To analyze the clinical results of a partial vertebrectomy with titanium mesh implantation and pedicle screw fixation using a posterior approach to reconstruct the spine in the treatment of thoracolumbar burst fractures.
METHOD:From January 2006 to August 2008, 20 patients with severe thoracolumbar fractures were treated.For vertebral bodies associated with one injured intervertebral disk, subtotal vertebrectomy surgery and single-segment fusion were performed. For vertebral bodies with two injured adjacent intervertebral disks, partial vertebrectomy surgery and two-segment fusion were performed.
RESULTS:All 20 patients were followed up for 12 to 24 months (average of 18 months). There were no complications such as wound infections, hemopneumothorax or abdominal infections in any of the patients. The neurological status of all of the patients was improved by at least one American Spinal Injury Association grade by the last follow-up. The anterior vertebral body height was an average of 50.77% before surgery, 88.51% after surgery and 87.86% at the last follow up; the sagittal Cobb angle was improved, on average, from 26.15° to 5.39° and was 5.90° at the last follow up. The percentage of spinal stenosis was improved, on average, from 26.07% to 4.93%° and was 6.15% at the last follow up. There were significant differences in the anterior vertebral body height pre- and post-surgery and in the sagittal Cobb angle and the percentage of spinal stenosis (p<0) in all patients.
CONCLUSIONS:This surgical procedure is simple and can accomplish decompression, reduction, fixation and fusion of the spine in one stage. This approach could be widely used in orthopedics.
In clinical settings, thoracolumbar three-column fractures are typically treated using an anterior-posterior combined approach. The reduction and fixation of thoracolumbar fractures is achieved through the posterior approach, whereas the decompression and fusion of the spine are completed using the anterior approach. However, the main drawbacks of the anterior-posterior combined approach include the major trauma associated with these procedures, longer operation time, increased blood loss and a high incidence of complications. Thus, we used a one-stage surgery that included partial vertebrectomy, titanium mesh implantation and pedicle screw fixation using the posterior approach; this approach produced good clinical results.
MATERIALS AND METHODSStudy populationAfter obtaining institutional ethics committee approval (Third Hospital of Hebei Medical University, Shijiazhuang, China) and written informed consent from the patients, twenty patients with serious thoracolumbar burst fractures that were treated using the one-stage posterior approach in a prospective study. There were 13 males and 7 females, and the average age was 38 years, ranging from 20 years to 56 years. There were 5 cases caused by car accident injuries, 9 cases caused by falling from a height and 6 cases caused by other mechanisms. The spinal level distribution of the cases was as follows: T3 vertebra, 1 case; T4 vertebra, 4 cases; T5 vertebra, 3 cases; T7 vertebra, 1 case; T11 vertebra, 6 cases; T12 vertebra, 1 case; L1 vertebra, 1 case; and L2 vertebra, 2 cases. All of the thoracic vertebrae injuries were associated with pulmonary contusions and pleural effusions, 2 cases of which were associated with calcaneus fractures, 1 case was associated with scapula fracture and 1 case was associated with an odontoid fracture. Only 1 of the 3 lumbar vertebrae cases was associated with a pelvic fracture. According to the American Spinal Injury Association (ASIA) neurological function classification, there were 4 A grade cases, 9 B grade cases, 5 C grade cases and 2 D grade cases. The average time from the day of the injury to the day of the operation was 13 days (range 3-23 days). Computed tomography (CT) examination of each patient showed that all three columns were injured and the corresponding MRI examination showed abnormal signals in the spinal cord.
Surgical procedureThe patient was placed in a prone position on the operating table. After successful anesthesia, routine surgical antiseptic techniques were performed and sterile towels were placed. Then, the incision markers for the injured vertebra were made using C-Arm fluoroscopy. A mid-line incision was made to expose the vertebral lamina, the articular process and the base of the transverse process of the injured vertebra. The exposure was expanded to the vertebral lamina, the articular process and the base of the transverse process of adjacent vertebra in cases associated with fracture and dislocation. Four pedicle screws were placed for single fractures and fracture-dislocation injuries required 8 pedicle screws. A total laminectomy was then performed, retaining the least-injured facet. If both of the adjacent intervertebral disks were injured, the facets of the upper and lower parts of the injured vertebra were removed. Each fracture was reduced and fixed temporarily using a pedicle screw system. The decompression was performed through the side that sustained serious damage; the medial wall of the pedicle was removed to expose the dura mater and venous plexus bleeding was stopped with bipolar coagulation. Subsequently, the dura mater and nerve roots were gently and slowly pulled to the opposite side; it was important not to pull too tightly on the nerve structures. Light activity of the nerve roots was kept intact and the range was not more than 1 mm; the stretching of the dura mater was performed more carefully above the L1 level. Parts of the injured vertebra were removed using ring drilling (1.0 cm) along the medial wall of the pedicle at a 30° angle; vertebral cancellous bone was further removed using a curettage curette to expose the upper and lower discs. Thereafter, fragments of broken discs and the bone that had fallen into the spinal column were completely removed using a cutter knife. Nerve root canal decompression in the region adjacent to the injured vertebra increases the activity of the nerve root, which can facilitate the implantation of the titanium mesh. Titanium mesh of a suitable diameter was selected after measurement with a caliper, filled with cancellous bone from the injured vertebra and implanted into the middle of the two adjacent vertebral bodies from a posterolateral direction under distraction while the spinal cord and the nerve roots were retracted using a nerve dissector. The distance from the titanium mesh to the posterior margin of the vertebral bodies was greater than 0.5 cm. Then, the pedicle screws were connected with the rod and fixed permanently by applying axial pressure after satisfactory positioning of the titanium mesh was confirmed using C-arm fluoroscopy. Bone grafting was performed on the posterior lateral aspect of the injured vertebra. Lastly, a drainage tube was placed and the wound was carefully closed with sutures (Figures1, 2).
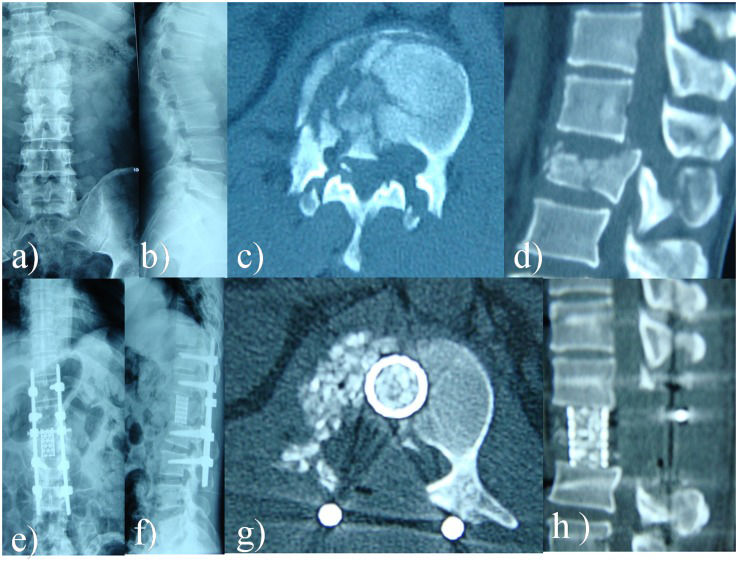
Typical case one: a) and b) the preoperative X-ray shows an L1 fracture and dislocation; c) and d) preoperative CT scan of the L1 vertebral body; e) and f) the postoperative X-ray of L1 vertebral body shows that the fracture achieved good reduction; g) and h) postoperative CT scan of the L1 vertebral body.
Typical case two: a) and b) the preoperative X-ray shows the L1 fractures; c) and d) preoperative CT scan of the L1 vertebral body; e) the preoperative MRI examination shows spinal cord compression; f) and g) the postoperative X-ray of the L1 body shows that the fracture achieved good reduction; h) postoperative CT scan of the L1 vertebral body.
The drainage tube was removed after 48 hours and routine postoperative antibiotics were administered for 72 hours. Low back muscle activity was restricted for 2 weeks after the surgery under the guidance of the doctors and activities away from the bed while wearing a thoracolumbar brace were allowed 3 weeks later.
Follow-up and assessment methodsThe recovery of neurological function was assessed using ASIA score standards. The quality of reduction was assessed by postoperative x-ray and the measurement of Cobb angle and the anterior vertebral body height. The degree of spinal canal decompression was assessed by evaluating the percentage of spinal stenosis, which was estimated as previously described (1). Briefly, “The least sagittal diameter of the spinal canal at the level of injury (referred to as, a, below) was measured on the CT scan. The normal diameter of the spinal canal was estimated by calculating the average of the respective measurements at the adjacent unaffected levels above and below the injury (referred to as, b, below). The percentage of spinal canal stenosis was calculated by using the formula (a/b×100)”. Bone graft fusion was assessed based on postoperative three-dimensional CT. The data were analyzed using SPSS 13.0 for Windows (SPSS Inc., Chicago, IL, USA). The one-sample Kolmogorov-Smirnov test was applied to analyze the continuous variables. For normally distributed data, probability values were calculated based on the analysis of variance. The Friedman test was applied to compare the anterior vertebral body height, sagittal Cobb angle and percentage of spinal stenosis. A p-value <0.05 was considered statistically significant.
RESULTSThe surgery time for the 20 patients ranged from 120 to 270 minutes (averaged 195 minutes) and the total blood loss ranged from 1200 to 4000 ml (averaged 2800 ml). Postoperative cerebrospinal fluid leakage occurred in only one patient who recovered after symptomatic treatment. The vertebral structure was returned to normal according to the following parameters: the anterior vertebral body height was, on average, 50.77% before surgery and 88.51% after surgery and it was 87.86% at the last follow up; the sagittal Cobb angle was improved, on average, from 26.15° to 5.39° and it was 5.90° at the last follow up; the percentage of spinal stenosis was improved, on average, from 26.07% to 4.93% and it was 6.15% at the last follow up. There was a significant difference between the pre- and post-surgery values of the anterior vertebral body height, sagittal Cobb angle and the percentage of spinal stenosis in all patients (p<0) (Table1). There were no large vessel injury complications or increased neurological symptoms in any of the 20 patients. There was also no loosening or breaking of the internal fixation on X-ray at the last follow-up. There was no obvious recovery of neurological function in the 4 cases with ASIA grade A. The ASIA score in 13 cases improved, including 7 cases that improved from B to C, 4 cases that improved from C to D and 2 cases that improved from D to E (Table2).
Pre- and postoperative radiographic measurement of the injured segment in the 20 patients.
| Before surgery | After surgery | Final follow-up | |
|---|---|---|---|
| Anterior vertebral body height (%) | 50.77±7.26 | 88.51±6.38 | 87.86±6.24 |
| Sagittal Cobb's angle (°) Percentage of spinal stenosis (%) | 26.15±3.74 26.07±2.84 | 5.39±2.66 4.93±2.02 | 5.90±2.61 6.15±2.20 |
(mean ±SD).
The concept of thoracolumbar burst fracture was originally proposed by Holdsworth (2) in 1970. The main features of this fracture are a wedge-shaped compression of the anterior column, middle column fractures and bone fragments of the posterior margin extruded into the spinal canal. These fractures are unstable and are often associated with neurological dysfunction.
The goal of surgical treatment is to decompress the neural elements, restore the vertebral height, correct the angular deformity and stabilize the spinal column (3). In recent years, several developments, such as the establishment of Denis' spinal three-column theory (4), the popularity of CT three-dimensional reconstruction and magnetic resonance imaging (MRI) examinations and the development of spinal fixation devices, have led to the extensive implementation of various surgical methods for thoracolumbar burst fractures. However, there has been no definitive evidence to help surgeons determine the optimal surgical treatment (5,6). Currently, there are three main commonly used surgical approaches: the posterior approach, the anterior approach and the posterior-anterior combined approach. The posterior approach of open reduction and internal fixation is used to restore vertebral body height and to partially reduce bone fragments through the stretching and distraction of the posterior longitudinal ligament and the posterior annulus fibrosus, which can also produce indirect decompression. However, this approach is associated with several disadvantages. 1) The indirect reduction is inaccurate and cannot ensure the anatomical reduction of the bone fragments that entered the spinal canal, resulting in an incomplete decompression of the spinal cord. 2) Although laminectomy helps in decompression, it may also further increase the instability of the spine. 3) Posterior pedicle screw fixation alone does not effectively maintain vertebral height, which could be responsible for the high failure rate of internal fixation that is observed even in cases without laminectomy. Additionally, the loss of vertebral height can result in the subsequent development of kyphosis. 4) The effect of posterolateral bone grafting fusion is inaccurate. 5) For old fractures (more than 2 weeks), posterior vertebral body reduction is very difficult (7,8). Moreover, even if the serious collapse of thoracolumbar fractures is associated with satisfactory reduction through the posterior approach, the “shell vertebral body” phenomenon (9) can still occur and cause secondary vertebral kyphosis. Secondary vertebral kyphosis usually requires the anterior approach correction, which significantly increases the physical and economic burden for patients (10,11).
Through the anterior approach alone, compression can be implemented under direct vision to achieve complete decompression of the spinal canal, which produces little disturbance for the already injured or edematous spinal cord and cauda equina. However, this approach cannot solve such problems, such as, a severely damaged vertebral posterior column structure, facet twisting, severe vertebral collapse, dural tears and epidural hematomas. Some doctors have adopted the combined anterior and posterior approach to increase the success rate; however, this increases the trauma and consequent surgical morbidity (4,12). Thus, we used single-stage posterior corpectomy, interbody fusion with titanium mesh and transpedicle screw fixation for this type of injury. This approach combines the advantages of the anterior only approach and the posterior only approach and reduces the trauma and complications that may arise with the combined approach (13,14); however, this approach is not suitable for patients with severe osteoporosis or those in poor physical condition. Nonetheless, this method allows for the completion of decompression, reduction, fusion and fixation in one stage and has the following advantages: less trauma, shorter operative time, less blood loss and total decompression. It is especially suited for patients with poor lung function who cannot tolerate a thoracotomy.
During the operation, the spine must be temporarily stabilized before decompression to avoid secondary spinal cord injury caused by instability. The decompression is generally started from the seriously injured side of the injury. In addition, the decompression of the vertebra associated with laminar fractures should be performed carefully, as cauda equina herniation can result from a fractured lamina.
Although there is controversy regarding the fusion of segments (15–17), we suggest the following: for patients with a single disk injury and small portions of vertebral body resection, a single-level fusion should be performed for the maximum restoration of the activities of the adjacent segments; for patients with an injury to two adjacent discs, corpectomy and double-segment fusion may be more effective.
In conclusion, the present study allows us to propose that posterior corpectomy and stability reconstruction with titanic mesh autografting and pedicle screw fixation in one stage is an effective technique for unstable thoracolumbar burst fractures. However, it is important to consider some key limitations of this study, such as the small number of patients and the lack of a control group.
AUTHOR CONTRIBUTIONSLi H conceived and designed the study. Liu Y wrote the manuscript and participated in data management. Dong T and Zhang Y performed the statistical analysis. Li G, Li H and Liu Y performed the surgical operations. All authors read and approved the final version of the manuscript.
No potential conflict of interest was reported.