To study the immediate and late results obtained from the implantation of vena cava filters in cancer patients with deep vein thrombosis concomitant with neoplasia.
METHODSThis was a retrospective evaluation of 50 patients with an association of cancer and deep venous thrombosis who underwent interruption of the inferior vena cava and the insertion of permanent vena cava filters. The indications for the procedure, filter implantation technique, early and late complications related to the operation, and the clinical evolution were evaluated.
RESULTSThe most frequent indication for filter implantation was the contraindication for full anticoagulant treatment (80%). The femoral vein was the preferred access route (86% of the patients). There were no complications related to the surgical procedure. During the follow-up, the following complications were observed: 1 episode of nonfatal pulmonary thromboembolism, 2 cases of occlusion of the inferior vena cava, and 1 case of thrombus retained in the device. Twenty patients (40%) died due to progression of the neoplasm.
CONCLUSIONSInterruption of the inferior cava vein using an endoluminal filter is a procedure with a low rate of complications. It is a safe and efficient measure for preventing pulmonary embolism in cancer patients who have deep vein thrombosis of the lower limbs.
Estudar os resultados imediatos e tardios obtidos com a implantação de filtros de veia cava inferior em pacientes com trombose venosa profunda concomitante a neoplasia.
MÉTODOSAvaliamos retrospectivamente 50 pacientes com câncer e trombose venosa profunda associada submetidos a interrupção de veia cava inferior com filtros intraluminais definitivos. Foram estudados aspectos referentes à indicação do procedimento, à técnica de implante dos dispositivos, complicações precoces e tardias relacionadas à operação e à evolução dos pacientes.
RESULTADOSA indicação mais freqüente para o procedimento foi a impossibilidade de anticoagulação plena (80%) e a via de acesso preferencial foi a punção da veia femoral, realizada em 86% dos pacientes. Não houve complicações relativas ao implante dos filtros. Durante a evolução ocorreram: um episódio de tromboembolia pulmonar não fatal e dois casos de oclusão da veia cava inferior; em um paciente foi demonstrada a presença de coágulo retido no dispositivo. Vinte pacientes (40%) faleceram devido à neoplasia.
CONCLUSÃOA interrupção da veia cava inferior com filtro endoluminal é um procedimento com baixo índice de complicações e eficaz na prevenção da embolia pulmonar nos pacientes com tromobose venosa profunda de membros inferiores portadores de câncer.
The relationship between neoplasia and venous thromboembolism is well established, either through the presence of related risk factors (chemotherapy,1,2,3,4,5,6 hormone therapy,5–7 immobilization,5 implantation of venous catheters,4,8,9,10 extrinsic compression of deep veins 5), or because of a possible condition of hypercoagulability that has still not been completely explained.4,6,11
Around 15% of neoplasic patients may present thromboembolic phenomena, and these are the second major cause of death among these patients.12,13 Likewise, it is known that individuals with venous thrombosis of unknown cause present a greater incidence of cancer.
It is not rare for patients with deep vein thrombosis (DVT) associated with cancer to be in a condition in which full anticoagulant treatment may be contraindicated: conditions most likely associated with this are cerebral metastases, active tumoral bleeding, thrombocytopenia or pulmonary thromboembolism, and the need for invasive procedures. Therefore, when anticoagulant treatment is contraindicated, the implantation of vena cava filters is necessary.
There has been a progressive increase in the utilization of vena cava filters. However, the number of articles regarding their utilization in cancer patients is still small, especially within our country.
The objective of the present work was to prospectively study the results obtained from the implantation and long-term utilization of vena cava filters in cancer patients.
METHODWe retrospectively evaluated 50 patients with some type of cancer who concomitantly had deep vein thrombosis in lower limbs and underwent vena cava filter implantation between January 1998 and January 2004.
Half of the cases were male patients (25 cases). The age range was from 28 to 89 years (average of 60.3). The most frequent indication for the procedure was the presence of DVT associated with some contraindication for full anticoagulant treatment (40 patients). The other situations in which the implantation of a vena cava filter was indicated were (i) the occurrence of pulmonary thromboembolism while the appropriate anticoagulant treatment was being applied (6 cases); (ii) pulmonary thromboembolism with severe respiratory dysfunction compromising more than 50% of the pulmonary parenchyma with right oor without a right ventricular pressure higher than 60 mm Hg (4 cases). Among all patients undergoing vena cava filter implantation, the most frequently found cancer types were colon and prostate cancer [Table 1].
Location of the cancer in patients submitted to vena cava filter implantation
| Neoplasia | Number of patients |
|---|---|
| Colon | 8 |
| Prostate | 7 |
| Breast | 5 |
| Ovary | 5 |
| Lung | 3 |
| Retroperitoneal sarcoma | 3 |
| Urinary bladder | 3 |
| Stomach | 2 |
| Cervix | 2 |
| Endometrium | 2 |
| Astrocytoma | 2 |
| Non-Hodgkin lymphoma | 2 |
| Bone | 2 |
| Pancreas | 1 |
| Larynx | 1 |
| Leukemia | 1 |
| Liver | 1 |
All the procedures were performed in the surgical room after digital cavography using iodide contrast, with the aid of radioscopy. Angiography was repeated after releasing the filter to observe and document whether the device had been correctly positioned. All but one of the filters were implanted in the infrarenal portion of the vena cava. The only 1 implanted above the renal veins, was in a patient who had thrombosis of the vena cava below the point where the renal veins emerge.
General anesthesia was used for 26 patients, of whom 16 underwent operations during the same period of anesthesia, immediately after blocking the inferior vena cava. In 15 cases, local anesthesia was chosen, associated with superficial sedation, and for the remaining 9 patients local anesthesia alone was used.
The access was by venous puncture in all cases. This was most commonly performed through the femoral vein contralateral to the limb affected by the thrombosis (43 patients). For the remaining 7 patients, the access was by puncture of the internal jugular vein.
The filters used were: LGM-VenaTech® (B-Braun) in 23 cases, Greenfield® (Boston Scientific) in 17 cases, and TrapEase® (Johnson & Johnson) in 10 cases.
Full anticoagulant treatment using low molecular weight heparin and vitamin K antagonists was reintroduced as soon as the contraindication for this ceased to exist.
The follow-up was performed clinically and by means of imaging examinations, with preference for duplex scanning of the vena cava, every 6 months during 5 years. If the patients underwent computerized tomography of the abdomen due to oncological indication and the image of the vena cava was satisfactory, the ultrasound examination was not requested.
We analyzed the implantation success rate exclusively related to the operative procedure, the immediate and late complications, and also the length of survival during the follow-up period of up to 60 months.
RESULTSThe implantation of the filter was adequate in all 50 cases, and this was proven by performing control cavography after releasing the device. There were no immediate complications from the procedure, which could have included venous perforation, hematomas of the retroperitoneum or puncture location, pneumothorax, arterial punctures, embolization, or inadequate positioning of the filter.
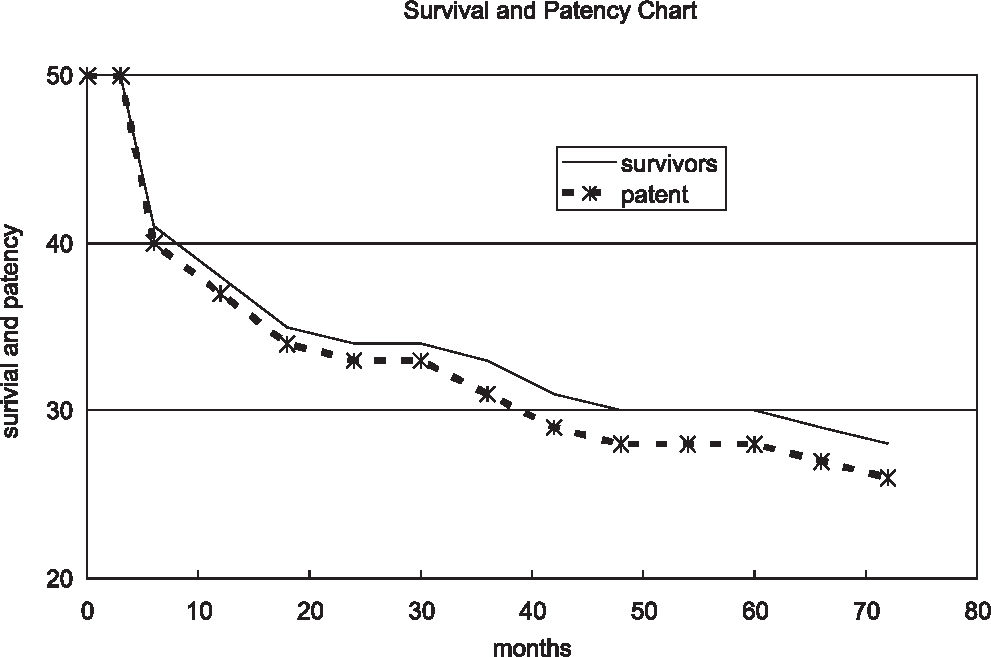
In the patients who underwent the procedure, we observed nonfatal pulmonary thromboembolism despite the presence of the filter in 1 patient, 2 cases of occlusion of the inferior vena cava, and the presence of a thrombus retained in the filter in 1 patient. There was no late migration of the filter. During the follow-up period of the study twenty patients (40% of the total) died. The cause of death was progression of the neoplasia in all cases. The length of survival, considering all 50 patients, was from 3 to 1824 days, with a median of 496 days, during the 5 years follow-up period (Figure 1).
DISCUSSIONSince 1944, when Homans14 described the ligature of the inferior vena cava as prophylaxis for pulmonary embolism, there has been much progress in the techniques for blocking the vena cava. Techniques have progressed from extraluminal procedures for vein interruption using plication and clips15 to the creation of intraluminal filters.16
Over the last few years, a consensus has been building up in the literature for the indication of the implantation of an inferior vena cava filter in cases in which anticoagulation treatment is contraindicated, or for patients who had pulmonary thromboembolism during full anticoagulation treatment.17,18,19 Recently, however, with the development of endovascular materials and techniques, there has been an even greater willingness to indicate this procedure.20,21 Some authors, such as Cohen22 and Calligaro,23 have proposed implantation of such filters as the first-choice method for oncological patients with DVT. Such proposals have also been based on studies that have demonstrated that these patients are at greater risk of hemorrhagic events than nononcological patients.24,25 Nevertheless, in these studies, most of the cases that evolved with bleeding presented an INR (international normalized ratio) greater than the proposed therapeutic levels (up to 3.0) at the time when the hemorrhage occurred. Thus, our understanding is that this is a very radical stance, and we do not share these authors’ opinion.
Most of the patients who underwent implantation of an inferior vena cava filter in our sample had a temporary contraindication for anticoagulant treatment during the intraoperative and immediate postoperative periods. Once the risk of bleeding secondary to the operation had been reduced, we reintroduced low molecular weight heparin and subsequently vitamin K antagonists, in spite of the presence of the filter. Other situations in which we indicated the procedure were when pulmonary thromboembolism occurred during full anticoagulant treatment and when it greatly affected pulmonary function. In this latter situation, a new episode of embolism could be fatal, even if the embolus were small. These indications are compatible with those used in other centers, according a number of reports.16,17,18,19
We believe that oncological patients should be followed even more closely with regard to anticoagulation control, since they often present clinical conditions that may interfere with the action of the anticoagulant. However, we believe that anticoagulant treatment using low molecular weight heparin or, whenever possible, vitamin K antagonists should be the first choice in treating such patients. The aim would be not only to reduce the risk of pulmonary embolism, but also to have a lower repercussion from the venous thrombosis for the affected limb. We reserve the implantation of a vena cava filter for individuals who are unable to receive any type of anticoagulant drug.
The blocking of the inferior vena cava using an intraluminal filter was successfully performed in all the patients. There were no large- or small-scale complications, and this is in keeping with the findings from other published series.19,26,27,28
The high rate of patient handling under general anesthesia was due to the fact that, in 16 cases, the implantation of the filter was on the same occasion as a large-scale operation necessarily conducted under this type of anesthesia. When the blocking of the inferior vena cava was independently performed, local anesthesia concomitant with light sedation was preferred, so as to decrease the scale of anesthesia without causing discomfort to the patient. Only when sedation was not possible (non-observance of 8 hours of fasting, or poor clinical condition) did we use local anesthesia alone; in these cases, infiltration of 2% lidocaine at the puncture location was employed. Wilson et al 21 also used local anesthesia for the implantation of vena cava filters for prophylaxis of pulmonary embolism in patients who had suffered a traumatic spinal cord lesion.
There is no consensus in the literature regarding which route is most suitable for implanting the vena cava filter. Some authors have advocated puncture of the internal jugular vein,17,29,30 while others have preferred puncture of the femoral vein.28 In the majority of our cases (86%), we performed the procedure by puncture of the femoral vein contralateral to the limb affected by the DVT, with the aim of avoiding the risks associated with puncture of the subclavian or jugular vein (hemopneumothorax and cervical hematoma). At the time of writing, we are also performing the procedure by puncture of the internal jugular vein, using smaller caliber (6 Fr) insertion devices, if central venous access is required for the patient. In such cases, the catheter is positioned before removing the insertion device.
After implanting the filter, we performed a clinical and radiological follow-up using duplex scanning of the vena cava every 6 months. The exception to this occurred whenever a patient underwent computerized tomography of the abdomen due to an oncological indication, provided that such examination gave an adequate image of the vena cava, thus allowing us to verify the position of the device and the patency of the vessel.
There is no defined standard for following up patients with implanted vena cava filters. Such a follow-up can be performed clinically, or with the aid of imaging examinations, such as a simple radiography of the abdomen, or duplex scanning.16,31,32
When the factor that gave rise to the contraindication for full anticoagulant treatment had been overcome, we reintroduced anticoagulant drugs (low molecular weight heparin and/or warfarin), in spite of the presence of the filter. We believe that this leads to lower rates of rethrombosis, thrombosis of the vena cava, or pulmonary embolism, and this is corroborated in the literature.17,27
In our sample, we documented 1 case (0.5%) of symptomatic pulmonary thromboembolism. This is a lower rate than reported from other centers, where the rate has ranged from 2.5% to 33%.16,17,19,27,30,33 We also recorded 1 patient (0.5%) with thrombus retained in the filter and 2 patients (1%) with thrombosis of the inferior vena cava. These rates are much lower than found in some series: 10% to 22% and 7% to 24%, respectively.19,27,30,33 It should be borne in mind that occlusion of the inferior vena cava could be considered to be a complication, possibly due to the presence of the foreign body in the lumen of the vessel, but it may also signify therapeutic success (retention of the thrombus), independent of whether the thrombus has a central or marginal position. No filter migrated in our patients, while such an occurrence may be found at a rate of more than 20%, in other reports.27,30
The large number of patients who died can be explained by considering the fact that our sample consisted of patients with cancer that were mostly at an advanced stage, and thus these were individuals with a low life expectancy. It is emphasized that none of the 20 deaths could be attributed to the procedure of implanting the filter or to being a consequence of pulmonary thromboembolism, therefore showing the efficacy of the method. Schleich et al,34 in a prospective follow-up study of 100 patients who had undergone implantation of an inferior vena cava filter, also observed that the mortality was greater among those with cancer.
CONCLUSIONImplantation of an inferior vena cava filter by an endoluminal route was shown to be a safe and efficient method for preventing pulmonary embolism in cancer patients with DVT.