A 46-year-old white woman presented to the clinic in September 2009 with intermittent abdominal epigastric pain accompanied by nausea, heartburn and frequent crises of asthma and cough for one year. Her past medical history revealed obesity-related arthropathy and a lumbar discal hernia with chronic NSAID use and no history of smoking. She underwent laparoscopic Roux-en-Y gastric bypass (RYGB) in September 2004 for morbid obesity (body mass index (BMI) 41.02 kg/m2) to construct a vertically oriented proximal gastric pouch, with a 120-cm jejunal Roux limb and jejunojejunostomy 50 cm beyond the ligament of Treitz (Figure1A-E). The gastric pouch was 3.5 cm, and the manually performed gastrojejunostomy was 13 mm, as verified by routine endoscopy one year after the operation (Figure 2A). A routine pre-operative upper endoscopy prior to the RYGB was normal. Two years after the RYGB, she was also submitted to laparoscopic adhesiolysis for small bowel obstruction. In September 2009, her weight decreased to 75.6 kg (166.3 lbs), which corresponded to a BMI of 26.79 (28% weight loss). Abdominal ultrasound and computed tomography ruled out any pancreatic or hepatobiliary disease. As the patient's symptoms did not improve despite extended trials of antacids and double doses of proton-pump inhibitors for over a year, investigations with 24-h esophageal pH monitoring (24-h pH testing) and manometry were conducted. A new upper endoscopy post-RYGB revealed a patent gastrojejunostomy (Figure 2A) in addition to grade B Los Angeles reflux esophagitis, with 10-mm longitudinal mucosal breaks (Figure 2B) and no signs of eosinophilic esophagitis. There was no evidence of hiatal herniation or Barrett's esophagus. Based on a 24-h pH test performed prior to fundoplication, the DeMeester score was 67.8 mmHg, with acid reflux occurring greater than 10% of the time both in supine (42.3%) and upright (16.9%) positions. The DeMeester reflux score was 67.8 (normal <14.72, 95th percentile). Manometry showed a lower esophageal sphincter pressure (LES) of 9 mmHg (normal range from 14.3 to 34.5 mmHg), and the contraction amplitude of the proximal and middle region was greater than 30 mmHg (50.6 mmHg). A biopsy showed grade 2 esophagitis. The upper gastrointestinal (GI) series revealed proper emptying of the gastric pouch but free gastroesophageal reflux disease (GERD). Therefore, the management of intractable postoperative reflux was performed with a laparoscopic 360° fundoplication to reinforce the lower esophageal sphincter by wrapping the excluded stomach around the lowest portion of the esophagus. This technique has not been previously described. Hiatal dissection and repair were performed, and the crura were approximated with three interrupted 2.0 polypropylene sutures. The excluded stomach was carefully isolated and used to construct the fundoplication, and the short gastric vessels were divided using the harmonic scalpel from the inferior pole of the spleen to the superior aspect of the excluded stomach. A loose, short 3-cm wrap was constructed, with assessment of the z-line (Figure 1C) performed under endoscopic guidance (Figure 1D). A 32-Fr intra-esophageal bougie was also used to calibrate the wrap. The excluded stomach (approximately 6 cm) was passed behind the esophagus, and the anterior and posterior excluded stomach lips were sutured together with three interrupted 3.0 polypropylene sutures (Figure 1E). The muscular wall of the anterior esophagus was incorporated in the sutures while carefully avoiding injury to the anterior vagus nerve. The fundoplication was not anchored to the crura. Reflux symptoms were scored using the Visick classification and a validated GERD questionnaire published elsewhere (1) before and after fundoplication (six months post-operation). There was marked improvement of preoperative symptoms and well-being in the post-operatory period (change in Visick classification from 3 to 1 and change in reflux symptoms score from 33 to 2). The patient tolerated the operation with no complications and experienced successful resolution of GERD symptoms. She was discharged on postoperative day two, tolerating a liquid diet without reflux or dysphagia. We were able to compare 24-h pH testing and manometry pre- and post-operatively. The erosion near the gastrojejunostomy (Figure 2C) healed after the surgery. She continues to be asymptomatic without reflux or dysphagia six months later.
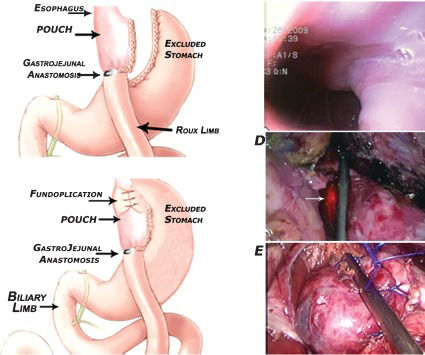
The proposed technique: A - Surgical anatomy post-RYGB. B - Surgical anatomy post-fundoplication. The LES was reinforced by wrapping the excluded stomach around the lowest portion of the esophagus. C - Endoscopic view of the 3.5-cm pouch and the 13-mm GJ. D - Endoscopic-guided fundoplication delimiting the z-line (arrow shows transillumination with the endoscope). E - Final result of the 360° short, floppy fundoplication. Abbreviations: RYGB – Roux-en-Y gastric bypass; LES – lower esophageal sphincter; GJ – gastrojejunostomy.
Pre - and intraoperative endoscopic view during laparoscopic fundoplication post-RYGB for obesity. A– Patent GJ. Transillumination of the jejunum with the laparoscope can be observed. B - Grade B Los Angeles reflux esophagitis (10-mm longitudinal mucosal breaks). C – Erosion in the pouch near the GJ. Abbreviation: GJ – gastrojejunostomy.
To our knowledge, this is the first described case of abdominal anti-reflux surgery (ARS) performed by laparoscopy in the late postoperative period following bariatric surgery. Bypass provides excellent long-term control of GERD symptoms and has the additional benefit of weight loss (2). Despite optimized medical therapy as the mainstay treatment, GERD continues in patients after undergoing surgery for morbid obesity. Up to 11-22% of patients who undergo successful RYGB operations will continue to complain of GERD symptoms postoperatively (1,3). RYGB was previously suggested (4) to accomplish both weight reduction and resolution of GERD similar to Roux-en-Y biliary diversion. Therefore, RYGB operations may not provide a definitive solution for GERD in all patients. Because bariatric surgery has only been conducted for the last 50 years and patients undergoing operations for morbid obesity are usually young, it is unclear what long-term effects GERD will have on this population. Patients with a BMI greater than 40 with reflux should undergo a bariatric procedure, particularly if they have gastroparesis (5). Those with BMI 30-39.9 requesting treatment for GERD can be offered a laparoscopic fundoplication, with outcome similar to that in patients who are within the normal weight range (6). The only surgical procedure described for persistent reflux similar to our case was a conventional 270° Belsey Mark IV ARS following open RYGB (7). Similarly, neither the short 6-cm gastric pouch nor adhesions from the previous operation were a contraindication for the fundoplication. RYGB successfully reduces GERD symptoms by (a) diverting bile away from the esophagus along the Roux limb, (b) decreasing acid production in the gastric pouch, (c) limiting the amount of acid reflux, (d) promoting weight loss, and (e) decreasing abdominal pressure over the LES and esophageal hiatus. BMI does not appear to influence the clinical outcome following laparoscopic anti-reflux surgery (6). Currently, endoluminal full-thickness gastroplication is experimental and indicated for overweight patients with mild reflux disease. (8) Endoscopic approaches were considered inadequate for this patient. Adhesions from the previous operation did not unduly hinder the dissection. This is why the previous RYGB did not prevent laparoscopic ARS similar to Nissen fundoplication, except that the excluded stomach was used instead. Furthermore, the good results obtained in our patient reinforce the suggested mechanism of action of a 360° fundoplication; namely, distension of the cardia is a major stimulus for transient lower esophageal sphincter relaxation (tLESR) (9). It is a vagus-mediated reflex caused by the stimulus of mechanoreceptors located at the gastroesophageal junction. The circular fixation of the top of the gastric cardia around the distal esophagus may further reduce the ability of the fundus to stretch or elongate, thereby decreasing episodes of tLESR. Thus, better results have been reported in a complete fundoplication compared with the Belsey Mark IV technique (10). Prospective clinical trials should investigate the long-term effects of the modified Nissen fundoplication to determine if it is a good surgical option for treating persistent reflux after RYGB operation.
No potential conflict of interest was reported.