Atherosclerosis is a chronic inflammatory disease that affects essentially all arterial beds including the aorta, coronaries, carotids, and peripheral arteries. It is the main cause of death in the western hemisphere, due to cardiovascular syndromes such as myocardial infarction, heart failure, and cerebrovascular accidents.
Very substantial economic and human resources have been used on treatments of its complications, including imaging studies, coronary bypass surgery, catheter interventions, pacemakers, and medical treatments. Treating complications, however, are remedial actions.
A better alternative is to prevent the development of atherosclerosis, or at least to identify patients who are at risk of acute events and intervene before they occur.
The aims of this review are to discuss the predictive value of traditional and emerging risk factors, as well as the role of noninvasive diagnostic methods for coronary atherosclerosis, including exercise stress test, echo stress test, duplex ultrasound, computed tomography, and magnetic resonance.
A combination of serum biomarkers and noninvasive approaches is of practical utility for identifying early disease. It is to be expected that future developments will soon perfect our ability to identify the vulnerable patient and allow a more individualized approach.
A aterosclerose é uma doença inflamatória crônica que afeta essencialmente todas as artérias incluindo a aorta, coronárias, carótidas e artérias periféricas. É a causa principal de morte no hemisfério ocidental, devido as síndromes cardiovasculares, tais como o infarto do miocárdio, insuficiência cardíaca e acidentes cerebrovasculares. Quantidades enormes de recursos económicos e humanos são usadas em tratamentos de suas complicações, inclusive estudos de imagem, cirurgias coronárias, intervenções com cateteres, marcapasso e tratamentos médicos. Tratar complicações, entretanto, são ações a posteriori. Uma alternativa melhor seria prevenir o desenvolvimento da aterosclerose, ou pelo menos identificar os pacientes que tenham risco de eventos agudos e intervir antes de sua ocorrência.
O objetivo desta revisão é discutir o valor prognóstico dos fatores de riscos tradicionais e emergentes, e o papel dos métodos diagnósticos não invasivos para a doença coronária - teste de esforço, eco estresse, ultra-sonografia dúplex, tomografia computadorizada e a ressonância magnética. A combinação de marcadores biológicos e de métodos não invasivos, é de grande utilidade na identificação precoce da doença aterosclerótica. Futuros desenvolvimentos logo aperfeiçoarão nossa capacidade de identificar o paciente vulnerável e nos permitir um manejo mais individualizado.
Atherosclerosis is a chronic inflammatory disease that affects essentially all arterial beds including the thoracic and abdominal aorta, coronary arteries, carotids, peripheral, renal and mesenteric arteries. It results from a complex interaction between genetic and environmental factors that causes the arterial wall to respond to inflammatory stimuli through the actions of endothelial cells, smooth muscle cells, inflammatory cells, and platelets.1 These produce a large variety of substances such as growth factors, cytokines, reactive oxygen species, enzymes, signaling factors that profoundly alter the arterial wall structure, and finally lead to the development of the atherosclerotic plaque.2–4 The plaque is composed of varying amounts of smooth muscle cells; monocyte-derived macrophages; T lymphocytes; cholesterol; cholesteryl esters; phospholipids; and extracellular connective tissue. This ensemble forms the extracellular matrix including collagen, proteoglycans, and the pericellular matrix formed by fibronectin and elastic fibers.5–7 The plaque eventually progresses to the point of obstructing the arterial lumen, reducing blood flow, and causing several clinical manifestations. A detailed description of plaque formation and evolution is beyond the scope of this article.
Atherosclerotic cardiovascular disease is the main cause of death in the western hemisphere, including in Brazil.8 For the last decades, the principal focus of treatment and investigation has been its complications, notably myocardial infarction, angina, sudden death, and heart failure. Very substantial economic and human resources, including imaging studies, catheterizations, coronary bypass surgery, catheter interventions, pacemakers, and medical treatments, have been used for the diagnosis and treatment of these complications. In spite of undeniable progress in all these areas with improved overall outcomes, treating complications of a disease is in fact a medical failure; we are acting after the events A better alternative would be to prevent the development of the basic disease, i.e., atherosclerosis, or at least to identify those patients who are at risk of an acute event and to intervene before damage occurs †for instance, ahead of the left ventricular dysfunction that follows a myocardial infarction.
Identifying causative factors of the primary disease is the fundamental principle of so-called primary prevention. The rational basis for the application of the principle lies in the ability to recognize individuals who are at risk for development of the disease, as well as those who are at risk for complications; the logical consequence is the customized use of effective therapeutic approaches.
In order to apply such a preventive approach, a basic knowledge of the nature of atherosclerosis is essential. Therefore, some pertinent features of atherosclerosis relevant to its prevention shall be highlighted.
First, atherosclerosis begins very early in life. In fact, in some instances the genetic determinants of atherosclerosis are present from the moment the ovum is fertilized by a spermatozoid, and the genes of the parents are mutually influenced, composing a new human being. However, this is the fate of a minority; it is estimated that only about 20% of cases of atherosclerosis are genetically determined.9,10 That atherosclerosis appears in infants, adolescents, and young adults, both male and females, blacks and whites, has been documented in several necropsy studies of young persons who died of violent death due to war wounds, accidents, suicides, or homicides.11–15 These individuals were asymptomatic, and their mean age was less than 30 years. In the Bogalusa study,13 the degree of atherosclerosis involvement in the aorta and the coronary arteries was directly proportional to the presence of classic risk factors. Thus, the development of atherosclerosis is an early phenomenon in humans although its clinical manifestation may only occur decades later.
Second, the development of atherosclerotic plaques begins in the arterial wall and progresses slowly in such way that for a long period of time the arterial lumen in not significantly affected; consequently blood flow may be normal even under conditions of increased oxygen demand, such as intense exercise. Hence no ischemic symptoms may occur. This was initially documented by Glagov et al16 and termed positive arterial remodeling; in the initial phases of plaque formation there is a thickening of the arterial wall and external expansion with maintenance of the lumen. In this phase, conventional coronary arteriography shows no luminal abnormalities or only arterial irregularities. For a certain time in the past, this finding was thought to indicate absence of atherosclerosis; we now know that is not so. Arterial remodeling explains the long asymptomatic period so often seen in patients with coronary artery disease.
Third, lesions that are not hemodynamically significant, e.g., those causing < 70% stenosis, may suddenly become unstable, suffer rupture, and cause partial or total occlusions precipitating an acute coronary crisis.17 Many factors may contribute to this phenomenon, including structural characteristics of the plaque, endothelial erosions, inflammation, and thrombosis.18 Therefore, having a plaque that is not flow-limiting does not necessary guarantee an event-free clinical course. This is corroborated by the finding that clinical coronary events are acute in two thirds of cases, while stable angina represents only one third. In addition, in 65% of acute coronary syndrome cases angiographic studies have documented previous lesions or the residual lesion in the culprit vessel which were less than 50%.19 The frequency of the destabilization phenomenon, as well as the fact that interventions such as coronary surgery or angioplasty are usually associated with higher complication rates than elective ones, highlights the importance of identifying patients with potentially unstable syndromes. Ideally all interventions should be elective.
Fourth, about 40% of patients in the fifth decade of their lives with documented coronary artery disease do not have classic risk factors.20 Therefore, on one hand, the presence of classic risk factors does confer a greater risk of atherosclerosis; on the other, their absence is no guarantee that the disease will not be present. More recent understanding of the pathophysiology of atherosclerosis has shed some light into this question; thus, the inclusion of inflammation, oxidative stress, endothelial dysfunction, and other novel risk factors may help to better judge the interaction among all risk factors and atherosclerosis.
Fifth, atherosclerosis is a systemic disease. The Framingham study21 showed that patients presenting myocardial infarction, cerebral vascular accident, heart failure, or peripheral vascular insufficiency as their first manifestation would, in the following 10 years, manifest disease in another vascular territory in proportions varying from 16% to 50%, both for men and women. In addition, secondary prevention studies with statins have systematically documented reductions of cardiac events, as well as reductions in stroke and intermittent claudication; this clinical observation makes biological sense since the basic pathophysiological mechanisms of atherosclerosis are the same, although regional variations are noted due to specific characteristics of the particular vascular beds. This feature of atherosclerosis makes it possible to analyze peripheral vessels, such as the carotid and brachial arteries, and draw meaningful inferences regarding what may occur in the coronary circulation, as has been shown for endothelial function22 and carotid intima-media thickness.23 Noninvasive vascular analysis has taken advantage of this fact, as will be discussed later.
So far, the most frequently used method to predict risk has been the Framingham score24,25 and the European risk score.26 These take into account the presence of classic risk factors, EKG findings, and pertinent clinical data. Although of great practical value, these systems are destined to predict risk, not the presence of disease in itself. In addition, since a considerable number of patients do not exhibit classic risk factors, this subset of individuals is not properly investigated. In addition, the presence of risk factors by itself does not mean that any given individual will develop the disease. Also, a long time lag between the documentation of a risk factor and the actual appearance of disease may occur; for instance, if the time lag is long, treating a patient for the presence of only 1 or 2 risk factors may indeed represent a significant decision problem. Hence, the search for methods of early detection of coronary disease may be justified. When the disease is detected in its early phases, a customized treatment may be proposed. But if no disease is present, the aggressive treatment of 1 risk factor may not be justified. Hence, an individualized approach should be aimed at, for; it would allow safer and eventually less costly treatments.
NONINVASIVE DETECTION OF ATHEROSCLEROSISClinical information is highly relevant for the recognition of atherosclerosis; thus, the typical history of angina, intermittent claudication, or a past coronary event, such as myocardial infarction, indicates with great probability the presence of the disease. The Framingham study27 established the validity of hypercholesterolemia, smoking, age, male sex, diabetes, obesity, sedentariness, and arterial hypertension, among others, as major determinants of future cardiovascular events, as to be later discussed. Diabetes in particular has received special recent attention,28 since its mere presence has been found to be as strong a predictor of events as a previous myocardial infarction. In parallel, the metabolic syndrome represented by insulin resistance, obesity, hypertension, and atherogenic dyslipidemia represents a major cause of atherosclerosis.29
Physical examination is very often entirely normal in atherosclerotic individuals, especially in the early phases of the disease. However, some findings, such as a carotid murmur or the absence of peripheral pulses, carry a strong predictive power.
Some specific laboratory data have predictive value for atherosclerosis development. Hypercholesterolemia, specifically elevated low-density lipoprotein, is the best known and also the most widely tested lipid abnormality in primary and secondary prevention studies.30 It is worth considering low-density lipoprotein heterogeneity. Small, dense low-density lipoprotein particles are more atherogenic than large, buoyant low-density lipoprotein particles.31 The oxidation of low-density lipoprotein also increases its atherogenicity. Low-density lipoprotein contains apolipoprotein (apo) B-100, which may be also atherogenic. Furthermore, some particles are larger and rich in triglycerides (large very-low-density lipoprotein), whereas others are smaller and rich in cholesteryl esters (small very-low-density lipoprotein, intermediate-density lipopoprotein). It is now known that remnant lipoproteins containing apo C-III are highly atherogenic, as is lipoprotein(a), another member of the apo B-100 group.32 Based on numerous large and well-designed clinical trials that followed thousands of patients for many years, it can be said that the benefits of lipid lowering therapy are now demonstrated beyond any reasonable doubt. These benefits extend to both men and women of all ages.30
Low levels of high-density lipoprotein are also recognized as an independent risk factor.33 We have shown that in healthy individuals in whom the only abnormality was a low level of high density lipoprotein, the endothelial-dependent arterial relaxation was significantly impaired and that this alteration could be reversed by niacin treatment.34 These individuals also had a decreased plasma clearance of chylomicron remnants; the two abnormalities facilitate atherosclerosis development and may explain the known elevated susceptibility for early atherosclerosis of patients with low levels of high-density lipoprotein.
Hypertriglyceridemia has also been analyzed. According to a meta-analysis of 17 prospective trials, hypertriglyceridemia is an independent risk factor for cardiovascular disease.35 The PROCAM study for instance found a significant relationship between hypertriglyceridemia and coronary artery disease risk, independent of low- and high-density lipoprotein levels.36
Remnant lipoproteins derived from chylomicrons and/or very low-density lipoprotein also promote atherogenesis and correlate especially with the progression of atherosclerosis.37 Both remnant cholesterol and remnant triglycerides were found to be increased in diabetic men and women compared with nondiabetics.38
We have also analyzed the triglycerides/high-density lipoprotein ratio in relation to the precocity of coronary artery disease detection in 495 patients with documented coronary artery disease.39 Taking triglycerides of 150 mg/dL and high-density lipoprotein of 40 mg/dL as normal values, a triglycerides/high density lipoprotein ratio of 3.75 was reckoned to be a normal value 39It was subsequently shown that values above 4.0 coincide with higher proportions of small low-density lipoprotein particles in human plasma,40 which have already been demonstrated to be particularly atherogenic. Although all lipid variables were associated with coronary artery disease, the strongest associations were with triglycerides and the triglycerides/HDL ratio above 3.75, especially in patients younger than 50 years of age. In addition, we found in 274 patients subjected to diagnostic coronary angiography that the extent of coronary disease evaluated through the Friesinger score41 best correlated with the triglycerides/high density lipoprotein ratio.42 Thus, a triglyceride/high density lipoprotein ratio > 4.0, not only correlates with precocity of coronary artery disease as clinically detected but also with more extensive coronary lesions. It may hence be a useful surrogate for atherosclerosis assessment.
Less commonly used, lipoprotein(a) may also be of value. Lipoprotein(a) is structurally similar to low density lipoprotein in protein and lipid composition.32 Retrospective case-control studies found a strong association between elevated lipoprotein(a) levels and coronary artery disease; however it should be noted that only 9 out of 13 prospective studies found lipoprotein(a) to be an independent risk factor for coronary artery disease. There is no clinical trial demonstrating that lowering lipoprotein(a) levels decreases coronary artery disease risk. Thus the value of lipoprotein(a) for atherosclerosis prediction remains uncertain.
NEW RISK FACTORS FOR ATHEROSCLEROSISThe inflammatory nature of atherosclerosis may be evidenced through easily measurable plasma components that can be, and have been proposed to reflect not only the presence of the disease itself, but also to indicate its clinical course, complications, and prognosis.43–50 High sensitivity C-reactive protein is the most used of these parameters. It has –additive value for predicting coronary artery disease risk beyond the classic risk factors.43 In prospective studies, healthy men and women with increased baseline levels of C-reactive protein were at increased risk for future coronary artery disease.44 Subclinical coronary calcification was also associated with increased C-reactive protein, in men and women45 and was significantly elevated in patients with coronary disease who died suddenly. It also correlates with immunohistochemical staining intensity and numbers of inflammatory cells in thin cap atheroma.46 Furthermore, one study reported that C-reactive protein is a risk factor that is independent of traditional risk factors, such as total cholesterol, high density lipoprotein cholesterol, age, smoking, body mass index, and blood pressure in women.47 A proof of concept argument can be the results of lipid-lowering trials in patients with recent acute coronary syndromes. In the PROVE-IT48 study, patients with a recent myocardial infarction were treated with either pravastatin or atorvastatin and followed up for a mean of 24 months; regardless the statin used. The reductions in recurrent myocardial infarction were greater when low-density lipoprotein < 70 mg/dL and C-reactive protein < 2 mg/L were achieved simultaneously by statin therapy than when those two values were above such limits. When low-density lipoprotein was <70 mg/dL but C-reactive protein >2 mg/L, or vice-versa, an intermediate reduction in recurrent myocardial infarction was observed. Thus lowering lipid levels and combating inflammation, both resulting from statin therapy, are comparably important for prevention of complications post acute coronary events.
A caveat regarding the routine use of C-reactive protein for risk prediction is warranted. C-reactive protein is a nonspecific marker of inflammatory diseases: it can be elevated in practically every inflammatory disease, such as rheumatic, chronic bacterial, or immunologic conditions. Nevertheless, the optional use of C-reactive protein to guide physicians in identifying patients without known cardiovascular disease who may be at higher risk than estimated by major risk factors alone was recently recommended by the American Heart Association.49 The rationale is that the additional information may guide the clinician in deciding for further evaluation, such as functional tests or even therapy.
Lipoprotein-associated phospholipase A2 has been studied. Lipoprotein-associated phospholipase A2 is an enzyme that catalyzes the hydrolysis of oxidized phospholipids, generating 2 bioactive products that can potentiate atherogenesis: lysophosphatidylcholine and nonesterified fatty acid moieties.3,4 Examining the association of lipoprotein-associated phospholipase A2 mass and activity with calcified coronary plaques in 266 cases of young adults and comparing to 266 controls, the authors of the Cardia study51 found that lipoprotein-associated phospholipase A2 was significantly higher in the cases than in the controls. They concluded that the enzyme is a useful marker for subclinical cardiovascular risk. Further studies are necessary, but lipoprotein-associated phospholipase A2 is a potential therapeutic target.
Homocysteine is the product of demethylation of methionine; remethylation and trans-sulfuration are critical steps in its degradation. Hyperhomocysteinemia is generally considered a contributing factor in systemic atherosclerosis, cerebrovascular disease, and peripheral vascular disease. Several case-control and cohort studies have linked hyperhomocysteinemia with coronary artery disease risk. In a Brazilian population of 236 patients, men and women, subjected to diagnostic coronary angiography, we recorded a number of significant points: (i) homocysteine levels were higher in those with than in those without coronary artery disease; (ii). multivariate analysis showed hyperhomocysteinemia to be an independent risk factor for coronary artery disease with an odds ratio of 2.48 (CI 95% 1.02-6.14); (iii) an inverse relationship between homocysteine levels and folic acid was observed; (iv) patients with more advanced coronary lesions as determined by the Friesinger method had a higher frequency of hyperhomocysteinemia.52 Our data are consistent with other studies, such as the Framingham Heart Study53 and the Atherosclerosis Risk in Communities (ARIC) study.54.
B-TYPE NATRIURETIC PEPTIDENatriuretic peptides are hormones involved in volume homeostasis and have been found to be increased in ventricular dysfunction. There are suggestions that they may have prognostic significance in apparently healthy persons. Thus, in 3,346 persons without heart failure included in the Framingham Heart Study, plasma B-type natriuretic peptide and N-terminal pro-atrial natriuretic peptide were examined regarding (a) the risk of death from any cause, (b) a first major cardiovascular event, (c) heart failure, (d) atrial fibrillation, (e) stroke or transient ischemic attack, and (f) coronary heart disease.55 Even adjusting for cardiovascular risk factors, each increment of one standard deviation in B-type natriuretic peptide levels was associated with a 27% increase in the risk of death (P < .009), a 28% increase in the risk of a first cardiovascular event (P < .03), and a 77% increase in the risk of heart failure (P < .001). The mean follow-up was 5.2 years. The investigators concluded that plasma B-type natriuretic peptide levels predict the risk of death and cardiovascular events independent of traditional risk factors.55,56 Further studies are needed to establish the true value of this parameters in terms of risk prediction in asymptomatic individuals.
SOLUBLE CD40 LIGANDThe CD40-CD40 ligand system is present in leukocytic and nonleukocytic cells, including endothelial and smooth-muscle cells and on activated platelets.57 The CD40 ligand also occurs as soluble CD40 ligand (sCD40L), which is proinflammatory for endothelial cells and promotes tissue factor expression on monocytes and endothelial cells. Evidence indicates that the CD40 ligand plays key roles in atherosclerosis development, progression, and complications, even in apparently healthy individuals. For instance, the Orbofiban in Patients with Unstable Coronary Syndromes—Thrombolysis In Myocardial Infarction-16 (OPUS-TIMI-16) found that elevated plasma levels of sCD40L identify patients at increased risk of death and recurrent myocardial infarction independent of other predictive variables, including troponin I and C-reactive protein.58 Additional investigation is warranted to define the practical role of soluble CD40 ligand in primary prevention.
FRAMINGHAM RISK SCOREThe Framingham risk score is certainly very popular and useful. It is a global risk score based on traditional risk factors such as age, sex, smoking, blood pressure, diabetes, arterial hypertension, and cholesterol values. According to the Framingham risk score, individuals are ranked into low-, intermediate-, and high-risk groups based on their chances of having events in 10 years. The low-risk group has less than 6% risk over 10 years, the intermediate-risk group, 6% to 20% risk over 10 years, and the high-risk group, equal to or higher than 20% risk over 10 years. Risk for the latter group is equivalent to those for patients with stable established coronary artery disease.59 Greenland et al,59 analyzed the North American adult population and estimated that 35% are in the low-risk group, 40% in the intermediate-risk group, and 25% in the high-risk group. This score system facilitates identification of patients at different risk levels and also has implications for counseling and treatment. The absence of any major risk factor identifies individuals at very low risk, while the traditionally major risk factors account for 50% to 80% of subsequent cardiovascular events in high-risk patients.60,61 The high-risk group—i.e., risk greater than 20% for 10 years—probably benefits from aggressive risk factor reduction such as a combination of healthy eating and exercise plus aggressive medical therapy, while patients at low risk require essentially advice regarding healthy lifestyles. However, the intermediate group represents the greatest challenge for treatment decisions and should always be evaluated carefully and individually.62
The European Risk Score25 is based on similar criteria and is therefore equivalent for practical purposes. A major limitation of this risk score system is that a significant number of individuals in the fifth and sixth decade of life with documented coronary artery disease, perhaps as many as 40%,20 do not exhibit the traditional risk factors. Accordingly, a modification to this scoring has recently been suggested aiming to improve coronary artery disease risk assessment in asymptomatic people. It is conceivable that the use of serum biomarkers, especially C-reactive protein and atherosclerosis imaging, including coronary calcium scoring or carotid ultrasound for intima-media thickness, may refine risk estimation.
DETECTION OF MYOCARDIAL ISCHEMIAThere are several ways to detect myocardial ischemia by noninvasive methods in addition to clinical data as mentioned before. Although several diseases, such as congenital coronary anomalies, myocardial hypertrophy, and tumors, can cause myocardial ischemia, by far the most common cause is atherosclerosis. Therefore, in susceptible patients, the detection of myocardial ischemia usually implies atherosclerosis as the underlying disease. Germane to this scenario is the premise by which any noninvasive test should be interpreted.
According to the Bayes’ theorem, the greater the prevalence of the disease in the population to which an individual belongs, the greater the validity of a positive test and likelihood that this is a true positive. Hence, in any population where there is a low likelihood of the condition being present, a positive result has limited value, being more likely a false positive.63
RESTING AND EXERCISE STRESS TESTINGResting EKG is of limited value for ischemia recognition, since more often than not, it is normal. However, some specific findings are of great significance, such as signs of previous myocardial infarction, ST depression, and T wave inversion.
Conversely, stress EKG testing, either pharmacological or exercise based, is of considerable value and has been extensively studied in different populations; specific criteria for test interpretation have been developed based on comparative evolutive data. It is noteworthy that the majority of positive stress tests are false positives in unselected asymptomatic people63 because of the low pre-test probability of disease. Hence, the absolute risk of cardiac events in these populations remains low; consequently, the routine use of exercise ECG testing in completely unselected asymptomatic populations is not recommended. In contrast, a positive exercise test in middle-aged men with several coronary risk factors has independent predictive power for major coronary events. On the other hand, even in the presence of risk factors, the predictive power of a positive test is not the same for women and young adults because disease prevalence is low.63
RESTING AND STRESS ECHOCARDIOGRAPHYMyocardial ischemia or infarction typically cause segmental myocardial dysfunction that can be detected by a 2-dimensional echocardiogram at rest. Areas of wall motion abnormalities, wall thinning, aneurysms, global ventricular dilation, increased ventricular volumes, and decreased ejection fraction can be indirect indicators of myocardial ischemia or necrosis. Given the ease with which an echocardiogram can be obtained, this method has considerable practical application in individual patients, especially those in whom exercise stress tests can not be performed.
Stress echocardiography is based on the principle that acute, induced myocardial ischemia leads to left ventricular dysynergy. It should be considered that the test adds costs and complexity to the exam. In a meta-analysis of 28 studies, the sensitivity and specificity of dobutamine stress echocardiography was 80% and 84%, respectively, for detection of coronary artery disease.64 In addition, there is only limited data supporting the use of stress echocardiography as a tool to assess the intermediate-risk patient.65 However, stress echocardiography can be of value in certain patients in the intermediate-risk category, such as women and the elderly. Additional studies are needed to define its role for elevating such patients to the high-risk category for primary prevention.
EXERCISE AND PHARMACOLOGICAL MYOCARDIAL PERFUSION IMAGINGMyocardial perfusion scintigraphy is one of the most useful, widely used, and reliable methods for noninvasive myocardial ischemia detection or elimination. It also has a unique position as a tool for myocardial viability analysis. Its sensitivity is about 95%, and its specificity reaches close to 90% in large series;66 its high negative predictive value of about 98% in asymptomatic individuals is of significant practical usefulness. Whether or not stress thallium scintigraphy can be a useful addition to exercise ECG testing for determining risk for major coronary events in intermediate-risk asymptomatic patients remains a critical question. Limited data suggest incremental value for this purpose in some populations, such as postmenopausal women and elderly men (age > 75 years) in whom the use of exercise ECG testing is of limited applicability. Recently, Lima et al67 reported stress SPECT results in 328 patients aged 74 years or older. Abnormal results were common, particularly in men, in patients with chest pain, and in those with resting or exercise ST-T abnormalities. Patients with normal perfusion images had an annual hard event rate of < 1.0% per year, while those with abnormal images had a corresponding annual rate of 14.3% per year.
Because few prognostic studies have included adequate numbers of asymptomatic people, data are scarce regarding the prognostic utility of noninvasive measures for the detection of myocardial ischemia in apparently asymptomatic people. With the exception of exercise ECG testing in asymptomatic men with increased cardiovascular risk profiles, few data exist to support the use of the noninvasive testing modalities.64
DIRECT DETECTION OF ATHEROSCLEROTIC PLAQUEDuplex ultrasoundDuplex ultrasound is widely applicable for the early detection of atherosclerosis in the noninvasive vascular laboratory. Its major advantages include the simplicity and general availability of the procedure. Examination of the carotid arteries to measure the intima-media thickness is used routinely, and evaluation of plaques and even estimates of the degree of obstruction also are performed on a regular basis. Although plaque diameter is readily measurable, the variable and complex 3-dimensional morphology of plaques68 produces a poor correlation with actual plaque size or volume. Semiquantitative approaches include averaging of plaque diameters; the number of segments with plaques in the common carotid artery, bulb, internal carotid artery, and external carotid artery; or plaque number. Intima-media thickness correlates well with the extent of coronary lesions, and furthermore, as intima-media thickness increases, cardiovascular event rates also increase.68,69 Thus, in the Kuopio Ischemic Heart Disease Risk Factor Study, myocardial infarction risk increased by 11% for each 0.1 mm increase in common carotid intima-media thickness.70
Measurement of the ankle-brachial index with a handheld continuous-wave Doppler instrument is an accurate way to diagnose peripheral arterial disease. This is important not only for identifying patients with peripheral arterial disease but also because they frequently have atherosclerosis in other arterial territories and hence may have increased frequency of myocardial infarction and stroke.71
Duplex ultrasound may also be used to assess brachial artery reactivity, and therefore, endothelial function.22,72 As shown by Celermajer et al,21 brachial artery reactivity accurately reflects coronary reactivity and therefore can be used as a surrogate marker of coronary endothelial function. Endothelial dysfunction actually precedes clinical manifestations of coronary artery disease, is a better prognostic indicator of events than coronary lesions themselves, is associated with several risk factors, and can be improved by the correction of many classic risk factors such as hypercholesterolemia and arterial hypertension.73 However, long-term studies of endothelial function are still necessary to prove its relationship to coronary atherosclerosis and its value as predictor of events in asymptomatic individuals.
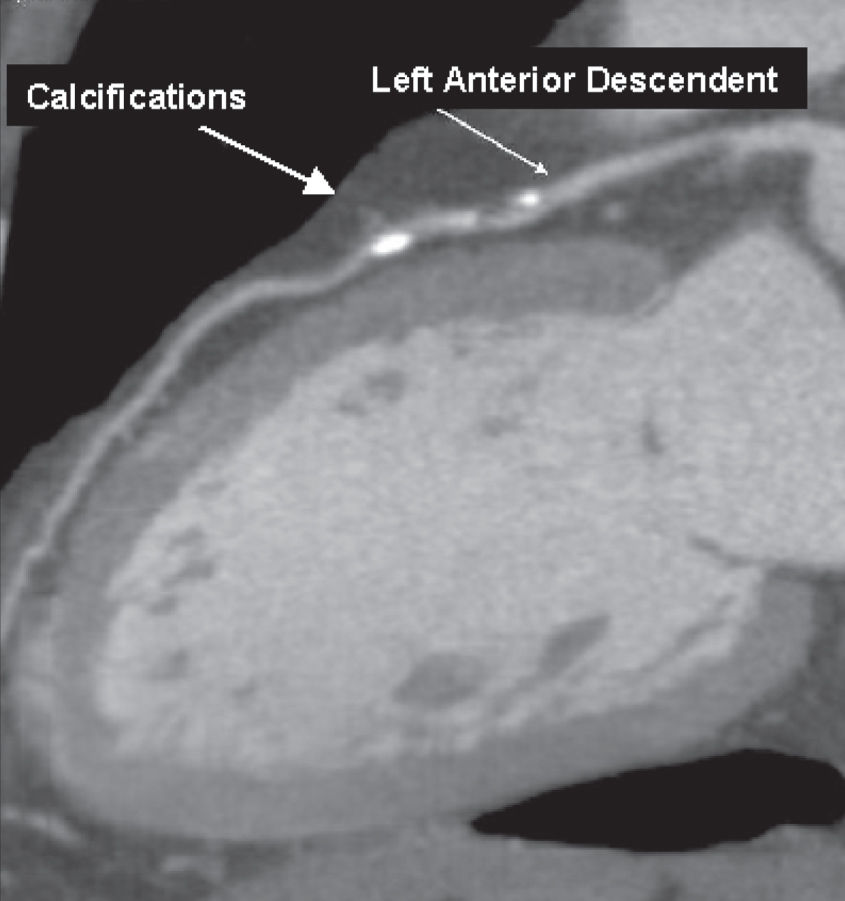
ULTRA FAST COMPUTED TOMOGRAPHY – DETECTION OF THE AMOUNT OF CALCIUMFast imaging is essential to overcome cardiac and respiratory motion artifacts; ultra fast computed tomography does just that. Only electron-beam computed tomography74 and fast-gated helical or spiral computed tomography75 can measure the amount or volume of calcium in blood vessels, although magnetic resonance imaging, x-ray angiography, and ultrasound can also identify calcified deposits in vessels. Atherosclerotic calcification may occur in early atherosclerotic lesions, it but is found more frequently and more extensively in advanced lesions.76 An association between coronary calcium and coronary artery disease has been documented;, there is also evidence that the amount of coronary calcium is a predictor of risk of coronary events.77 According to a meta-analysis of data in asymptomatic populations, a calcium score above the population median value was associated with an unadjusted odds ratio of 4.2 (95% confidence interval [CI] 1.6 to 11.3) for myocardial infarction or death.78 It is not certain, however, whether the predictive value of coronary calcification in high-risk subjects is superior to that of standard coronary risk factors79; given the cost and complexity of the test, this is a point of considerable practical interest. The additional benefit of using both coronary artery calcium scores plus the Framingham risk score was evaluated by Greenland et al80 in 1,461 asymptomatic, middle-aged (> 45 years) adults with at least 1 coronary risk factor; they were followed for 8.5 years after the computed tomography scan. A coronary artery calcium score > 300 was predictive of myocardial infarction or coronary death; (P < .001), compared with a score of zero. Moreover, coronary artery calcium scores were predictive of risk among patients with a Framingham risk score higher than 10% (P < .001) but not with a Framingham risk score lower than 10%, suggesting that high coronary artery calcium scores can modify the predicted risk obtained from Framingham risk score alone, especially among patients in the intermediate-risk category.79Figure 1 illustrates calcium scoring.
Ultra fast multislice computer tomography of coronary arteries. Calcification of coronary, score 9.8 Agatston,80 75th percentile for age and gender
Noninvasive coronary angiography is performed after the intravenous administration of iodinated contrast agent, with EKG synchronization and during breath holding to minimize motion artifacts. Multiplanar reformat, maximum intensity projection, volume rendering, or virtual angioscopy can be performed and aid in the diagnosis of coronary stenosis. The technique is improving rapidly, and the newer generation 64-slice multidetector computer tomography will further refine diagnostic capability. Sensitivities of 89% to 92% and specificities of 93% to 98% have been recently reported, after the exclusion of arteries considered to be of subdiagnostic image quality.81,82
Although the diagnostic accuracy of noninvasive angiography regarding the degree of stenosis is still a matter of concern, this method may be satisfactory and convenient after percutaneous or surgical revascularization. Indeed, some studies show good results in detecting total occlusions but rather low sensitivity and specificity for identifying in-stent restenosis or saphenous vein graft lesions.83,84
The detection of noncalcified atherosclerotic plaques prone to rupture by computed tomography has also been tried with promising results.85,86 However, multidetector computed tomography underestimates plaque burden when compared to intravascular ultrasound, probably due to lower spatial resolution, especially in distal segments.87 Long-term observations regarding the predictive value of multidetector computed tomography are not available because of its relatively recent development; however, given its noninvasive nature and overall diagnostic precision, progressive use can be anticipated in the near future.
MAGNETIC RESONANCE IMAGINGCardiac magnetic resonance imaging offers a unique, impressive range of information that has revolutionized the field of cardiac imaging. Through cardiac magnetic resonance, the dynamics of cardiac function can be appreciated in minute detail, and pathophysiological mechanisms became evident, forming the basis for clinical or surgical management of patients with known or suspected coronary artery disease. Cardiac magnetic resonance methods allow assessment of global and regional cardiac function, cardiac volumes, myocardial perfusion, cardiac valves, pericardium, myocardial viability, and proximal coronary anatomy, among others. Individually, these methods have shown promise as alternatives to the established tools for the noninvasive detection of coronary stenosis and myocardial infarction.88–90 A unique advantage of cardiac magnetic resonance imaging is that several of its methods can be combined in a single scanning session.
CONTRAST-ENHANCED MAGNETIC RESONANCE ANGIOGRAPHYNoninvasive, accurate detection of coronary stenosis has been a challenge for quite some time. Recently, contrast-enhanced coronary magnetic resonance angiography was found to have high specificity and sensitivity compared with x-ray angiography for the detection of luminal narrowing > 50% in humans.89 Technical advances in processing speed and new contrast agents91,92 are partly responsible for the rapid evolution of the field. Imaging of large vessels, such as the aorta, carotid, and femoral arteries, is now routine and replaces conventional angiography, with unquestionable advantages. In addition, contrast-enhanced magnetic resonance angiography methodology has been proposed as a technique for the assessment of coronary anomalies, patency of bypass grafts, post-stent improvement in coronary flow, and coronary in-stent restenosis.93–97
HIGH-RESOLUTION MRI FOR PLAQUE CHARACTERIZATIONPlaque destabilization is responsible for acute coronary syndromes and is a complex phenomenon characterized by inflammation, thrombosis, apoptosis, hemorrhage, and endothelial dysfunction that occur mostly in lipid-rich plaques. Magnetic resonance can differentiate plaque components with reasonable accuracy, based on biophysical and biochemical parameters such as chemical composition, water content, physical state, molecular motion, or diffusion.57 Thus far, magnetic resonance plaque characterization of the carotid arteries and aorta has proven to be very sensitive and specific as compared to that of the coronary arteries.98,99 A crucial ultimate goal of cardiovascular noninvasive imaging is to have reliable technology for plaque characterization of the coronary arteries.56
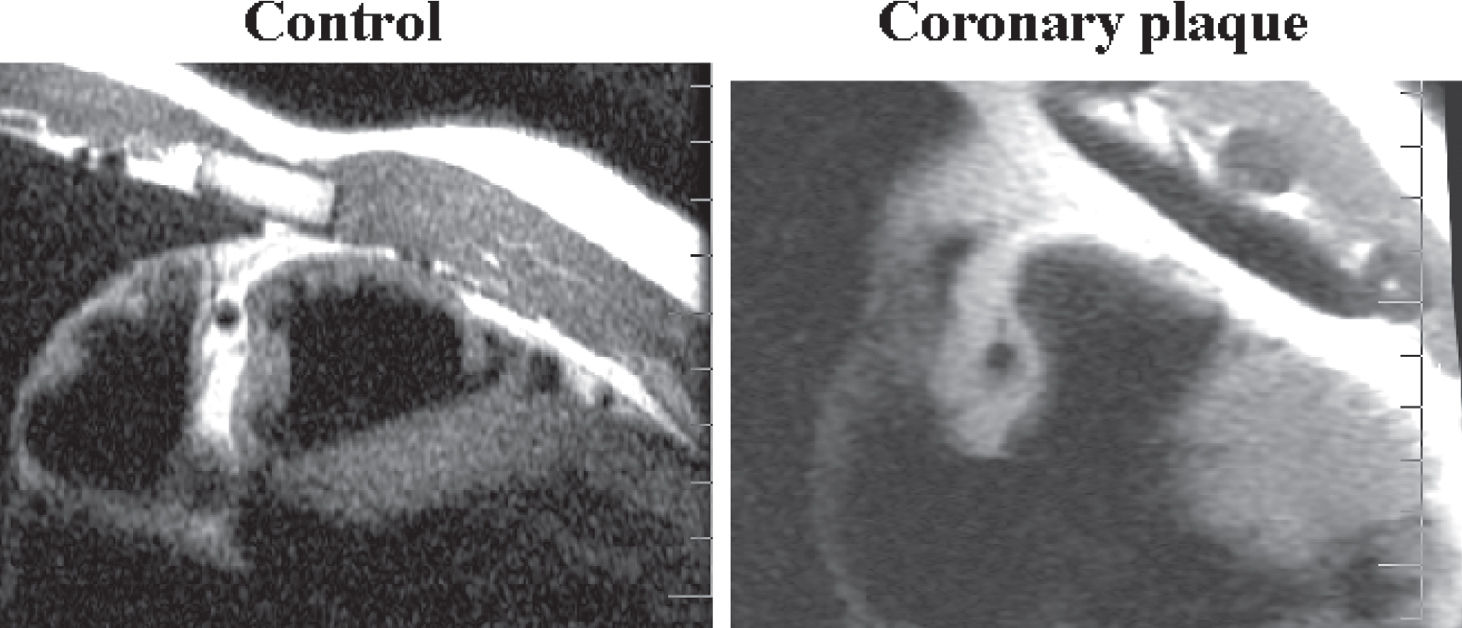
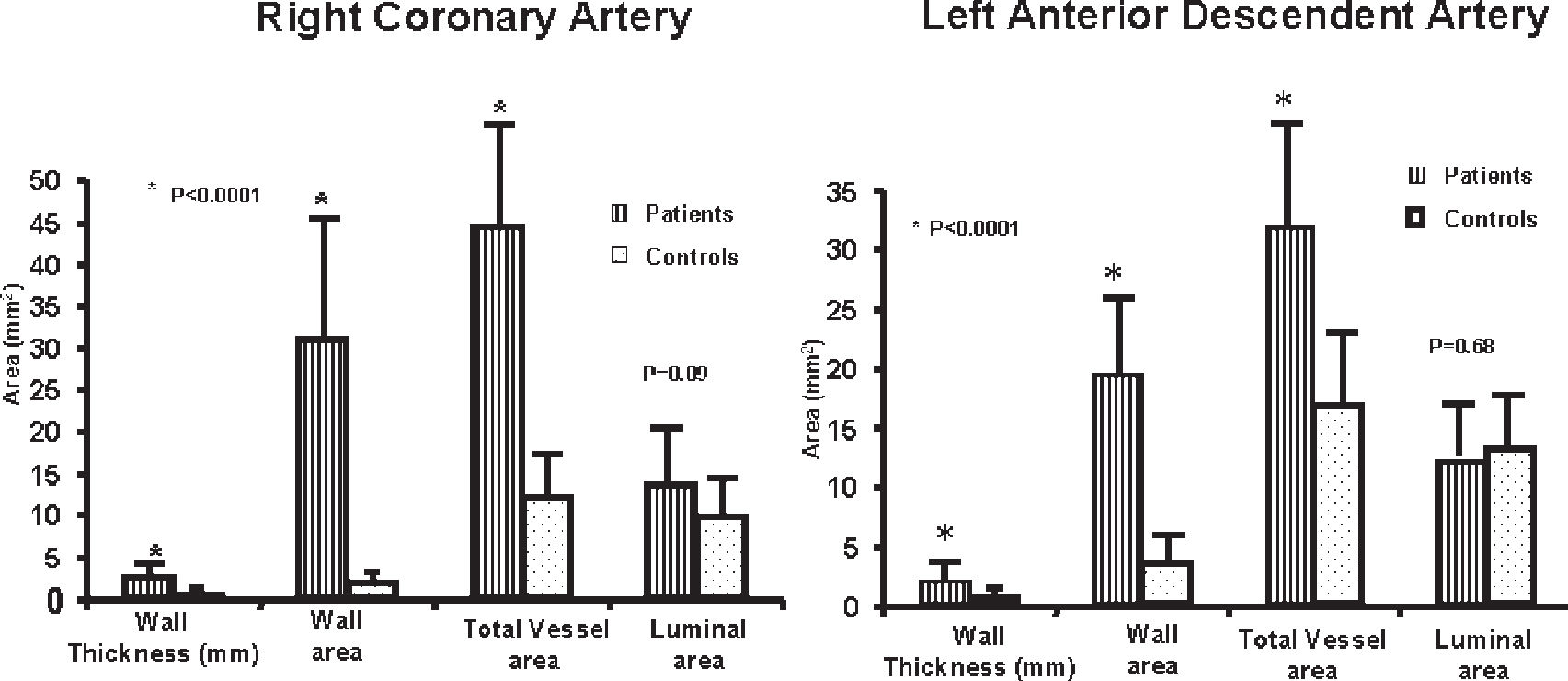
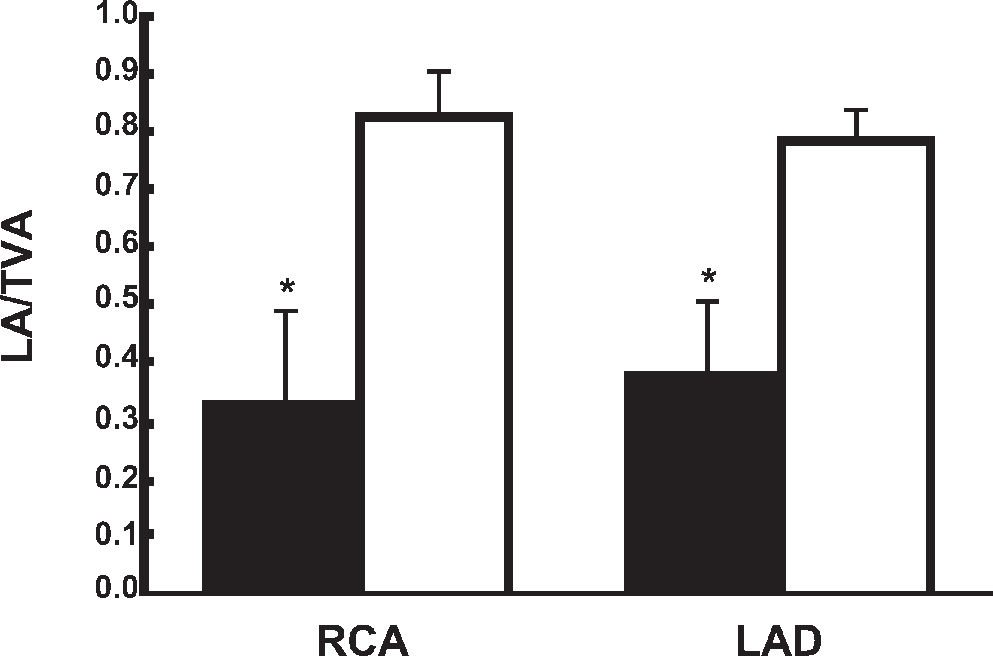
Magnetic resonance imaging is a new noninvasive method that can detect morphologic characteristics of coronary arteries in vivo in animals and humans and also allows the identification of arterial remodeling in experimental atherosclerosis.100–103 We have already detected by magnetic resonance imaging coronary vessel wall modifications, e.g., increases in wall thickness, vessel wall area, and total vessel area in patients with coronary artery disease compared to normal controls.104 Interestingly, the luminal area was preserved in these patients in spite of the presence of large plaque volumes (Figure 2). Thus, magnetic resonance imaging to determine the luminal area/total vessel area ratio is a noninvasive method for detecting coronary vessel wall modifications including remodeling and for clearly differentiating patients with coronary artery disease from healthy subjects despite a similar lumen (Figures 3a, 3b).
Magnetic resonance of coronary arteries. Observe the increment of wall thickness and total vessel diameter of diseased vessel, a positive remodeling (right) compared to the control (left)104
Magnetic resonance of coronary arteries. Positive remodeling of coronary arteries indicated by increased wall thickness, wall area, and total vessel area with preservation of luminal area104
The relationship between risk factors and the occurrence of atherosclerosis is unpredictable and variable. In general, it takes decades for risk factors to cause significant vessel obstruction and clinical syndromes. Although risk factors, and especially the clustering of 2 or more, will eventually lead to obstructive lesions, the time course of such events in any individual patient is far from predictable. Thus, some patients may have a slow clinical course over decades and finally present with typical effort angina due to flow-limiting stenosis, often affecting all coronary beds. On the other extreme, patients may present with acute coronary syndromes in their forties and fifties, with coronary lesions of moderate severity or even minor stenosis, due to destabilization of the plaque. Clearly then two different challenges must be faced if prevention of lesions on one hand and prevention of events on the other are to be achieved. Prevention of atherosclerosis development, the so-called primary prevention, is based on the recognition of risk factors and early identification of incipient lesions. For those individuals, the approaches for early detection of atherosclerosis were examined above. They need long-term preventive measures directed at controlling risk factors, such as recommendations for healthy lifestyles and eventually drug therapy, such as statins, aspirin, antihypertensives, or treatment for diabetes.
Identifying the unstable patient is an entirely different matter, because not everyone who has a plaque will soon have an event; conversely patients with even minor plaques may suffer acute events. For instance, analyzing 516 patients who were on a waiting list for coronary surgery, we observed that the most powerful indicators of complications in this period were angina, heart failure, and high triglyceride levels; coronary anatomy by itself was not a good predictor.105 This suggests that functional status, more than anatomy, is a fundamental determinant of prognosis.
In this regard, the challenge is to identify the unstable patient. Although inflammatory markers, coronary calcium scoring, magnetic resonance imaging, optical coherence tomography, angioscopic studies, thermography studies, and vascular ultrasonography have all been studied regarding their ability to identify such vulnerable patients, this still remains an elusive goal.106 Identification of “soft” plaques by noninvasive means would be critical. In this respect, magnetic resonance imaging is likely to have the greatest potential. Plaque analysis based on nanoparticles or gadolinium-tagged molecular imaging is being tested in noncoronary vascular beds, such as the distal aorta.107,108 Given the velocity of recent developments in this field, it may not be unrealistic to say we are in the dawn of the molecular plaque imaging era, which hopefully will improve our predictive ability.
These future developments will perfect our ability to identify not only incipient atherosclerosis but the vulnerable patient as well; then a more individualized approach for patient care can be adopted.