Stress affects surgeons both during training and during professional activity.
OBJECTIVESTo compare stress levels affecting surgical residents during the simulated initial assessment and management in the Advanced Trauma Life Support practical exam vs initial assessment and management of trauma patients in the emergency room.
METHODEighteen surgical residents were evaluated under basal conditions, during the Advanced Trauma Life Support simulation, and during emergency room initial care. Heart rate, systolic arterial pressure, and diastolic arterial pressure were measured. The Student t test was used to test for differences between means, with statistical significance declared when P < .05.
RESULTSHeart rate and systolic arterial pressure were increased at the beginning and at the end of Advanced Trauma Life Support simulation and emergency room initial care. diastolic arterial pressure was only increased at the end of the Advanced Trauma Life Support simulation. Comparing values obtained during the Advanced Trauma Life Support simulation with those obtained during emergency room initial care, heart rate and systolic arterial pressure were significantly higher during the Advanced Trauma Life Support simulation both at the beginning and end of the test events. However, diastolic arterial pressure was only significantly higher for Advanced Trauma Life Support simulation compared emergency room at the end of the procedures. These results suggest that the simulation in the practical exam portion of the Advanced Trauma Life Support course is more stressful for the resident surgeon than is the actual initial assessment and care of trauma patients in an emergency room.
Comparar os níveis de stress que afetam os residentes de cirurgia durante a avaliação inicial simulada nos cursos Advanced Trauma Life Support versus a avaliação do trauma do paciente na sala de emergência.
MÉTODOSDezoito residentes em cirurgia foram avaliados em condições basais no curso de Advanced Trauma Life Support e na sala de emergência. Foram medidas a freqüência cardíaca, pressões arterial sistólica e diastólica.
ESTATÍSTICASTeste t do Estudante. Significantemente p<0.05.
RESULTADOSNo início da avaliação no Advanced Trauma Life Support, a freqüência cardíaca e pressão arterial sistólica foram mais altas do que (e pressão arterial diastólica foi similar a) os valores basais respectivos; no começo da avaliação na sala de emergência foram observadas respostas similares. No fim da avaliação no Advanced Trauma Life Support e na sala de emergência, os valores de freqüência cardíaca, pressão arterial sistólica e pressão arterial diastólica foram maiores do que no começo, exceto que a pressão arterial diastólica não variou significantemente durante a avaliação inicial na sala de emergência. Comparando os dois procedimentos, observa-se que o Advanced Trauma Life Support produziu elevações significativamente maiores de freqüência cardíaca e pressão sistólica tanto no inicio quanto no final dos respectivos procedimentos. Esses resultados sugerem que a avaliação inicial simulada no curso Advanced Trauma Life Support é mais estressante para o cirurgião do que no cuidado inicial de pacientes com trauma na sala de emergência.
In physiological terms, stress is defined as a set of adaptive reactions developed by the individual undergoing an aggression, stimulation, or effort. Thus, stimuli that cause pain, anger, or fear provoke a reaction of fight or flight and are associated with a state of stress.1 Initially, these stimuli provoke an increase in sympathetic activity that causes an increase in heart rate and arterial blood pressure. Stress, which has been called the disease of the 20th century,2 is classified as a disease by the World Health Organization (code F 43.9 ICD 10, 1997),3 and it is considered a possible factor in the development or worsening of cardiovascular diseases.4,5 During their training, physicians are exposed to frequent stressful situations, such as the admission examination for residency and performance of surgeries and emergency care.6
Furthermore, a high rate of mental diseases, alcoholism, drug abuse, and matrimonial problems has been reported for physicians.7–9 It is recognized that resident physicians, both in surgery as in other specialties, are constantly under stress that is usually evaluated through qualitative variables such as nights on duty, sleep disorders, exhaustion, alcohol or drug abuse, fatigue, low performance, and altered general behavior.10,11 A study comparing stress of medical teams with that of professional aviation teams emphasizes that physicians, contrary to aviation pilots, tend to deny the effect of stress and fatigue on their performance.11 Several recent studies on stress among physicians and medical residents have used heart rate and arterial blood pressure measurements as stress evaluation parameters.12–16
The Advanced Trauma Life Support (ATLS) course, which has been internationally adopted for teaching/learning on traumatized patient care, is administered over 2 days to physicians, and it has contributed to improved trauma care and outcome.17,18
The ATLS course consists of theoretical and practical lectures. To evaluate the cognitive and trauma management skills, 2 examinations are performed: a theoretical exam in the form of tests, and a practical exam using a trauma mannequin. The practical exam consists of the initial assessment and care of a simulated trauma patient and is based on an Objective Structured Clinical Examination (OSCE) for evaluation of the clinical performance of the student.19–21 The student performs the procedures of this care with the help of a nurse, under the supervision of an instructor. During the care, unforeseen situations are created that require quick and precise identification and solution, which are typical stress-generating occurrences.
Although the ATLS course is based on pedagogic fundamentals, the stress level it generates for students has not yet been quantified. The purpose of the present study was to quantify the stress level that affects the physician during the practical exam portion of the ATLS course in comparison to during initial trauma patient care in the admission room of the ER of a teaching hospital.
MATERIALS AND METHODSIn September 2000, 18 second-year surgical residents of the Department of Surgery were studied during rotational training in the Emergency Surgery Service (ESS) of the Hospital das Clínicas, Faculty of Medicine, University of São Paulo.
The study was approved by the Institutional Ethics Committee and was performed in accordance with the established guidelines on the treatment of human subjects. The heart rate (HR) and arterial blood pressure (AP) of each resident were initially measured under basal conditions (B) during the normal working period of the residents in the ESS, but in the absence of any emergency situation. The same group of 18 residents was evaluated in these 3 different situations.
Thereafter, these parameters were measured during simulated initial assessment and care in the ATLS practical exam portion (ATLS simulation) and during the initial assessment and care of a traumatized patient performed by the residents in the emergency room (ER initial care).
The HR was recorded continuously by means of a chronometer (Polar Vantage NVTM, Finland) with the sensor attached to the thorax of the resident during the entire evaluation period. Basal HR was recorded during 3 minutes under basal conditions. The ER HR and ATLS HR were recorded during the entire period spent in the care of 1 patient in the ER and in the period spent with the ATLS simulation, respectively. In order to measure the HR, the chronometer was started immediately before the beginning and stopped immediately after the end of the test event. The arterial pressure (AP) was measured using a manual sphygmomanometer (Novametric, Becton & Dickson) under basal conditions, immediately before and immediately after the ER initial care and the ATLS simulation. The same instrument, as well as the same standardized procedures, were used by the same researcher for all measurements in the 3 situations—basal condition, ER initial care, and ATLS simulation.
During patient care in the emergency room, patients under cardiopulmonary arrest, where either mechanical maneuvers or emergency thoracotomy were required, were not included in the study. Patients with nonsevere trauma were not included. Also, patients requiring external cardiac compression or emergency room thoracotomy during ER initial patient care were not included.
The ATLS practical exam included simulated cases of severe brain injury, open or blunt thorax trauma, cardiac tamponade, abdominal trauma, burn injury, and hypovolemic and neurogenic shock. The ATLS simulation was performed by the surgical resident with the help of a nurse, under continuous instructor observation. No other person, for example a simulated family member, was allowed to participate.
The data obtained are expressed as mean ± standard deviation. Statistical analysis of the results were carried out using the Student t test. Values of P < .05 were considered statistically significant.
RESULTSThe mean time period required for the ER initial care procedures was 30 minutes, for the ATLS simulation was 15 minutes.
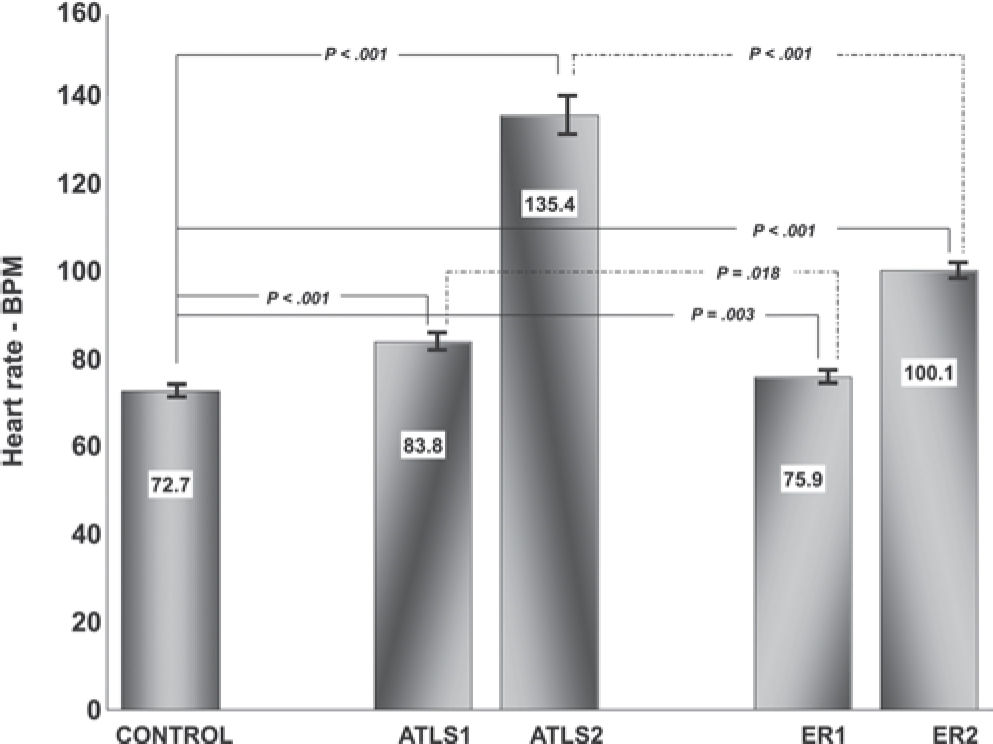
Values obtained for basal HR (HR-B) resulted from the mean of 3-minute recordings. Basal values of systolic (SAP-B) and diastolic (DAP-B) arterial pressures resulted from the mean of 3 measurements. The mean HR values of the 3 initial and final minutes of the ATLS simulation and ER initial care were taken to represent respectively the initial and final HR of the ATLS and ER test events. Figures 1 and 2 show HR and AP (SAP and DAP), respectively, measured under basal conditions (CONTROL), at the beginning and at the end of the ATLS (ATLS1, ATLS2) simulation and ER (ER1, ER2) initial care.
Fig. 1 displays the effects of ATLS simulation and ER initial care on HR. At the beginning of the ATLS simulation, HR was increased over basal values, and it increased further at the end of the simulation. Similarly, for ER care, HR increased over the basal rate at the beginning, and at the end of the procedure. When the 2 procedures were compared, ATLS induced more tachycardia than ER initial care, both at the beginning and at the end of the respective procedures.
Fig. 2 displays the corresponding results for arterial pressure. Systolic pressure displayed a pattern which was entirely similar to that of heart rate: it increased at the start and at the end of both procedures; it was significantly higher for ATLS vs. ER care, both at the beginning and the end of respective procedures. In contrast, diastolic arterial pressure displayed a very different response. It only increased at the end of the ATLS simulation, all other values remaining at basal conditions.
DISCUSSIONStress is a reaction by an individual facing a threatening stimulus to overcome or adapt to it, and it comprises 3 phases: alert (alarm), resistance, and exhaustion.7,8 Innumerable daily activities contain stimuli that are interpreted by an individual as a threat and generate stress.22 Stress is influenced by biographic factors, mental states, occupational activities, and personality characteristics, being usually expressed in terms of behavior patterns that affect accomplishments, competitiveness, feelings of urgency, dedication to work, and concern about deadlines.23,24 Thus, the level of stress is difficult to quantify.
When submitted to a stress evaluation, an individual is subjected to challenging tasks, such as performing arithmetic tests and public speaking with good performance to the public and to the evaluators. These challenges represent threats that provoke fear of disqualification and unforeseen reactions. Factors influencing the result of stress evaluation include individual characteristics and the method employed. The individual characteristics comprise age, gender, cultural differences, and personality traits.15,25 Some evaluation methods use questionnaires that quantify subjective characteristics by means of scoring.26 Other frequently used methods for stress evaluation are based on variables derived from cardiovascular reactivity such as HR, SAP, and DAP. Cardiovascular reactivity can be defined as an alteration in a relevant variable, such as arterial blood pressure, observed between a basal condition and conditions such as physical or mental strain, psychomotor activity, social evaluation, and other threats. In a specific study15 HR and arterial blood pressure variations caused by stress (speaking in public) were used to analyze the effects of individual characteristics (personality, hostility, gender) on the cardiovascular reactivity. Each individual participating in that study performed an oral presentation evaluated by the professor and colleagues. The results revealed that each participating individual exhibited a specific cardiovascular reactivity, which was higher in males, more elevated in hostile indivuduals, and did not reveal influences of other personal traits. In our study, with the aim of maintaining the homogeneity of the study group, only individuals of the same age group, same gender, and similar level of knowledge of trauma patient care were included. The group comprised male residents of surgery during their rotational training stage in the Emergency Surgical Service of the Institution. All tests measurements where taken on all participants to minimize possible influences of individual characteristics on the results of the study.
The level of difficulty of the simulated emergency care in the ATLS practical test, although not quantified, is uniform. However, the level of difficulty of emergency care procedures performed in the emergency room is variable, depending on diverse patient conditions such as trauma severity and complexity, degree of organ dysfunction, etc. In order to limit these variations, the time period for the emergency care of each patient was limited to the completion of the basic procedures required for emergency care, thus excluding the care of patients with non-severe trauma. The result was a test period with a mean of 30 minutes. Furthermore, 2 special procedures, external thoracic compression and emergency room thoracotomy, were excluded from this emergency care to avoid physical exertion that could affect the stress level and the measured parameters.
The fact that while performing the ATLS simulation the surgical resident was continuously under the observation/evaluation by the instructor who would decide in favor or not of his passing the test may represent a stress-generating stimulus.33 During ER initial care, the resident was not performing an evaluation test that would be decisive for his approval. Rather, the resident surgeon is under direct supervision/evaluation by the assistant surgeon as part of the resident's global performance in the surgical residency program. These factors could have resulted in a greater stress level during the ATLS simulation. The stress-generating potential of qualification tests, which could result in greater stress than that experienced by the professional while performing his/her work tasks that require the same level of knowledge/experience, has not been clearly evaluated in the reviewed literature.
The use of variations in heart rate and arterial blood pressure, which are components of cardiovascular reactivity, as the foundation of this method of evaluating the level of stress in the individuals in this study was based in the assumption that said components of cardiovascular reactivity adequately indicate the variation of stress. Various reports present substantial data to support this assumption. The parameters of cardiovascular reactivity most frequently used to represent the level of stress are HR, SBP, and DBP, which can easily be measured and expressed numerically.12,25 In this context, Melhado et al.12 quantified stress of pilots and aircraft crew using measurements of HR and AP under resting conditions (on a day off), as well as during various conditions of stress (pre-flight, take off, mid-cruise, approaching, and landing), and demonstrated significant increases of BP and HR during in-flight operations, especially during take-off and landing, which are considered more stressful periods.12 In another study, the alterations of HR and BP in response to stress caused by a mathematical test, compared to values under resting conditions, were used in the evaluation of the effect of a medication for arterial hypertension treatment. The results showed a reduction of BP in resting conditions as well as in stressful situations following treatment.26 Alterations of AP, HR, cardiac index reactivity, and vascular resistance index in response to mental stress (mathematical tests, speaking in public, etc.) were used to evaluate the effects of oral contraceptives on CVR in women who were smokers versus women who were nonsmokers.16 Other studies offer support for using HR and AP in the evaluation of the effects of stress.13,14,29 In general, it is thought that all kinds of stress can increase BP and HR, at least temporally.12,13
Several studies investigated the value of ATLS course, including the usefulness of the mannequin for the evaluation of residents’ management skills,30 its adequacy regarding the preparation of professionals of different levels for trauma care,31 the improvements that have occurred comparing the 1993 and 1997 versions,32and the durability of the cognitive and management skills learned through the ATLS course.20 The validity and importance of the OSCE, which is based on the use of standardized simulated patients in the ATLS course for evaluation of clinical performance of the students has also been emphasized.20,21,31
According to cognitive theories, stress levels depend less on the real risk of the stimulus than on the risk or threat as evaluated by the individual, whose ability to overcome the threat involves self-confidence, self-esteem, and self-image. In the alarm phase, the adrenergic response predominates, with immediate cardiovascular reactivity and motor reactions of fight or flight. The individual may decide to face the situation that generates anxiety, to avoid it and flee, which generates fear and depression, or even to ignore the threat, if he decides there is no risk. At the end of the alarm phase and the beginning of the resistance phase to the stressor challenge, cognitive-affective reactions and memory functions, involving personality, culture, and experience come into play, determining the decision taken to face the situation.7,8,33
In the ER initial care events of this study, the resident faced the challenge of caring for the critical patient, applying in practice the acquired theoretical knowledge associated with the resident's limited practical experience. The main threat faced by the resident in ER initial care is the risk of failure that may even lead to the death of the patient. In the ATLS simulation, the risk of failure is the threat of disqualification from the care of patients.
The results of the present study indicate that both heart rate and systolic arterial increased during ATLS simulation and ER initial care, from start to finish. Overall, ER initial care and the ATLS simulation represented effective, non-neutral stimuli that affected HR and BP. Accordingly, both the initial and final values of these variables (with the exception of the initial DAP) were higher in the ATLS simulation than in the ER initial care event, suggesting that the ATLS simulation had a higher potential to cause anxiety and stress than actual ER initial care. Although it is accepted that great stress may depress cognitive activity,33,34 the possible impact of the stress generated during the ATLS practical exam on the surgeon's learning process was not in the focus of this study and remains to be determined.
In conclusion, the results of the present study suggest that simulated initial assessment and care of a trauma patient in the practical exam of the ATLS course generates a higher level of stress in the surgeon than that usually generated by the actual initial assessment and care of trauma patients in the ER. More studies are warranted to clearly determine the factors of this finding.