To present selected results of military conscript surveys related to HIV/AIDS, conducted in Brazil, 1997-2002.
METHODSQuestionnaires including information on socio-demographic data, sexual behavior practices, sexually transmitted infections-related problems, and use of injecting drugs were completed by 30970 individuals, obtained through a 2-stage sampling. An index of sexual risk behavior was developed to take into account multiplicity of partners and irregularity of condom use. The HIV infection prevalence rate was estimated for 2002. Logistic regression was used to identify the most important determinants of HIV infection.
RESULTSThe percentage of regular condom use increased from 38% (1997) to 49% (2002), and the index of sexual risk behavior decreased from 0.98 in 1997 to 0.87, in 2002. The HIV infection prevalence rate was 0.09%, in 2002, which remained unchanged since1998 Riskier sexual practices among young men with incomplete education and among “men who have sex with men” were found as well as among the participants who reported at least one sexually transmitted infections - related problem. The most important predictor of HIV infection was to be positive for syphilis.
CONCLUSIONSThe estimated value of the HIV infection prevalence supports the diagnosis of a concentrated HIV epidemic, in Brazil. Results indicate that particular attention needs to be paid for regional differentials, and for special subgroups, in Brazil.
Apresentar determinados resultados de levantamentos sobre HIV/AIDS em conscritos do Exército Brasileiro, conduzidos em 1997-2002.
MÉTODOSAplicaram-se questionários em 30970 conscritos, selecionados segundo um esquema de amostragem em 2 estágios, para obter informações sobre comportamento sexual, problemas relacionados a infecções sexualmente transmitidas e uso de drogas injetáveis. Desenvolveu-se um índice de comportamento sexual de risco para contemplar multiplicidade de parceria sexual e uso de preservativo. Estimou-se, para o ano de 2002, a taxa de prevalência de infecção pelo HIV.
RESULTADOSA porcentagem de uso regular de preservativo aumentou de 38%, em 1997, para 49%, em 2002. O índice de comportamento sexual de risco decresceu de 0,98 em 1997 para 0,87, em 2002. O índice de prevalência de infecção HIV foi de 0.09%, in 2002, permanecendo inalterado desde 1998 Práticas sexuais de maior risco foram observadas entre aqueles com baixa escolaridade e em “homens que fazem sexo com homens”, como também entre aqueles com problemas de infecções sexualmente transmissíveis. O mais importante preditor de infecção pelo HIV foi a soropositividade para lues.
CONCLUSÕESA prevalência estimada de infeção pelo HIV suporta o diagnóstico que a epidemia de AIDS, no Brasil, é do tipo “concentrada”. Os resultados indicam que são necessárias medidas de intervenção que contemplem diferenças regionais e também voltadas para subgrupos populacionais especiais.
Studies to determine factors involved in sexual risk behavior among adolescents have been widely recognized as key tools for controlling the spread of HIV.1 Essentially, they provide information for the development of preventive strategies and contribute to maximizing the effectiveness of interventions.
In Brazil, some initiatives were undertaken in the 1990s to monitor risk behavior among adolescents. A pioneering study on behavioral risks for HIV infection with Brazilian military conscripts was conducted in 1992, based on a small sample in the city of Campo Grande, MS.2 The Brazilian Demographic and Health Survey carried out in 1996, which included a module on sexual behavior and knowledge about HIV transmission, is a further example of this kind of research.3
The first survey among military conscripts was carried out in Thailand.4 Since 1990, cross-sectional studies have been undertaken in an effort to broaden identification of sexual behavior patterns related to HIV infection.5,6,7 Intercourse with commercial sex workers was one of the factors most closely associated with the HIV infection and other sexually transmitted infections.8 Reports on the successes obtained in the prevention and control of the spread of HIV and AIDS began to appear by the end of the 1990s.9,10
In Brazil, the technical cooperation project between the Ministry of Health and the Ministry of the Army started in 1996. This partnership brought together a number of activities involving prevention of sexually transmitted infections (STI) among young men and made possible the implementation of surveys among conscripts at the time they presented themselves to the Military Selection Committees. Since military service is mandatory in Brazil and young males have to present themselves to the Army when they complete 17 to 18 years of age, military conscripts are very representative of the population of young men.
The surveys in Brazilian military conscripts were carried out on an annual basis from 1996 to 2000. Aiming to enlarge the knowledge about sexual behavior practices of young Brazilian men, these surveys have attempted to focus on different subjects from year to year. Some modules have been repeated periodically to establish relevant changes in unsafe sexual practices among male adolescents as well as to monitor prevention and intervention activities with respect to HIV/AIDS.
In 1996, the first national survey focused only on knowledge about HIV transmission. In 1997, a few questions about condom use were introduced.11 In 1998, a more wideranging questionnaire was used. This involved a series of questions about sexual practices and other risk behaviors related to HIV, such as use of injecting drugs. However, the 1998 sample was not representative of the Brazilian young male population, as only areas with excessive AIDS incidence were selected for study. In that year, blood samples were also collected for HIV testing. The results were compared with a control group composed of randomly selected conscripts in Rio de Janeiro and São Paulo.12
After 1999, the full questionnaire about sexual practices has been adopted, with new topics being introduced each year. The 1999 survey focused on the relationship between sexual risk behavior and the use of licit and illicit drugs.13 In year 2000, socioeconomic inequalities in risky sexual behavior were examined.11
The most recent survey among Brazilian military conscripts was carried out in year 2002, with the specific objective of estimating the HIV prevalence rate at the national level and to establish the most important determinants of HIV infection among young men.
This paper presents temporal trends of HIV-related risk behavior in Brazilian military conscripts based on the 1997 through 2002 surveys.
METHODSThis study refers to selected results of the analyses of military conscript surveys that were carried out during the period 1997 to 2002 in Brazil. Special emphasis is given to the results obtained in 2002.
This project was approved by the National Commission for Research Ethics of the National Health Council (number 4306).
The surveys were carried out through a questionnaire that was completed by the conscripts themselves at the time they presented themselves to the Army authorities. Illiterate conscripts and functional illiterates in other words, young men who would have been unable to respond coherently to the written questionnaires have always been excluded, constituting one of the limiting factors of the study. Considering that informed consent could lead to refusals and be a source of bias, the self-reported and anonymous questionnaires were deposited directly into a container as a way of guaranteeing confidentiality for the interviewee.
Yearly sample sizes and summarized descriptions of objectives and sampling plans are presented in Table 1. Detailed descriptions of the 1997 to 2000 sampling designs and results are presented elsewhere.11 All analyses were restricted to 17- to 20-year-old participants, because older conscripts are enrolled in military service only in exceptional situations.
Summary descriptions of sampling plans and objectives of the surveys. Brazilian Army conscripts, 1997-2002
| Year | Sample size | Main objectives | Summarized sampling plan | Proportion (%)17-20 years old |
|---|---|---|---|---|
| 1997 | 9844 | To establish the relationship between the level of knowledge about HIV transmission and sexual practices. |
| Age of conscript was not obtained. |
| 1998 | 30318 | To estimate HIV prevalence rates in areas with excessive AIDS incidence rates. | 2-stage sampling. Stratification of primary units: 2 geographic areas composed of municipalities with disproportional growth rates of AIDS incidence in the 1990s and 1 control stratum composed of municipalities of Rio de Janeiro and São Paulo | 96.9 |
| 1999 | 29373 | To establish the relationship between sexual behavior and use of licit and illicit drugs. | 2-stage sampling. Stratification of primary units: macro-geographic region and metropolitan areas. | 96.3 |
| 2000 | 23659 | To investigate socioeconomic inequalities in sexual behavior. | 2-stage sampling. Stratification of primary units: macro-geographic region, municipality size (0-50000; 50001-300000; 300001+ inhabitants), capital/not capital. | 96.3 |
| 2002 | 30970** literate ones | To estimate HIV prevalence rate and establish main predictor factors for HIV infection. | 2-stage sampling. Stratification of primary units: macro-geographic region and municipality size (0-50000; 50001-400000; 400001+ inhabitants). | 94.0 |
The questionnaires included information on social and demographic data, sexual behavior practices, STI-related problems, and use of injected drugs. In the years 1998 and 2002, blood samples of the participants were collected for syphilis and HIV testing. All the tests were carried out in the Laboratory of the Biology Institute of the Brazilian Army.
To analyze sexual behavior over time, the following indicators were used:
- i)
Rate of sexual activity;
- ii)
Age of sexual debut;
- iii)
Number of sexual partners (lifetime, past year, and past month);
- iv)
Condom use at last sexual intercourse;
- v)
Regularity of condom use over the past year, according to type of partner (fixed, casual, paid partner, the conscript as payee). Regularity of condom use (by type of partner) was established by the proportion of conscripts who reported that they had always used condom in the past year (by type of partner).
Additionally, a summary index to evaluate unsafe sexual behavior over time was defined. The Index of Sexual Risk Behavior over the past year (ISRB) was defined as the weighted sum of the number of partners over past year, weighted by the regularity of condom use, according to type of partners. The following 4 types of partner (of either sex) were considered: fixed or regular partner; casual partner friend, acquaintance, “one night stand”; paid partner the conscript paid the partner for sexual intercourse; paying partner the partner paid the conscript for sex.
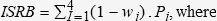
Mathematically, the ISRB is expressed as follows:
i indicates the type of partner;
wi = 0.00 – never used a condom with partners in category i;
wi = 0.25 – used a condom in less than half of the occasions with partners in category i;
wi = 0.75 – used a condom in over half the occasions with partners in category i;
wi = 1.00 – used a condom in all occasions with partners in category i;
Pi = number of partners in category i.
The index equals 0 when the conscript had always used condom in the past year, with any type of partner, and increases with the nonregularity of condom use with multiple partners.
Differences in sexual risk behavior were also analyzed according to the sexual preference of the responding conscript: men who have sex with other men (MSM) or with women only.
To analyze the use of injected drugs, the question “Have you ever injected drugs?” had 6 optional answers (never; only tried; had used, but no longer; uses now and then; uses only on weekends; uses frequently). An injecting drug user
(IDU) was considered to be a respondent who answered in the affirmative to 1 of the 3 last options. The category “used at least once” included any one of the affirmative options.
In the year 2002, the sample size was calculated from an estimated HIV prevalence rate of 0.1% with a 95% confidence interval and bilateral error of 0.04%. Considering a design effect of 1.20 and possible nonrespondent losses, the final sample size was adjusted to 40000 conscripts. The sample design had 2 stages of selection: in the first stage, 105 Military Committees were systematically selected with probability proportional to size, defined by the frequency of conscripts in the precedent year. Macro-geographic regions (North; Northeast; Southeast; South; Center-West) and size of municipality categories (0 to 50,000; 50,000 to 400,000; 400,000 and more inhabitants) stratified the primary sampling units. In the second stage, conscripts were selected in each Military Committee with equal probability.
For the HIV tests in the year 2002, the blood samples were tested with an ELISA technique. The inconclusive ones and those with reagent results were tested for confirmatory results using the Western blot test. Serological examinations for syphilis were also performed by ELISA.
The 2002 HIV prevalence rate was estimated taking into account the sampling design. Logistic regression procedures were used to evaluate the effects of behavioral practices and socio-demographic factors as well as to identify the most important predictors of HIV infection.
RESULTSIndicators of HIV-related risk behaviors over time are presented in Table 2. The percentage of regular condom use increased substantially from 38% in 1997 to 49% in 2002. In the last 3 years, improvements were also observed including: an increase of regular condom use with paid partners (commercial sex workers), an increase in the proportions of condom use at last intercourse from 62% to 70%, and a significant decrease in the percentage of injecting drug users.
Indicators (%) of sexual behavior by year. Brazilian Army conscripts, 1997-2002
| Group | Proportions | Year | |||
|---|---|---|---|---|---|
| 1997 | 1999 | 2000 | 2002 | ||
| Entire sample | Sexual activity | 83.9 | 81.8 | 83.0 | 82.5 |
| Injected cocaine | |||||
| At least once in the past | …* | 1.9 | 0.9 | ||
| Current user | 0.6 | 0.2 | |||
| Sexually active conscripts | Sexual debut <14 years old | 24.8 | 19.8 | 20.2 | |
| More than 10 partners over lifetime | 19.7 | 19.6 | 18.7 | ||
| Men who have sex with men | 3.3 | 3.0 | 2.9 | ||
| Condom use at last sexual intercourse | 62.2 | 68.8 | 69.7 | ||
| Sexually active conscripts (past year) | At least one paid partner | 16.6 | 17.3 | 16.2 | |
| The conscript has been paid at least once | 5.5 | 5.9 | 4.1 | ||
| Regular condom use | |||||
| Fixed partner | 43.1 | 48.4 | 43.7 | ||
| Casual partner | 53.2 | 56.2 | 57.2 | ||
| Paid partner | 68.8 | 67.0 | 77.9 | ||
| The conscript had been paid | 53.8 | 48.6 | 44.0 | ||
| Any type of partner | 37.6 | 44.8 | 49.2 | 48.5 | |
| More than 5 sexual partners (past year) | 14.2 | 13.6 | 13.9 | ||
Table 3 shows the improvement in regular condom use from 1999 to 2002 in all population subgroups except for the group of conscripts with more than 5 partners over past year for which the proportion of regular condom use remained the same. From 1999 to 2002, the index of sexual risk behavior (ISRB) decreased from 0.98 to 0.87. This index can be interpreted as the mean number of partners with unsafe sex over the past year. Despite the overall improvement, the results indicate riskier sexual practices among young men with lower education levels when compared to those with higher educational levels. Also, it is worth noting that while the group of MSM had a very high ISRB value, it also had the most significant reduction over this period of time. The group of conscripts with more than 5 partners over past year is of concern, since the ISRB was greater than 2, indicating multiple partners and unsafe sex. Moreover, no signs of improvement were observed. On the contrary, the ISRB showed an increase from 2.02 to 2.11 in this subgroup.
Percentage (%) of regular condom use and index of sexual risk behavior (ISRB) by population subgroups and year. Brazilian Army conscripts, 1999 and 2002
| Subgroup | % Regular Condom Use | ISRB | ||
|---|---|---|---|---|
| 1999 | 2002 | 1999 | 2002 | |
| Entire sample | 44.8 | 48.5 | 0.96 | 0.87 |
| Incomplete high school | 41.8 | 44.0 | 1.11 | 1.01 |
| Complete high school | 47.4 | 50.1 | 0.83 | 0.83 |
| Men who have sex with men | 30.3 | 34.1 | 1.90 | 1.56 |
| More than 5 sexual partners | 42.2 | 42.0 | 2.02 | 2.11 |
| (past year) | ||||
| Sexual debut <14 years old | 37.1 | 41.7 | 1.38 | 1.26 |
ISRB = index of sexual risk behavior
For the year 2002, occurrence of problems related to sexually transmitted infections (STI) is presented in Table 4. The most frequent problems were lesions and blisters on the penis. The main STI problems discharge from the urethra and penis warts were reported less often but cannot be ignored, since the proportions are considerably high: 3.9% (urethral discharge) and 2.9% (penis warts).
Indicators (%) of sexual behavior in conscripts who reported STI-related problems and were positive for syphilis. Brazilian Army conscripts, 2002
| Problem | % of Conscripts | % Regular Condom Use | ISRB |
|---|---|---|---|
| Urethral discharge | 3.9 | 24.3 | 1.89 |
| Blisters on penis | 5.7 | 28.6 | 1.89 |
| Lesions on the penis | 7.5 | 29.2 | 1.66 |
| Warts on penis | 2.9 | 21.4 | 2.10 |
| None of these problems | 84.4 | 52.6 | 0.73 |
| Syphilis (positive) | 0.848 | 34.2 | 1.37 |
Evidence of the association between STI-related problems and unsafe sexual practices were also found. The proportions of regular condom use were much lower among the participants who reported any of the STI-related problems. Notable differences were also found for the mean values of the ISRB. Among those who did not mention any problems at all, the ISRB was 0.74, but among the participants who reported at least one STI-related problem, the ISRB was 1.60. Regarding syphilis, 0.848% tested positive; among these individuals, only 34% reported regular condom use, and the ISRB equaled 1.37.
In Table 5, HIV prevalence rate results for year 2002 are presented. The total sample prevalence rate was estimated as 0.090%. Comparison among population subgroups shows significant differences among the prevalence rates. The highest HIV prevalence rate (0.984%) was found among the participants that were positive for syphilis, followed by the MSM subgroup (0.564%). Conscripts with low educational levels showed a significantly higher HIV prevalence rate (0.156%) than those who had completed high school (0.063%). No HIV-infected cases were found in the IDU population.
HIV infection prevalence rate in selected subgroups. Brazilian Army conscripts, 2002
| Subgroup | Size(%) | HIV Prevalence Rate (%) | Prevalence Rate ±SE* |
|---|---|---|---|
| Entire Sample | 100.0 | 0.090 | 0.072-0.108 |
| Incomplete high school | 29.3 | 0.156 | 0.113-0.199 |
| Complete high school | 70.7 | 0.063 | 0.045-0.081 |
| Men who have sex with men | 2.9 | 0.564 | 0.278-0.850 |
| At least 1 STI related problem | 15.6 | 0.226 | 0.156-0.296 |
| Positive for syphilis | 0.8 | 0.984 | 0.310-1.658 |
| Resident of Southern Brazil | 14.8 | 0.157 | 0.097-0.217 |
| More than 10 lifetime sexual partners | 18.7 | 0.213 | 0.151-0.275 |
Logistic regression results (Table 6) show that the most important predictors of HIV infection were as follows: being positive for syphilis, having sex with other men (MSM), having reported at least 1 problem related to STI, having more than 10 sexual partners over a lifetime, being a resident of Southern Brazil, and having a low education level.
Predictor factors for HIV infection. Brazilian Army conscripts, 2002
| Predictors | OR | 95% CI | P value | OR (adjusted) | 95% CI** | P value |
|---|---|---|---|---|---|---|
| Positive for syphilis | 10.68 | 2.60 - 43.84 | .0011 | 5.72 | 1.32 - 24.90 | .02 |
| Men who have sex with men | 1.80 | 2.05 - 17.97 | .0010 | 4.06 | 1.29 - 12.80 | .02 |
| At least 1 problem related to STI | 3.49 | 1.59 - 7.66 | .0018 | 2.76 | 1.18 - 6.45 | .02 |
| More than 10 lifetime sexual partners | 2.89 | 1.32 - 6.32 | .0078 | 2.33 | 1.05 - 5.18 | .04 |
| Resident of Southern Brazilian | 2.00 | 0.83 - 4.80 | .12 | 2.77 | 1.10 - 6.99 | .03 |
| Incomplete high school | 2.47 | 1.15 - 5.31 | .02 | 2.06 | 0.92 - 4.60 | .08 |
Comparisons among the 2002 survey and those performed in earlier years show some very important results such as the increase in condom use measured by both regular condom use and condom use at last intercourse and the substantial reduction in the size of the IDU population. Moreover, the 2002 HIV prevalence rate showed stabilization, with no signs of increase when compared to the 1998 estimated prevalence rate in the control stratum.12
However, despite the unequivocal improvements regarding the male adolescent population, results indicate that particular attention needs to be paid to the group of those least socially advantaged young men. Not only was the proportion of regular condom use lower among the participants with low educational levels, but also the ISRB was higher than the index found among the participants with higher education levels. In addition, the HIV prevalence results obtained in 2002 indicated that the young men with low education levels are more likely to develop HIV infection. These findings indicate the persistence of social inequalities in the frequency of unsafe sex over time. Considering that illiterate conscripts were not included in the survey, the observed social inequalities certainly underestimate their real magnitudes.
Further results meriting attention are the sexual practices in the MSM subgroup. This group had a low percentage of regular condom use and a high ISRB, meaning multiple partners and unsafe sex. The HIV prevalence rate in this group was 6 times greater than the overall prevalence rate.
A positive test for syphilis and the reporting of a previous STI problem were both important predictors of HIV infection. These findings are similar to those observed among conscripts in Thailand.14,15
The present results also confirmed the various studies that have drawn attention to the association between the occurrence of other STI and HIV infection,16 not only because the presence of a STI in one of the partners increases the risk of HIV transmission,17 but also because the risk factors are similar, which assumes greater significance in view of the selective sexual contacts among social groups.18,19
As has been pointed out by Ronald,20 the synergism between HIV and other STIs provides unique opportunities for targeted interventions. Increasing access to clinical services for STI and improving clinical management of STIs have been shown to be successful strategies in lowering HIV transmission.21
The higher HIV prevalence among young males in Southern Brazil is also a matter of concern. It consistently emphasizes the continuous spread of HIV/AIDS in this Brazilian region where the use of injected drugs has been the main drive of the epidemic. A previous regional comparison has already shown that the pace of the AIDS epidemic in the South has yet to slow down. While the AIDS epidemic has tended to achieve a plateau in the Southeast, a persistent growth rate has been evidenced in the South.22
Another noteworthy aspect is the synergy of sexual risky practices. The young men who reported multiple partners and sexual debut at an earlier age tended to engage in unprotected sex more frequently. Cruz-Grote23 points out that the preventive initiatives and programs should be implemented in pre-adolescence, before the beginning of their sex lives. Valois et al.24 propose creative approaches in school and community settings as well as long-term intervention strategies focused on adolescent behavior changes and environmental modifications. In addition to the current approaches, Rotheram-Borus25 contemplated the possibility of structural changes such as decreasing poverty, ensuring access to healthcare, and increasing social opportunities.
Considering the geographic, social, and cultural heterogeneity of Brazil, one of the greatest challenges to be faced is to ensure that the measures undertaken succeed in having a broad, all-embracing impact, particularly among those groups that are most difficult to access with preventive measures.
The authors thank the technicians from the Laboratory of the Biology Institute of the Brazilian Army, in Rio de Janeiro City, for their laboratory work.