Prediabetes is a high-risk state for diabetes. The study aims to describe routine clinical practice and the views of physicians and pharmacists on prediabetes management.
Materials and methodsAn observational, descriptive, cross-sectional study was conducted using a structured questionnaire.
ResultsA total of 410 physicians and 393 pharmacists completed the questionnaire. Self-adherence to clinical practice guidelines (CPGs) was reported by 51.5% and 23.2% of physicians and pharmacists, respectively. Less than 60% of participants defined prediabetes according to main CPG. Regarding the use of screening strategies to detect prediabetes (physicians: 96%; pharmacists: 42.1%), reports indicate the opportunistic strategy is widely employed (≥75%) whereas systematic screening is unusual (<20%). Changes in lifestyle were deemed essential by almost all participants (≥95%), but in clinical practice only 58.3% of healthcare centers and 28.0% of pharmacies were found to provide awareness-raising/instruction. The role of pharmacists in the prevention of prediabetes/diabetes was judged useful by most participants.
ConclusionsUse of CPG, systematic prediabetes screening strategies, and specific strategies for patient education are scarce. The support of community pharmacists in prediabetes management was well valued. Therefore, it is crucial that the lines of action followed by both physicians and pharmacists align with each other and with the CPG.
La prediabetes es un estado de alto riesgo para la diabetes. El objetivo del estudio es describir la práctica clínica habitual y las opiniones de médicos y farmacéuticos sobre el manejo de la prediabetes.
Materiales y métodosSe realizó un estudio observacional, descriptivo y transversal mediante un cuestionario estructurado.
ResultadosContestaron al cuestionario 410 médicos y 393 farmacéuticos. El 51,5% y el 23,2% de los médicos y los farmacéuticos, respectivamente, comunicaron que seguían las guías de práctica clínica (GPC). Menos del 60% de los participantes definieron la prediabetes según la GPC principal. En cuanto al uso de estrategias de cribado para detectar la prediabetes (médicos: 96%; farmacéuticos: 42,1%) los informes indican que se utiliza ampliamente la estrategia oportunista (≥75%), mientras que el cribado sistemático es poco habitual (<20%). Casi todos los participantes (≥95%) consideraban esenciales los cambios en los hábitos de vida, pero en la práctica clínica solo el 58,3% de los centros sanitarios y el 28,0% de las farmacias concienciaban o facilitaban formación. La mayoría de los participantes consideraban útil la función de los farmacéuticos en la prevención de la prediabetes/diabetes.
ConclusionesEl uso de GPC, estrategias sistemáticas de cribado de la prediabetes y estrategias específicas para la educación de los pacientes es escaso. Se valoraba bien el apoyo de los farmacéuticos comunitarios en el manejo de la prediabetes. Así pues, es crucial que las líneas de acción seguidas por médicos y farmacéuticos se alineen entre sí y con las GPC.
Prediabetes is a high-risk state for diabetes. It is defined by glycemic variables above normal, but lower than type 2 diabetes mellitus (T2DM) thresholds.1
Prediabetes refers to individuals with impaired glycated hemoglobin (HbA1c) levels, impaired fasting glucose (IFG) and/or impaired glucose tolerance (IGT). These individuals have a high risk of developing diabetes and cardiovascular disease.2
Prediabetes definition according to IGT (evaluated by 2-h 75g oral glucose tolerance test (OGTT)) is similar among the main clinical practical guidelines (CPG) such as those of the World Health Organization3 (WHO), the American Diabetes Association4 (ADA), the National Institute of Health and Care Excellence5 (NICE), and the Spanish Diabetes Society6 (Sociedad Española de Diabetes (SED)). However, there is currently no consensus definition for prediabetes based on IFG or HbA1c among these CPG.
It has been demonstrated that over a period of 3–5 years, about 25% of prediabetic individuals progress to T2DM while 25% return to a normal state of glucose tolerance and 50% remain in the prediabetic state.7 Progression to T2DM can be minimized using adequate prevention strategies such as dietary intervention and physical activity to ensure weight loss.8 Therefore, early detection of prediabetic states will help to promote prompt strategies to reduce the risk of developing T2DM.9 The implementation of screening programs, together with the early management of prediabetes and previously unrecognized diabetes, are both cost-effective and cost-saving from the healthcare perspective.10
In Spain, screening is mainly performed by physicians; however, community pharmacists, who maintain constant contact with patients, could play an important role both in screening and in promoting healthy lifestyles. In fact, previous initiatives carried out in Spain involving community pharmacists have reported positive results in the detection of prediabetes and diabetes,11–15 nevertheless, there is little evidence on the actual clinical practice followed by either group.
For this reason, the Detecta2 study aims to describe the routine clinical practice and the views of physicians and pharmacists with respect to the management of prediabetes within the Spanish healthcare system. In addition, we also describe the perception of the pharmacist's role in achieving this purpose.
Material and methodsStudy designAn observational, descriptive, cross-sectional study, based on a structured ad hoc questionnaire, was conducted between May and November 2018. A scientific committee comprising two diabetes experts (one physician and one community pharmacist) elaborated the ad-hoc questionnaire based on the results of a literature review on physicians’ and pharmacists’ perception and clinical practices in prediabetes management.
The questionnaire was composed of 34 items, organized in 5 sections, to explore perceptions and routine clinical practices: (1) use of guidelines for the management of prediabetes; (2) definition of prediabetes; (3) screening and detection strategies; (4) processing of patient information/education; and (5) role of pharmacists in prediabetes prevention. Additionally, physicians were asked about screening and detection methods used in clinical practice and their frequency of use. The questionnaire included open and closed-ended questions (dichotomous or multiple choice), numerical rating scales (from 0 to 10) and 5-point Likert-scale questions (from disagree to strongly agree).
Participants’ sociodemographic variables (age and gender) and professional characteristics (specialty, length of time practicing the specialty, number of patients attended in practice daily, Spanish region of practice and type of area) were also recorded.
An electronic form was used to collect physicians’ data, while face-to-face or telephone interviews were used to gather community pharmacists’ information.
ParticipantsParticipants were selected according to the following inclusion criteria: (1) physicians practicing in the Spanish public health sector, with at least 2 years’ experience in their specialty; and (2) community pharmacists with a minimum of 2 years of experience in the field of the Spanish community pharmacy.
In order to ensure the study population was a representative sample, the estimation of population size was based on the assumption of maximum uncertainly with a 95% confidence interval and 5% precision. The calculation included the number of primary-care physicians, endocrinologist, and internists who practice within the Spanish public healthcare system,16 and the number of community pharmacies.17 As a result, the minimum required sample size was estimated at 381 physicians and 378 community pharmacists.
Statistical analysisAbsolute and relative frequencies were calculated to describe qualitative variables. Means, standard deviations (SD), and interquartile range (IQR) were calculated to express quantitative variables. Quantitative variables were compared using Student's t test or equivalent methods for non-parametric variables. Data analysis was performed using STATA version 14 statistical software. For all statistical tests, p<0.05 was considered as statistically significant.
There is currently no consensus definition for prediabetes among main national (SED) and international CPGs (ADA, WHO and NICE), therefore we estimated the percentage of participants who defined prediabetes according to these CPGs. A deviation of one unit or less between the threshold (upper and lower) set by the participant and the threshold defined by the CPGs was considered correct. In addition, the mean percentage was calculated for the deviation between the range established by the participants and that defined in the guidelines.
Ethical considerationsThe Clinical Research Ethics Committee of the Hospital Universitario Puerta de Hierro (Madrid) was consulted prior to conducting the survey. Since the study consisted of an opinion questionnaire addressed to healthcare professionals, the Clinical Research Ethics Committee considered that ethical approval was unnecessary. All participants received appropriate information on the study and agreed to participate. To ensure data confidentiality, all documents were duly encoded.
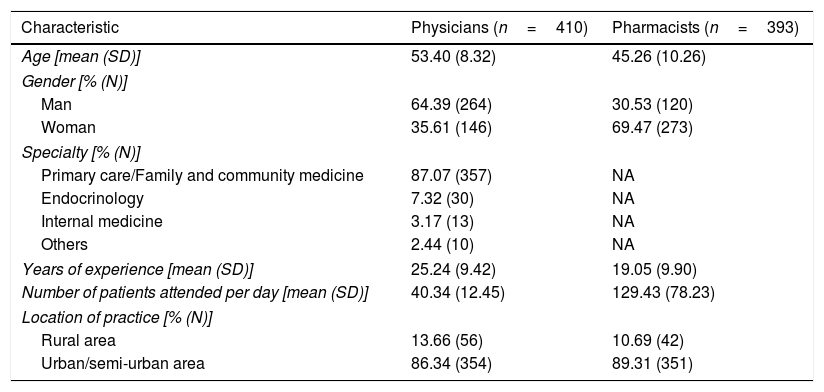
ResultsA total of 426 physicians and 469 pharmacists from all Spanish regions were invited to participate in the study. Of these, 96.2% of physicians (n=410) and 83.8% of pharmacists (n=393) completed the questionnaire. All of them, were highly experienced in diabetes management, reporting a mean experience of 25.2 (SD 9.4) and 19.1 (SD 9.9) years, respectively. Sociodemographic characteristics of study participants are shown in Table 1.
Sociodemographic characteristics of participants.
| Characteristic | Physicians (n=410) | Pharmacists (n=393) |
|---|---|---|
| Age [mean (SD)] | 53.40 (8.32) | 45.26 (10.26) |
| Gender [% (N)] | ||
| Man | 64.39 (264) | 30.53 (120) |
| Woman | 35.61 (146) | 69.47 (273) |
| Specialty [% (N)] | ||
| Primary care/Family and community medicine | 87.07 (357) | NA |
| Endocrinology | 7.32 (30) | NA |
| Internal medicine | 3.17 (13) | NA |
| Others | 2.44 (10) | NA |
| Years of experience [mean (SD)] | 25.24 (9.42) | 19.05 (9.90) |
| Number of patients attended per day [mean (SD)] | 40.34 (12.45) | 129.43 (78.23) |
| Location of practice [% (N)] | ||
| Rural area | 13.66 (56) | 10.69 (42) |
| Urban/semi-urban area | 86.34 (354) | 89.31 (351) |
SD, standard deviation. NA, not applicable.
Most participants stated that CPG are useful for the management of prediabetes in clinical practice (physicians: 87.6%; pharmacists: 83.7%). However, only 51.5% of physicians and 23.2% of pharmacists reported self-adherence to CPG, being ADA (39.8%) and SED (52.7%) the most frequently used, respectively.
Definition of prediabetesBoth physicians and pharmacists considered prediabetes a pre-disease stage (75.6% and 78.4%, respectively), which is underdiagnosed (93.4% and 82.4%) and represents a public health problem (90.9% and 89.1%).
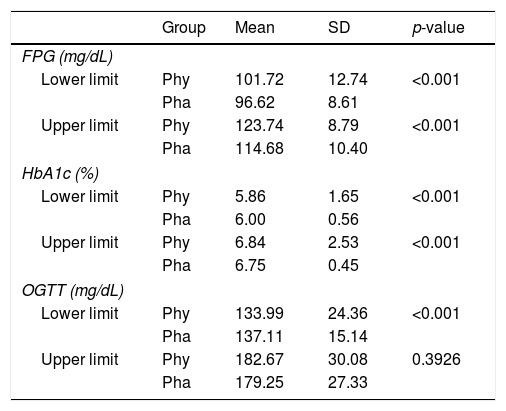
Heterogeneity was observed concerning prediabetes definition among physicians and pharmacists. In this respect, FPG levels to define prediabetes were significantly higher for physicians than for pharmacists (101.7–123.7mg/dL vs. 96.6–114.7mg/dL; p<0.001). The range of HbA1c levels was significantly wider (5.9–6.8% vs 6.0–6.7%; p<0.001). The range of OGTT levels was wider, but only differed significantly for the minimum threshold (134.0–182.7mg/dL vs. 137.1–179.3mg/dL; p<0.001) (Table 2).
Definition of prediabetes.
| Group | Mean | SD | p-value | |
|---|---|---|---|---|
| FPG (mg/dL) | ||||
| Lower limit | Phy | 101.72 | 12.74 | <0.001 |
| Pha | 96.62 | 8.61 | ||
| Upper limit | Phy | 123.74 | 8.79 | <0.001 |
| Pha | 114.68 | 10.40 | ||
| HbA1c (%) | ||||
| Lower limit | Phy | 5.86 | 1.65 | <0.001 |
| Pha | 6.00 | 0.56 | ||
| Upper limit | Phy | 6.84 | 2.53 | <0.001 |
| Pha | 6.75 | 0.45 | ||
| OGTT (mg/dL) | ||||
| Lower limit | Phy | 133.99 | 24.36 | <0.001 |
| Pha | 137.11 | 15.14 | ||
| Upper limit | Phy | 182.67 | 30.08 | 0.3926 |
| Pha | 179.25 | 27.33 | ||
SD, standard deviation. FPG, fasting plasm glucose. HbA1c, glycated hemoglobin. OGTT, oral glucose tolerance test. Phy, physicians. Pha, pharmacists.
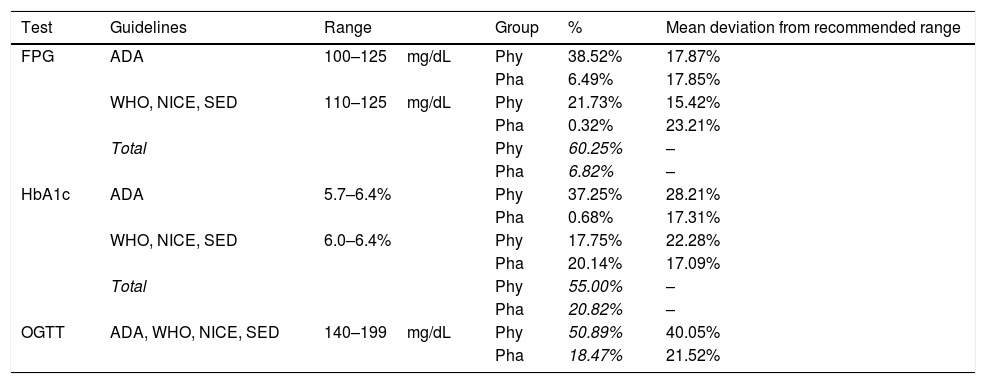
Based on these responses, almost half of physicians defined prediabetes in accordance with some of the main CPGs (ADA, WHO, NICE, SED): FPG (60.3%), HbA1c (55.0%) and OGTT (50.9%). On the other hand, a lower percentage of pharmacists’ responses fitted within the ranges given by the CPGs: FPG (6.8%), HbA1c (20.8%) and OGTT (18.5%) (Table 3).
Definition of prediabetes according to the main CPG.
| Test | Guidelines | Range | Group | % | Mean deviation from recommended range |
|---|---|---|---|---|---|
| FPG | ADA | 100–125mg/dL | Phy | 38.52% | 17.87% |
| Pha | 6.49% | 17.85% | |||
| WHO, NICE, SED | 110–125mg/dL | Phy | 21.73% | 15.42% | |
| Pha | 0.32% | 23.21% | |||
| Total | Phy | 60.25% | – | ||
| Pha | 6.82% | – | |||
| HbA1c | ADA | 5.7–6.4% | Phy | 37.25% | 28.21% |
| Pha | 0.68% | 17.31% | |||
| WHO, NICE, SED | 6.0–6.4% | Phy | 17.75% | 22.28% | |
| Pha | 20.14% | 17.09% | |||
| Total | Phy | 55.00% | – | ||
| Pha | 20.82% | – | |||
| OGTT | ADA, WHO, NICE, SED | 140–199mg/dL | Phy | 50.89% | 40.05% |
| Pha | 18.47% | 21.52% | |||
SD, standard deviation. FPG, fasting plasm glucose. HbA1c, glycated hemoglobin. OGTT, oral glucose tolerance test. Phy, physicians. Pha, pharmacists. ADA, American Diabetes Association. WHO, World Health Organization. NICE, National Institute of Health and Care Excellence. SED, Spanish Diabetes Society.
Most participants (physicians: 97.3%; pharmacists: 94.7%,) stated that screening for prediabetes helps increase its detection. Nearly 60% of physicians and 70% of pharmacists considered that screening should be universal regardless of blood glucose levels.
While most of physicians (96.0%) reported the use of screening strategies to detect prediabetes only 42.1% of pharmacists reported their use. The opportunistic strategy was found to be the most widely employed (physicians: 76.1%; pharmacists: 97.5%) whereas the use of systematic screening was unusual (physicians: 19.9%; pharmacists: 2.5%).
Nonetheless, 61.7% of physicians reported implementation of screening strategies in their healthcare facilities to identify people at risk of developing diabetes, being the Finnish Diabetes Risk Score (FINDRISC)18 the most frequently used method (69.6%). In this respect, most participants considered that among different screening test the FINDRISC18 was the most appropriate (physicians: 80.5%; pharmacists: 77.5%).
Half of the participants indicated that if neither prediabetes nor diabetes was diagnosed, they would repeat the screening test every year (regardless of diabetes risk) while 43.2% reported repeating it every 4 years for low-risk individuals and every year for high-risk individuals.
Among the reasons for not using screening strategies, the most frequently reported was the lack of time by both physicians (58.8%) and pharmacists (72.8%), followed by the lack of resources (23.5% and 33.5%, respectively).
DetectionMost physicians (96.8%) and pharmacists (91.6%) stated that detection of prediabetes helps prevent the development of diabetes. To confirm prediabetes and diabetes physicians and pharmacists preferred FPG test (73.9% and 74.5%, respectively), and the use of HbA1c (78.8% vs 46.7%; p<0.001), in contrast to OGTT (31.0% vs 9.4%; p<0.001). This trend is in line with the routine clinical practice where FPG test (88.9%) and HbA1C (85.5%) levels are the most widely used by physicians. In the event that prediabetes was detected, 85.4% of physicians and 93.4% of pharmacists would advise a second confirmatory test, stating preference for HbA1c (physicians: 72.9%; pharmacists: 76.9%).
The risk factors considered most important by physicians and pharmacists for considering screening or detection test were: obesity; impaired fasting glucose; family history of diabetes in first degree relatives; vascular complications, and prior gestational diabetes (mean score >8 on a scale from 0 to 10).
TreatmentStudy results showed that physicians (41.5%) and pharmacists (40.5%) considered that prediabetes diagnosis may lead to overtreatment of the condition.
However, in general, less than 15% of them considered metformin (or other drugs) adequate for treating prediabetes, except for obese individuals (BMI≥35kg/m2) (physicians: 54.6%; pharmacists: 20.4%). In contrast, changes on lifestyle were deemed essential for prediabetic people by almost all participants (physicians: 97.6%; pharmacists: 99.2%). Natural therapies were considered an option for some pharmacists (23.9%) and physicians (9.0%).
Patient information/educationMost physicians and pharmacists considered that inadequate information available to people with prediabetes may result in an increased risk of developing diabetes (percentile 25≥7; i.e., more than 75% of participants assigned a score of at least 7 points on a scale from 0 to 10).
Despite this, respondents reported that in clinical practice 58.3% of healthcare centers and 28.0% of pharmacies have procedures in place to inform/instruct people about their prediabetes. In particular, most information is tailored to each patient (physicians: 84.5%; pharmacists: 75.5%) and is provided verbally (physicians: 93.3%; pharmacists: 60.9%) in individual sessions with the patient (physicians: 92.9%; pharmacists: 90.9%). Among the reasons for not having informative procedures in place, they reported lack of time (physicians: 75.4%; pharmacists: 61.0%) and lack of resources (physicians: 67.8%; pharmacists: 35.3%). In relation to the issues that patients should be informed about, most respondents considered that it is very important to raise patients’ awareness about healthy lifestyles (diet and exercise), the risk of developing diabetes and the importance of adherence to professional recommendations (percentile 25≥8).
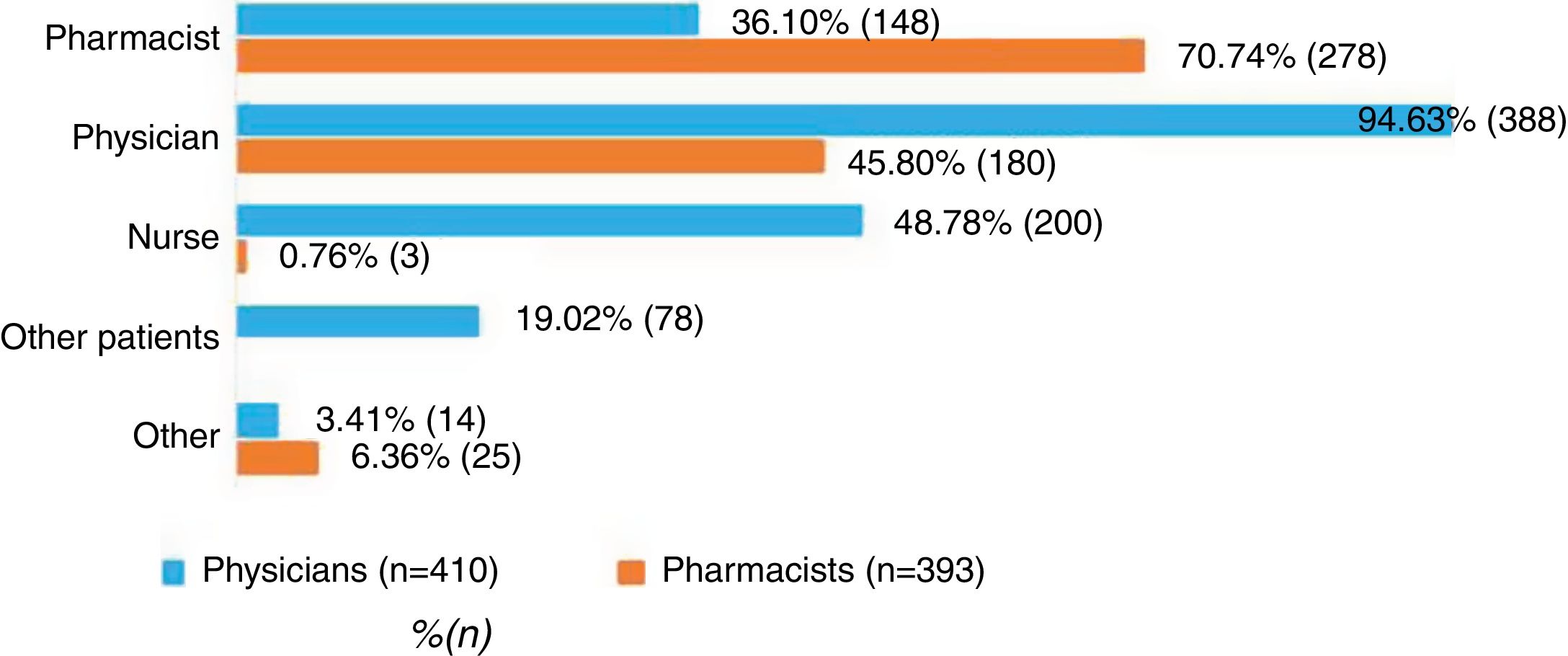
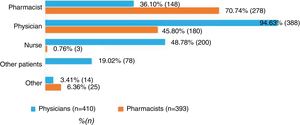
Respondents were consulted about who should inform/instruct prediabetes patients. Seventy point seven percent of the pharmacist and 94.6% of the physicians consider their own specialty as the most suitable for informing patients. Furthermore, 45.8% of pharmacist consider physicians should also participate, while 36.1%, 48.8%, and 19.0% of physicians consider that the pharmacist, nurses and other patients should be involved, respectively (Fig. 1).
Role of pharmacists in prediabetes preventionParticipants were asked about the role of community pharmacists in detecting prediabetes or diabetes and improving patients’ adherence to healthy lifestyles and pharmaceutical recommendations. In general, it was considered positively by most physicians and pharmacists (P25>6). This active role of pharmacists in the prevention of prediabetes/diabetes was judged more useful by pharmacists than by physicians for: 1) prediabetes detection (6.0 vs 7.0; p<0.001), diabetes detection (6.5 vs 8.0; p<0.001), detection of people at risk of developing diabetes (6.0 vs 7.0; p<0.001) and improved adherence to hygienic-dietary and/or pharmaceutical recommendations (6.0 vs 7.0; p<0.001).
DiscussionIn Spain, almost half of diabetics are unaware they have the disease.19 This fact, together with the prevalence of diabetes and prediabetes in the Spanish population (13.8% and 14.8% respectively),19 highlight the importance of early detection.
Our study provides information on physicians’ and pharmacists’ knowledge and attitude toward diabetes screening and detection guidelines and also provides evidence on their adherence to these guidelines as well as how they conduct clinical practice.
There is evidence to suggest that those physicians who adhere to CPG deliver better outcomes for their patients.20,21 In our study, more than 80% of participants considered CPG useful for the management of prediabetes, but only 50% of physicians and 25% of pharmacists acknowledge that they use them. As a result, when participants were asked to define prediabetes, less than 60% of physicians and 25% of pharmacists were within the ranges given by the main CPG for FPG, HbA1c and OGTT. Findings show there is a gap between pharmacists’ perceptions of adherence to the guidelines and their actual knowledge. This difference is less evident in the case of physicians, although differences between physicians’ reported self-adherence to diabetes screening CPG and their actual practice have previously been reported in the literature.22
Most participants stated that prediabetes screening improves its detection, but this practice is only a widespread among physicians. For those physicians and pharmacists who do screening tests, opportunistic tests were the most widely used screening strategy. In this regard, CPG state that opportunistic screening of risk groups, as well as two-stage screening using the FINDRISC18 can contribute to detecting cases of prediabetes. Although benefits in terms of morbidity and mortality have not been demonstrated, screening can contribute to preventing diabetes and probably its chronic complications.6 Despite participants’ agreement with this, surprisingly, only 20% of physicians reported using systematic strategies although 60% of them stated its use in their healthcare facility. This difference could be explained by the over-representation of family doctors or due to using these questionnaires in a non-protocolized manner.
FINDRISC18 is the most frequently used for screening, and FPG and HbA1c for detection. Regarding screening frequency, although there is no consensus, in general the main CPG recommend screening every 3–5 years, or even annually in high-risk patients. In our study, almost half of the physicians found this frequency adequate. However, the other half considered that it should be annual in all cases. In this context, the availability of online (self-administered) questionnaires and/or the assistance of the community pharmacist could facilitate their regular use.
Previous evidence suggests that conversion from IGT to T2DM can be delayed or avoided by a diet- and exercise-based treatment regimen, resulting in reductions in diabetes risk ranging from 28% to 67%,6 and the cost-effectiveness of these non-pharmacological interventions has been demonstrated.8,23 For this reason, healthy lifestyles (i.e. diet and exercise) are recommended by all CPG. In general, our study participants (>75%) considered that inadequate information available to prediabetic individuals might increase their risk of developing diabetes; however, they reported that under 60% of healthcare centers and below 30% of pharmacies follow procedures to inform people about their prediabetes. Similar results have been found in previous studies. Gess et al. reported that half of those identified as high-risk via primary care practices in the UK were not informed of their risk status, and a third were not aware of the role of diet and exercise in risk reduction.24 Similarly, data from the National Health and Nutrition Examination Survey (USA) showed that only one third of prediabetic individuals had received lifestyle recommendations from their physicians.25,26
Despite the proven benefits of diet and exercise in preventing diabetes, lifestyle interventions are difficult for patients to maintain and, in some cases, not possible (e.g. due to disability or medical reasons).27 Several studies suggest that addressing incentive approaches (e.g. pedometers) or pharmacological interventions in high risk individuals may reduce the progression of diabetes compared to standard lifestyle advice.23,27 However, in Europe no drugs are currently indicated (according to the technical data sheet) for the prevention of diabetes. Notwithstanding, different CPG suggest metformin treatment for prediabetic individuals in certain cases. The ADA supports metformin treatment in very high-risk prediabetic individuals: severe obesity (BMI≥35kg/m2), history of gestational diabetes and under 60 years of age. Similar recommendations are established by the SED when lifestyle modification has failed, while NICE suggests its use when lifestyle change programs are not possible. Metformin was considered suitable for obese prediabetic individuals by nearly half of the physicians who participated in our study. However, very few pharmacists believed metformin treatment was adequate in any case.
More than 40% of the participants considered that prediabetes diagnosis may lead to overtreatment of the condition. This perception is not supported by previous studies, where metformin use in prediabetes has been reported, being less than 1% among U.S. adults with prediabetes and only slightly more common among those with additional risk factors for diabetes.28
The role of community pharmacists in detecting prediabetes or diabetes and in improving patients’ adherence to healthy lifestyles and pharmaceutical recommendations was considered positively by most of participants. This finding is in line with previous studies, which highlight the relevance and excellent position of community pharmacies in the screening, monitoring and education of patients, thereby contributing to preventing disease complications.11–15 The incorporation of follow-up and education programs and interventions in community pharmacies has been shown to increase patient responsibility concerning their disease and its treatment, highlighting the key role of the pharmacist in patient follow-up.12 Interestingly, opinions clashed in that physicians stated that they should be the primary agents to provide patient information, while pharmacists held the opposite view. In fact, there is growing evidence that, through a range of extended services, pharmacists may contribute positively to the clinical and humanistic outcomes of diabetic patients, and also indicate that these services can be delivered cost-effectively.29
This study has several limitations: (1) ad hoc questionnaires are not standardized; (2) most questions included in the questionnaire were closed-ended, which may hamper the interpretation of participants’ perceptions; (3) the included participants had a mean of 25 years of experience in the case of physicians, and 19 years in the case of pharmacists, which could lead to some bias in the extrapolation of results; (4) the number of endocrinologist and internist participating in the study was low compared to the other specialties; and finally, (5) caution should be exercised when considering the extrapolation of the present findings to other countries due to, for example, possible differences in the extent to which community pharmacists are involved in disease management.
ConclusionOur study shows that limited use of CPG has been found, which may explain the relatively low concordance between participants’ definition of prediabetes and that stated in the guidelines. Similarly, systematic prediabetes screening strategies are scarce, with FINDRISC test18 being the most widely used for prediabetes screening and FPG/HbA1C tests for prediabetes detection. Informing/instructing the prediabetic patient is considered essential to prevent the onset of diabetes. However, a relatively low proportion of professionals reported specific strategies aimed at raising patient awareness in their centers. In this respect, the role of the community pharmacist was valued positively as a support in the detection and management of prediabetes. To this end, it is crucial that the lines of action taken by both physicians and pharmacists align with each other and with the CPG.
FundingThis study was funded by BGP Product Operations S.L (Mylan) who had no role in the study design or data analysis and interpretation.
Conflict of interestJFN and JAF state they have no conflicts of interest. MKM, RdMM and LGM are Mylan employees. LL and dPHD work for an independent research organization (Outcomes’10, S.L.), which has received fees for its contribution to the development and coordination of the project and to the writing of this manuscript.