Chronic kidney disease is a major public health problem worldwide. In Brazil, approximately 100,000 patients (January 2012) receive renal replacement therapy. Nevertheless, data on dialysis incidence in the Brazilian population are scarce. This study aims to analyze the incidence of patients starting dialysis therapy in São Paulo City, the largest Brazilian metropolis.
METHODThis cohort study analyzed data from 9,994 patients starting hemodialysis or peritoneal dialysis funded by the Brazilian Public Health System during a 5-year period (2007–2011). Patient data for this study (recorded as electronic files) were obtained from the São Paulo City's Dialysis Regulatory Bureau, which regulates the allocation of patients requiring dialytic therapy.
RESULTSThe dialysis incidence rates were 178, 174, 170, 185 and 188 per million population for the years 2007, 2008, 2009, 2010 and 2011, respectively. The incidence rates increased with age. Hypertension and diabetes were the main etiologies diagnosed. Hemodialysis was the chosen dialysis modality in the majority of patients (92.6%), whereas the percentage of patients referred for peritoneal dialysis decreased from 10.1% to 5.5%.
CONCLUSIONThe incidence of patients starting renal replacement therapy from 2007–2011 in São Paulo was stable but higher than the projected incidence for the entire country. The authors emphasize the need for further studies of the incidence of dialysis in the Brazilian population and for the creation of a Brazilian registry of dialysis patients, which would be a valuable tool for developing healthcare policies and renal replacement therapy strategies.
Chronic kidney disease (CKD) is characterized by a progressive decline in renal function; it is currently classified into 5 stages based on the presence of kidney damage and/or the reduced estimated glomerular filtration rate (1). CKD stage 5, which is defined as a glomerular filtration rate of <15 ml/min/1.73 m2 and also known as end-stage renal disease (ESRD), reflects a kidney failure stage in which most patients will require renal replacement therapy ([RRT], i.e., dialysis or kidney transplantation) to sustain life. Both RRT modalities are associated with significant morbidity and mortality risks and represent major health care costs. Thus, worldwide, CKD is considered a major public health problem that contributes to the global burden of noncommunicable diseases (2).
Worldwide, more than 2 million patients require RRT; the majority are located in the United States of America (USA), where nearly 0.5 million patients are treated with dialysis or transplantation for kidney failure (3). During the last 2 decades, the annual growth in the number of dialysis patients was 6-12% in many developed countries, and the growth rate in several developing countries was even higher (2). However, even this growth rate likely represents far less than the actual need for RRT (4) because in many countries, particularly in developing countries, there is a large number of undiagnosed CKD patients, and access to RRT remains unaffordable for some members of the affected population (2–5). Thus, CKD has often been described as a rising global epidemic (6). In fact, many reports have described the rising prevalence of CKD in the general population. However, recent data point toward a slight reduction in the CKD prevalence in South Korea (7), and the incidence rates of patients starting RRT have been reported as decreasing in the USA in recent years (8,9) and stabilizing in Europe (10).
Brazil is the fifth-largest country in the world, both by population (192.3 million inhabitants in 2011) and area (8,514,877 km2). Brazil has the third-largest dialysis population worldwide, and together with the USA, Japan, Italy and Germany, it accounts for 56% of all RRT patients (3,11). In January 2012, there were 91,314 patients undergoing dialysis in Brazil, the majority of whom (∼85%) were being funded by the Brazilian Public Health System (BPHS) (12). The dialysis prevalence in Brazil was estimated as 475 dialysis patients per million of population (pmp) (12). Although information regarding the prevalence of patients undergoing dialysis in Brazil is readily available, data on dialysis incidence are scarce and based on projections (13,14). In the present study, we aimed to evaluate the incidence of patients starting dialysis therapy in São Paulo City, the largest Brazilian metropolis, during a 5-year period (2007–2011) and also to compare it with the incidences projected for countries with equivalent populations.
PATIENTS AND METHODSThis cohort study analyzed the data from patients starting hemodialysis or peritoneal dialysis from January 1st, 2007 to December 31st, 2011, who were referred from the São Paulo City Dialysis Regulatory Bureau (SPc-DRB). SPc-DRB, which is funded by the BPHS, is a division of São Paulo City's Health Bureau, which regulates the allocation of patients with ESRD requiring dialytic therapy into 36 satellite dialysis centers. Note that the present analysis was limited to the patients receiving dialytic therapy that was supported by the public health system (approximately 85% in Brazil). In São Paulo City, when a physician refers a patient to start a chronic program of hemodialysis or peritoneal dialysis funded by the BPHS, a specific questionnaire must be completed and sent to the SPc-DRB. The patients are identified by name, mother's name, birth date, BPHS number and address. In addition to the data identification, the questionnaire comprises information about the presumptive diagnosis, previous dialytic treatment and/or kidney transplantation, hepatitis B (HBV), hepatitis C (HCV), and HIV serology, as well as the requested RRT modality. After a complete analysis of the questionnaire, each patient receives a unique SPc-DRB number before being forwarded to one of the satellite dialysis units. This protocol procedure allows the SPc-DRB (funded by the BPHS) to have almost complete control of the incidence and prevalence of dialysis patients in São Paulo City because the SPc-DRB number is required for therapy reimbursement. This form began to be recorded in electronic files in mid-2006, which provided us with the data for analysis. For the present analysis, we excluded current dialysis patients and those who had previously received a kidney transplant; additionally, the data bank was double-checked to exclude duplicate patients, those who had been transferred between dialysis units and patients not living in São Paulo City. Note that the patients with acute kidney injury were not included in the data bank because their access to dialysis therapy was not regulated by the SPc-DRB. To compare the dialysis incidence in São Paulo with the incidences projected for other countries, we used the data available from the US Renal Data System (USRDS) and the United Nations (15,16).
Statistical analysisThe variables were expressed as median (interquartile range [IQR]) or as absolute (n) and relative (%) values, as appropriate. Age- and gender-standardized dialysis annual incidence rates pmp were calculated on the basis of the official São Paulo City population (17). Standardized incidence rates were estimated to analyze the variation in incidence compared to the first year (2007). Gender comparisons by age strata were made using the Poisson regression analysis and presented by incidence rate (IR) with a 95% confidence interval (CI). A p for trend analysis was conducted to show the variations in patient characteristics throughout the study period.
Statistical significance was set at the level of p<0.05, and the statistical analyses were performed using the SPSS software version 17.0 (SPSS Inc., Chicago, IL, USA) and SAS version 9.3 (SAS Campus Drive, Cary, NC, USA 27513).
RESULTSDialysis incidence rateThe dialysis incidence rates in the city of São Paulo from 2007 to 2011 are shown in Table 1. A total of 1,956 new ESRD patients started dialysis therapy in 2007, with an adjusted incidence rate of 178 pmp. Incidence rates in 2008, 2009, 2010 and 2011 were 174, 170, 185 and 188 pmp, respectively. Using 2007 as a reference, the age- and gender-standardized incidence rates from 2008, 2009, 2010 and 2011 were, 0.98, 0.96, 1.04 and 1.06, respectively, as shown in Figure 1.
Incidence of patients starting dialysis in São Paulo from 2007–2011.
| Year | São Paulo City population∗) | Incidence | |
|---|---|---|---|
| Absolute “n” | Per million population | ||
| 2007 | 11,019,484 | 1,956 | 178 |
| 2008 | 11,093,746 | 1,927 | 174 |
| 2009 | 11,168,194 | 1,897 | 170 |
| 2010 | 11,245,983 | 2,080 | 185 |
| 2011 | 11,337,021 | 2,134 | 188 |
Considering that the São Paulo City population is as large as that of many countries, the results obtained in this study were compared not only with the incidence rate of ESRD in Brazil but also with the rates of other countries with similar populations and with South American countries (Table 2), as reported by USRDS (15). For the period between 2007 and 2009, the ESRD incident rates in São Paulo were maintained at similar levels (ranging from 178 to 170 pmp), whereas the reported overall Brazilian dialysis incidence rate during the same period ranged from 140 to 99 pmp. Note that the dialysis incidence in the city of São Paulo were comparable with those of Greece, Belgium, and the Czech Republic, countries with populations similar to that of São Paulo city. However, for the same period, the incidence rates of ESRD in São Paulo were higher than those reported for other South American countries, such as Argentina, Chile and Uruguay, but were only half the ESRD rate in the USA.
Demographic and reported incidence rates of ESRD from 2007–2009: A comparative analysis of São Paulo City with Brazil and other countries.
| Population (million) | Incidence of ESRD (pmp) | |||
|---|---|---|---|---|
| 2010∗) | 2007# | 2008# | 2009# | |
| São Paulo City | 11.25 | 178 | 174 | 170 |
| Greece | 11.36 | 192 | 201 | 204 |
| Belgium, Dutch speaking | 10.71 | 190 | 190 | 201 |
| Belgium, French speaking | 187 | 190 | 196 | |
| Czech Republic | 10.49 | 185 | 182 | 181 |
| Brazil | 194.95 | 140 | 148 | 99 |
| Argentina | 40.41 | 151 | 144 | 151 |
| Chile | 17.11 | 144 | 153 | 153 |
| Uruguay | 3.37 | 143 | 166 | 135 |
| United States | 310.38 | 362 | 363 | 371 |
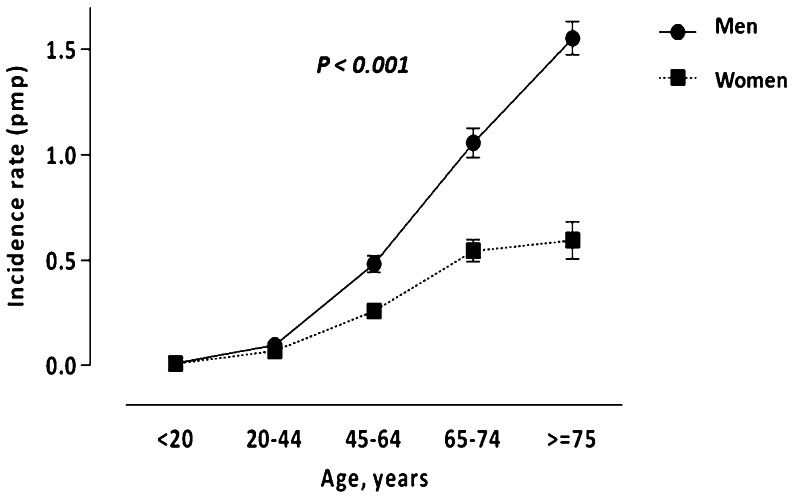
The clinical characteristics of this population are shown in Table 3. From 2007 to 2011, 9,994 patients (median age, 59 years, IQR, 47–70 years) started dialysis in São Paulo; the majority of patients were males (58.7%). The age-specific incidences, which increased steadily with age, for males and females are shown in Figures 2A and 2B. Using individuals younger than 20 years as the reference point, the rate for starting dialysis was 8.16 (95% CI, 7.29–9.12) times higher for patients aged between 20 and 44 years, 36.08 (95% CI, 32.34–40.25) times higher for patients aged between 45 and 64 years, 77.62 (95% CI, 69.41–86.79) times higher for persons aged between 65 and 74 years and 98.99 (95% CI, 88.45–110.79) times higher for those aged 75 years or older. Males had a higher dialysis incidence than women (IR: 1.87. 95% CI: 1.82–1.93) (Figure 3).
Demographic and clinical characteristics of patients who started dialysis treatment in São Paulo City from 2007–2011.
| Year | |||||||
|---|---|---|---|---|---|---|---|
| TOTAL | 2007 | 2008 | 2009 | 2010 | 2011 | p for trend | |
| Subjects | n = 9,994 | n = 1,956 | n = 1,927 | n = 1,897 | n = 2,080 | n = 2,134 | |
| Gender, n (%) | 0.574 | ||||||
| Male | 5,870 (58.7%) | 1,146 (58.6%) | 1,122 (58.2%) | 1,121 (59.1%) | 1,210(58.2%) | 1,271(59.6%) | |
| Female | 4,124 (41.3%) | 810 (41.4%) | 805 (41.8%) | 776(40.9%) | 870(41.8%) | 863(40.4%) | |
| Age, n (%) | |||||||
| <20 years | 168 (1.7%) | 30(1.5%) | 41 (2.1%) | 34(1.8%) | 31(1.5%) | 32(1.5%) | |
| 20–44 years | 1,981 (19.8%) | 400 (20.4%) | 349 (18.1%) | 400(21.1%) | 396 (19.0%) | 436 (20.4%) | |
| 45–64 years | 4,181 (41.8%) | 819 (41.9%) | 782(40.6%) | 769(40.5%) | 935 (45.0%) | 876 (41.0%) | 0.312 |
| 65–74 years | 2,002 (20.0%) | 369 (18.9%) | 409 (21.2%) | 364(19.2%) | 404 (19.4%) | 456 (21.4%) | |
| ≥75 years | 1,662 (16.7%) | 338 (17.3%) | 346 (18.0%) | 330(17.4%) | 314 (15.1%) | 334 (15.7%) | |
| Etiology of CKD, n (%) | |||||||
| Diabetes | 2,305(23.1%) | 465(23.8%) | 453 (23.5%) | 384(20.2%) | 556(26.7%) | 447(21.0%) | 0.842 |
| Hypertension | 1,550(15.5%) | 339(17.3%) | 326 (16.9%) | 272(14.4%) | 325(15.6%) | 288(13.5%) | |
| Glomerulonephritis | 475(4.8%) | 120(6.1%) | 97 (5.0%) | 94(5.0%) | 90(4.3%) | 74(3.5%) | |
| Polycystic Kidney Disease | 132(1.3%) | 19(1.0%) | 36 (1.9%) | 25(1.3%) | 26(1.3%) | 26(1.2%) | |
| Unknown | 5,320 (53.2%) | 954(48.8%) | 935 (48.5%) | 1,065(56.1%) | 1,070(51.5%) | 1,296(60.7%) | |
| Dialysis modality, n (%) | |||||||
| Hemodialysis | 9,256 (92.6%) | 1,758 (89.9%) | 1,776 (92.2%) | 1,756(92.6%) | 1,950(93.7%) | 2,016(94.5%) | <0.001 |
| Peritoneal Dialysis | 738 (7.4%) | 198 (10.1%) | 151 (7.8%) | 141(7.4%) | 130(6.3%) | 118(5.5%) | |
| Chronic Infectious Diseases, n (%) | |||||||
| HBV | 364 (3.6%) | 33 (1.7%) | 50 (2.6%) | 30(1.6%) | 119(5.7%) | 132(6.2%) | 0.039 |
| HCV | 463(4.6%) | 89 (4.6%) | 109 (5.7%) | 87(4.6%) | 81(3.9%) | 97(4.6%) | |
| HIV | 305 (3.1%) | 26 (1.3%) | 24 (1.3%) | 30(1.6%) | 93(4.5%) | 132(6.2%) | |
Overall, diabetes (23.1%) and hypertension (15.5%) accounted for most of the main presumptive diagnoses of CKD requiring RRT in São Paulo City during the study period, representing approximately 39% of all cases. Note that the majority of patients were referred without a known etiology. The CKD etiologies did not change significantly over the study period (Table 3).
Hemodialysis was the dialysis modality of choice, showing a significant increase over the last 5 years. The percentage of patients referred for peritoneal dialysis decreased from 10.1% in 2007 to 5.5% in 2011.
Incidence rates of hepatitis B, hepatitis C and anti-HIV seropositivity in dialysis patientsThe incidence of patients with positive serology for the HBV as well as HIV increased gradually during the study period, whereas the incidence of HCV remained stable (Table 3).
DISCUSSIONThe present study analyzed the incidence of patients starting chronic dialysis therapy in São Paulo City from 2007 to 2011. The data for this analysis was obtained from the data bank of a government agency that regulates the allocation of patients with ESRD requiring dialysis therapy, which was funded by the BPHS. In Brazil, the BPHS is responsible for supporting the majority of patients maintained on chronic dialysis therapy, approximately 85% of all patients; the remaining 15% of patients are supported by private health insurance companies (12). It is remarkable that the data presented here are not based on projections but are the result of the reliable analysis of concrete data on the incidence of chronic dialysis supported by the government in São Paulo City.
The dialysis incidence in São Paulo (i.e., 170-188 pmp for the study period) was higher than that estimated for the entire Brazilian population. According to the Brazilian Dialysis Census 2009, the incidence of patients on dialysis was estimated to be 144 pmp (18), and USRDS projections showed an even lower figure (99 pmp) (15), whereas the incidence rate in São Paulo (according to the current study) was higher, 170 pmp. One possible explanation for these disparities may be related to the method employed for calculating the incidence. The rates reported by the Brazilian Dialysis Census were based on a questionnaire, completed online by the dialysis centers, which has a response rate of approximately 70% (12); thus, the incidences were calculated based on estimates that could have been inaccurate. Alternatively, this discrepancy might have been the result of geographic and socioeconomic disparities among the different regions in Brazil. As recently reported by Couchoud et al. (19), in the French population, socioeconomic background and the medical practices related to public health system may explain substantial between-area variations in CKD patients access to renal replacement therapy. According to the Brazilian Dialysis Census 2011 (12), the dialysis incidence for the southwest region, in which São Paulo is located, was nearly identical to the rate presented here. However, one important observation of our study is that incidence rates in São Paulo were found to be rather stable during the observation period. The annual incidence of dialysis initiation varied by only ±5% as compared to the 2007 data. This finding is in agreement with the reported stabilization of European dialysis incidence (10) and even decreasing trends in the USA (8,9).
Our data showed that the incidence of dialysis initiation in São Paulo was comparable to the ESRD/dialysis incidence rates reported for some European countries with similar populations, such as Greece, Belgium and the Czech Republic (15). However, the incidence of dialysis initiation in São Paulo was higher than those reported by other South American countries, but still half the reported incidence rate in the USA (15). A limitation in this comparison is that our data did not include incident kidney transplants. However, in the spite of the large kidney transplantation program in Brazil—with 4,630 kidney transplants performed in 2010 (24.1 pmp) (20)—particularly in the southwest region (13,14,20,21), the percentage of preemptive renal transplantation in Brazil is still low. Therefore, the dialysis incidence most likely equals the ESRD incidence (13,14,20,21). We should also consider some limitations of the present analysis, such as that our data collection did not include patients with dialysis therapy covered by private health insurance or those who died before being discharged from the hospitals. Taken together, we may speculate that the rates presented here underestimate the real dialysis incidence in São Paulo City. The lack of national data on CKD patients to serve as a control, as previously noted (22), limits our analysis, and thus readers also should note that the comparisons between the dialysis incidence in São Paulo City and those for Brazil and other countries presented here are crude and may be not be precise because of the differences in the compositions of the various populations.
The increased incidence of dialysis in people older than 65 years occurred in parallel with longer life expectancies for the Brazilian population and with the comorbidities associated with aging (9,23). Our results also show an important gender difference in dialysis incidence, which is in agreement with the previously reported faster progression rate of many renal diseases in males (24–27). This difference in CKD progression between males and females may be attributed to a number of factors, including the differential impact of sex hormones on kidney damage and also a combination of environmental, socioeconomic, lifestyle and health care factors (28).
The cause of the CKD was unknown for the majority of the patients, as was previously reported for the Brazilian population (14). This issue may be a consequence of the fact that the majority of patients initiating RRT in Brazil come from emergency units at public hospitals, and only a small proportion of patients had actually seen a nephrologist before starting dialysis (21). Hemodialysis was the most common modality of dialysis therapy for the patients initiating RRT in São Paulo, and a clear decreasing trend in the choice of peritoneal dialysis was observed in our study. This trend agrees with the data from the USA for the corresponding time period (15), although recent data indicates that the number of patients treated with peritoneal dialysis pmp in both developing and developed countries has increased over the last decade (29). Among the factors that may favor the choose of hemodialysis instead of peritoneal dialysis in Brazil, the economic constraints undoubtedly have a major impact. With regard this, although the reimbursement for hemodialysis and peritoneal dialysis provided by BPHS is approximately the same, the final income for the owners of dialysis centers is much lower for peritoneal dialysis, which impacts financial incentives and the viability of maintaining these programs (21).
An interesting observation is the progressive increase in the number of patients with HBV and HIV positive serology. Of note, the number of individuals infected by HBV may be overestimated because since 2009, patients classified as positive were not only those with the surface antigen (HBsAg positive) but also patients who presented with anti-HBc positive in the absence of a positive anti-HBs. In fact, the prevalence of chronic HBV infection in São Paulo City was estimated at 1.02% (30). The observed increase in the incidence of HIV patients starting dialysis may reflect the significant improvement in the life expectancies of HIV patients, which corresponds with access to the highly active antiretroviral drugs provided to the affected population through the BPHS (31).
To conclude, the incidence rate of patients starting RRT from 2007 to 2011 in São Paulo (using reliable data on actual treatments) was higher than the projected incidence for the entire country of Brazil. Compared with the 2007 data, the incidence rates were stable from 2008 to 2011. We hope that the current report will stimulate action toward creating a Brazilian registry of dialysis patients. Such a registry would be a valuable tool for the planning, development and monitoring of national healthcare policies. In particular, such data would allow for a better understanding of the factors influencing the temporal trends in the changes in RRT incidence and prevalence patterns, such as the timing of dialysis initiation, choice of dialysis modality and clinical outcomes (morbidity and mortality); these data are crucial when formulating national strategies for RRT in Brazil.
Conflicts of Interest: Baxter Healthcare Corporation employs Bengt Lindholm. Baxter Novum is the result of a grant to the Karolinska Institutet from the Baxter Healthcare Corporation. None of the other authors have reported any conflicts of interest.
AUTHOR CONTRIBUTIONSCordeiro AC and Cunha RF created the database. Cordeiro AC, Cunha RF, Lindholm B, and Noronha IL conceived the study. Carrero JJ, Qureshi AR, and Castro I performed the statistical analysis. Cordeiro AC, Carrero JJ, Qureshi AR, Cunha RF, Lindholm B, Castro I, and Noronha IL participated in the writing of the manuscript.
We would like to thank the São Paulo City's Dialysis Regulatory Bureau group, which was responsible for establishing and updating this data bank. Juan J. Carrero acknowledges grant support from the Swedish Research Council and the Loo and Hans Osterman Foundation. Baxter Novum is the result of a grant to the Karolinska Institutet from the Baxter Healthcare Corporation.
No potential conflict of interest was reported.