and a fixed effects model was used when the heterogeneity was not significant.
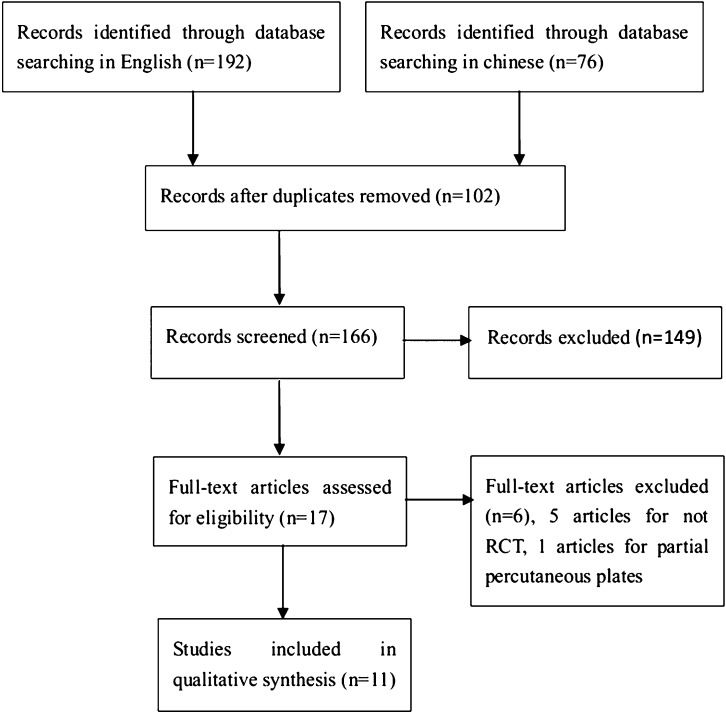
RESULTSThe selection flow is shown in Figure1. Eleven studies matched our inclusion criteria (14-24). Table2 summarizes the key characteristics of the included studies, and Table3 summarizes the methodological quality criteria (12). A total of 734 patients with tibial shaft fractures were included in this study. All fractures used the Arbeitsgemeinschaft für Osteosynthesefragen (AO [Association for the study of internal fixation, ASIF]) classification. In addition, fractures were also classified as closed and open fractures in the included studies. All open fractures were classified using the Gustilo open fracture classification.
Characteristics of the included studies.
| Study | Year | Single- or multicenter trials | Participants | Fractures | Number of percutaneous plate | Number of intra-medullary nail procedures | Loss to follow-up | Percutaneous plates | Intramedullary nails |
|---|---|---|---|---|---|---|---|---|---|
| Fernandes | 2006 | Multicenter | 45 | 45 | 22 | 23 | None | Bridging plates | Nonreamed interlocking nails |
| Zhou | 2012 | Single center | 54 | 54 | 27 | 27 | None | Percutaneous locking plates | Interlocking intramedullary nails |
| Zhang | 2012 | Single center | 58 | 58 | 29 | 29 | None | Percutaneous locking plates | Interlocking intramedullary nails |
| Yan | 2011 | Single center | 80 | 80 | 40 | 40 | None | Percutaneous locking plates | Interlocking intramedullary nails |
| Tang | 2010 | Single center | 80 | 80 | 40 | 40 | None | Percutaneous locking plates | Interlocking intramedullary nails |
| Shi | 2011 | Single center | 66 | 66 | 34 | 32 | 5 | Percutaneous locking plates | Interlocking intramedullary nails |
| Li | 2010 | Single center | 68 | 68 | 34 | 34 | None | Percutaneous locking plates | Interlocking intramedullary nails |
| Jiang | 2012 | Single center | 40 | 40 | 20 | 20 | None | Percutaneous locking plates | Interlocking intramedullary nails |
| Chen | 2008 | Single center | 85 | 85 | 50 | 35 | None | Percutaneous locking plates | Interlocking intramedullary nails |
| Chen | 2005 | Single center | 66 | 66 | 34 | 32 | 5 | Percutaneous locking plates | Interlocking intramedullary nails |
| Chen | 2012 | Single center | 92 | 92 | 46 | 46 | None | Percutaneous locking plates | Interlocking intramedullary nails |
Methodological quality of the included studies.
| Study | Randomization methods | Allocation concealment | Blinding | Intention-to-treat | Jadad score |
|---|---|---|---|---|---|
| Fernandes | Not stated | Not stated | Not stated | Yes | 2 |
| Zhou | Not stated | Not stated | Not stated | Yes | 2 |
| Zhang | Not stated | Not stated | Not stated | Yes | 2 |
| Yan | Not stated | Not stated | Not stated | Yes | 2 |
| Tang | Not stated | Not stated | Not stated | Yes | 2 |
| Shi | Not stated | Not stated | Not stated | No | 1 |
| Li | Not stated | Not stated | Not stated | Yes | 2 |
| Jiang | Random number table | Not stated | Not stated | Yes | 3 |
| Chen08 | Not stated | Not stated | Not stated | Yes | 2 |
| Chen05 | Not stated | Not stated | Not stated | No | 1 |
| Chen12 | Not stated | Not stated | Not stated | Yes | 2 |
Nine studies reported functional recovery scores (14,16-19,21-24). One study used a customized functional score (18), and the others used the Johner-Wruh functional score to evaluate the final results. There were no significant between-group (i.e., the minimally invasive percutaneous plates group and the interlocking intramedullary nailing group) differences in the rates of excellent and good Johner-Wruh scores (RR 1.03, 95% CI 0.98–1.09, p = 0.19), and there was no statistically significant heterogeneity detected among these studies (Chi2 = 1.68, degrees of freedom [df] = 7, I2 = 0%, p = 0.98) (Figure2).
Among the eight studies that reported postoperative fracture healing times, five studies reported that the fracture healing time was significantly shorter in the minimally invasive percutaneous plates group than in the interlocking intramedullary nailing group (15-16,20),; the other three studies reported no significant differences in fracture healing times (14,17,19). Pooled data showed that the fracture healing time in the minimally invasive percutaneous plates group was significantly shorter than that in the interlocking intramedullary nailing group (standardized mean differences, SMD, -2.31, 95% CI, -3.59 – -1.04, p = 0.0004). Significant heterogeneity was detected among these studies (Chi2 = 34.88, df = 7, I2 = 80%, p<0.00001).
The reoperation rates did not differ significantly between the minimally invasive percutaneous plates and interlocking intramedullary nailing groups (RR 0.15, 95% CI, 0.02–1.24, p = 0.08). No significant heterogeneity was detected among these studies (Chi2 = 0.12, df = 1, I2 = 0%, p = 0.73).
The infection/osteomyelitis rates and superficial infection rates did not differ significantly between the minimally invasive percutaneous plates and interlocking intramedullary nailing groups (RR 0.51, 95% CI, 0.11–2.28, p = 0.38 and RR 1.16, 95% CI, 0.50–2.66, p = 0.73, respectively). There was also no significant heterogeneity detected among these studies (Chi2 = 0.46, df = 2, I2 = 0%, p = 0.79 and Chi2 = 1.85, df = 4, I2 = 0%, p = 0.76, respectively).
Three studies reported delayed union (15-16,20). The minimally invasive percutaneous plates group had a significantly lower likelihood of delayed union compared to the interlocking intramedullary nailing group (RR 0.28, 95% CI, 0.08–0.97, p = 0.04). Three additional studies reported nonunion (18,23-24). Pooled data showed that the nonunion rate differed significantly between the minimally invasive percutaneous plates and interlocking intramedullary nailing groups (RR 0.75, 95% CI 0.17–3.29, p = 0.70). No statistically significant heterogeneity was detected among these studies (Chi2 = 2.54, df = 2, I2 = 21%, p = 0.28 and Chi2 = 1.53, df = 2, I2 = 0%, p = 0.47, respectively).
The rates of internal fixation loosening or breakage did not differ significantly between the minimally invasive percutaneous plates group and the interlocking intramedullary nailing group (RR 0.65, 95% CI 0.24–1.74, p = 0.40). Moreover, no significant heterogeneity was detected among these studies (Chi2 = 1.53, df = 5, I2 = 0%, p = 0.91).
Eight studies (14,16-17,19), reported on pain, and two studies (15,18) reported on limited ankle mobility after the rehabilitation treatment. Pooled data showed that the minimally invasive percutaneous plates group had a lower rate of pain than the interlocking intramedullary nailing group; moreover, the limited ankle mobility rates did not differ significantly between the two groups (RR 0.38, 95% CI 0.19–0.75, p = 0.005 and RR 2.07, 95% CI 0.56–7.66, p = 0.28, respectively). There was also no statistically significant heterogeneity detected among these studies (Chi2 = 4.33, df = 7, I2 = 0%, p = 0.74 and Chi2 = 0.36, df = 1, I2 = 0%, p = 0.55, respectively).
Publication bias was assessed by comparing the standardized mean differences of fracture healing time, and substantial asymmetry (Figure3) was found; note that a number of studies may be missing from the lower right-hand corner of the plot.
DISCUSSIONTibial shaft fractures are the most common diaphyseal fractures in adults. The traditional open reduction and internal fixation of tibial fractures often requires extensive dissection that may lead to tissue devitalization, creating an environment that is less favorable to union and increasing the risk of infection as a result of blood supply disruption (25). Closed intramedullary nailing is still considered a gold standard treatment for long bone diaphyseal fractures. However, the procedure has a tendency to result in angular malunion and anterior knee pain problems when used to treat tibial fractures. Narrow medullary canals can impede nailing, and repeated reaming through this bone can cause significant thermal injury to the shaft (26). The minimally invasive percutaneous plate method has become more popular with the development of locking compression plating (LCP) (27). Through a small skin incision, the plate is tunneled extraperiosteally along the medial aspect of the tibia and fixed with head locking screws. The purpose of this meta-analysis and systematic review was to summarize the existing evidence in order to determine the safety and efficacy of the minimally invasive percutaneous plating method compared with the interlocking intramedullary nailing method. Although the evidence quality is low, the most important finding of this study is that minimally invasive percutaneous plating could shorten fracture healing times and decrease the rates of postoperative delayed union and pain compared with interlocking intramedullary nailing for tibial shaft fracture fixation. However, no significant differences were observed between the two groups in terms of the functional recovery score, rate of reoperation, or complications (e.g., infection/osteomyelitis, superficial infection, nonunion, internal fixation loosening or breakage, and limited ankle mobility).
Minimally invasive percutaneous plates and interlocking intramedullary nailing are prominent examples of biological internal fixation. Differing from conventional stable internal fixation, these approaches reduce the incidence of extended traumatic and iatrogenic necrosis by avoiding exposure of the fracture site and balancing stability and biology (28). Minimal surgical trauma and flexible fixation allow prompt healing when the blood supply to bone is maintained or can be restored early. Both methods have yielded mostly good to excellent functional recovery scores (7,29). The results of this meta-analysis did not reveal any between-group differences in the rates of excellent or good Johner-Wruh scores.
Although this study demonstrated that minimally invasive percutaneous plates could shorten fracture healing times for tibial shaft fracture fixation compared with interlocking intramedullary nailing, the assessment of publication bias indicated a moderate asymmetry. We included eight studies that reported fracture healing time, and these studies were randomized controlled trials, which are less susceptible to selection bias (30), and strictly adhered to the inclusion criteria. We found no significant differences between the eight studies regarding the participants, interventions, or outcome measures (14-17,19-20,22-23). Regarding the study types, one study (15) was a multicenter trial, and the others were single-center trials. Five studies had Jadad scores of two (15-17,20,23), two studies had scores of one (14,19), and the last study had a score of three (22). Statistically significant heterogeneity was detected among these subgroup analyses (Chi2 = 33.38, df = 6, I2 = 82%, p<0.00001 and Chi2 = 21.61, df = 4, I2 = 81%, p = 0.0002, single-center trials and trials with Jadad scores of two, respectively). Five studies reported that the fracture healing time was significantly shorter in the minimally invasive percutaneous plates group compared to the interlocking intramedullary nailing group (15-16,20,22-23). The other three studies reported no significant differences in fracture healing times (14,17,19). The funnel plot of the pooled data showed that a number of studies might be missing from the lower right-hand corner of the plot. Thus, low-quality evidence suggests that minimally invasive percutaneous plates could shorten fracture healing time compared with interlocking intramedullary nailing for tibial shaft fracture fixation.
The surgical treatment of displaced distal tibia fractures yields reliable results with either plate or nail fixation. Tibial nails would be associated with more knee pain, and plates would be associated with pain from implant prominence (31). Based on the data presented above, minimally invasive percutaneous plates could decrease the rates of pain and delayed union compared with interlocking intramedullary nailing for tibial shaft fracture fixation. In addition, no significant differences were observed between the two groups in terms of reoperation and other complications.
This meta-analysis has a number of limitations. First, in this systematic review, only one study randomized the patients to the treatment groups. The lack of appropriate methodology, including the lack of allocation concealment, blinding, and possible confounding factors, which can lead to over-reporting of the treatment effect, and selection or allocation biases, likely affected the study results (32). Thus, all conclusions should be carefully interpreted. Second, the funnel plot suggests a moderate publication bias that is mainly attributable to the absence of small negative studies.
Overall, there is insufficient evidence to draw definitive conclusions on the effects of minimally invasive percutaneous plates versus interlocking intramedullary nailing for tibial shaft fractures in adults. Low-quality evidence suggests that the use of minimally invasive percutaneous plates can shorten fracture healing times and decrease the postoperative delayed union rate and pain level compared with interlocking intramedullary nailing for tibial shaft fracture fixation. The evidence also suggests that there are no significant between-group differences in terms of the functional recovery score, rate of reoperation, and other complications (e.g., infection/osteomyelitis, superficial infection, nonunion, internal fixation loosening or breakage and limited ankle mobility). Further research entailing high-quality randomized controlled, multicenter trials is required to address key clinical questions regarding the effects of using minimally invasive percutaneous plates versus interlocking intramedullary nailing in the treatment of tibial shaft fractures in adults.
AUTHOR CONTRIBUTIONSAll authors assisted in the study design. He GC and Wang HS contributed equally to this work and should be considered co-first authors. All authors participated in the data interpretation, manuscript preparation, and critical revision.
No potential conflict of interest was reported.