This study aimed to estimate the effectiveness of a comprehensive diabetes program (CDP) in terms of glycemic control, adherence, and the selection of candidates for sensor-augmented insulin pump therapy (SAP).
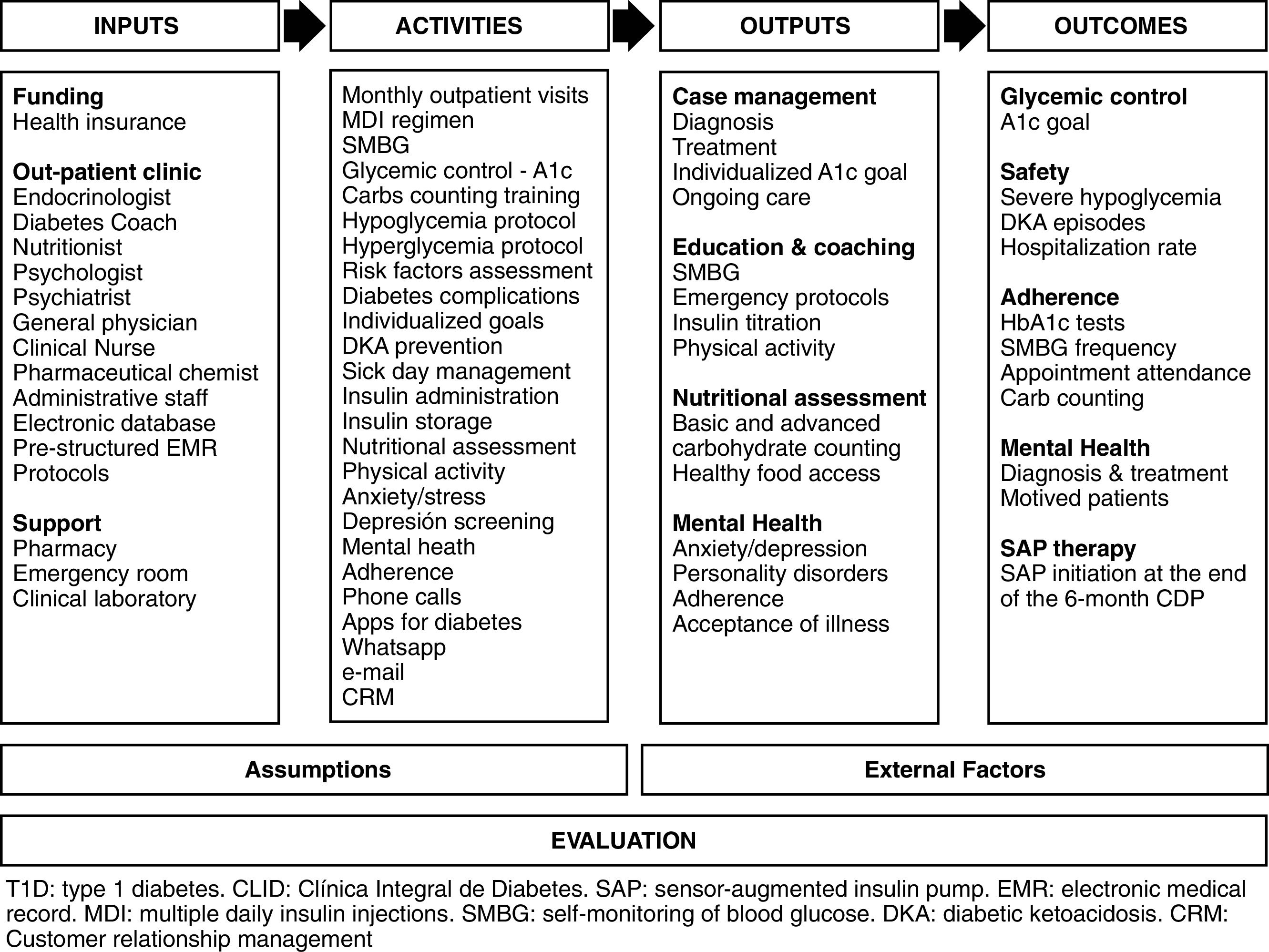
MethodsWe compared diabetes control before and 6 months after CDP. The program was based on disease management using a logical model dealing with the following: case management, education and coaching, nutritional assessment, and mental health.
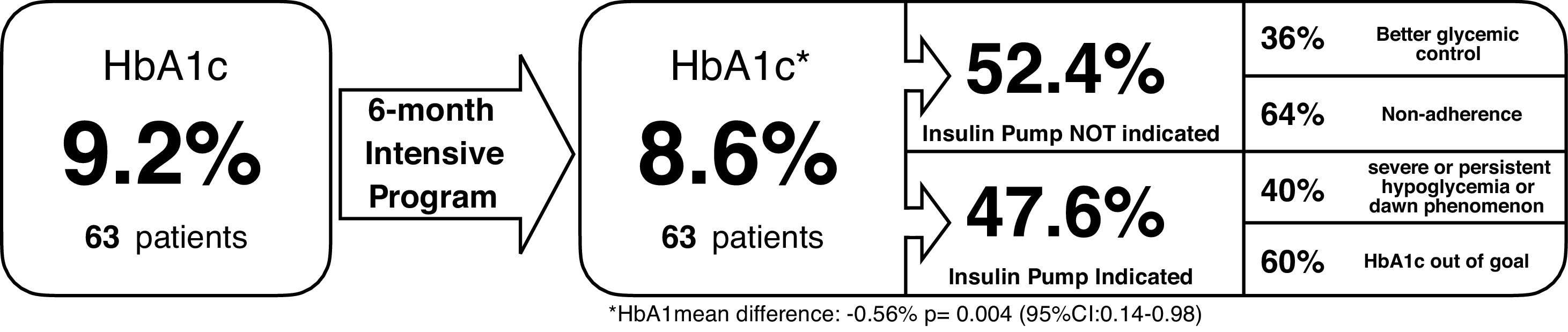
ResultsThe CDP improved glycemic control, HbA1c decreased by 0.56% (p-value=0.004; 95% CI: 0.14–0.98) and 19.1% of the patients reached the HbA1c goal without hypoglycemia. The CDP reduced by 52.4% the indication for SAP due to better glycemic control (36.4%) or non-adherence issues (63.6%); the remaining 47.6% persisted with poor glycemic control despite good adherence and were scaled to SAP. Among the 30 suitable candidates for SAP therapy, 60% did not reach the HbA1c goal and 40% had either hypoglycemic episodes (severe or persistent) or dawn phenomenon. The overall non-adherence rate was 33.3%.
ConclusionsCDP optimized the selection of suitable candidates for SAP by improving glycemic control and identifying adherence issues early. These results provide evidence of the impact of the implementation of patient selection and educational protocols in the real-life setting of a highly experienced clinic.
Este estudio tuvo como objetivo estimar la efectividad de un programa integral de diabetes (PID) en términos de control glucémico, adherencia y selección de candidatos para la terapia con bomba de insulina aumentada por sensor.
MétodosComparamos el control de la diabetes antes y 6 meses después del PID. El programa se fundamenta en la gestión de la enfermedad utilizando un modelo lógico, cuyas principales actividades fueron: manejo de casos, educación y entrenamiento, evaluación nutricional y salud mental.
ResultadosEl PID mejoró el control glucémico, la HbA1c disminuyó un 0,56% (p=0,004; IC 95%: 0,14-0,98) y el 19,1% de los pacientes alcanzaron la meta de HbA1c sin hipoglucemia. El PID redujo en un 52,4% la indicación de bomba de insulina aumentada por sensor, debido a un mejor control glucémico (36,4%) o problemas de no adherencia (63,6%), el 47,6% restante persistió con un mal control glucémico a pesar de una buena adherencia y fueron escalaron a terapia SAP. Entre los 30 candidatos ideales para SAP, el 60% no alcanzó la meta de HbA1c, y el 40% tuvo episodios de hipoglucemia (graves o persistentes) o fenómeno del alba. La tasa global de no adherencia fue del 33,3%.
ConclusionesEl PID optimizó la selección de candidatos ideales para la terapia con bomba de insulina aumentada por sensor al mejorar el control glucémico e identificar tempranamente los problemas de adherencia. Estos resultados proporcionan evidencia del impacto de la implementación de protocolos de selección y educación de pacientes bajo condiciones reales de una clínica altamente experimentada.
Sensor-augmented insulin pump therapy (SAP) which combines Continuous Subcutaneous Insulin Infusion (CSII) and real-time Continuous Glucose Monitoring (rtCGM) have been associated with better glycemic control without an increase in hypoglycemia when compared with multiple daily insulin injections (MDI) in patients who are appropriately educated and supported.1–3 Current guidelines from the American Association of Clinical Endocrinologists and American College Of Endocrinology – AACE/ACE and the Endocrine Society recommend its use over MDI in motivated patients with type 1 diabetes who have not achieved an A1c goal or who have achieved their A1c goal but continue to experience severe hypoglycemia or high glucose variability. Likewise, before initiating SAP or any other diabetes care technology, candidates should receive a thorough evaluation to assess patient's psychological status and a wide range of diabetes self-care behaviors that are likely to impact the adherence to therapy. In addition, it is suggested that patients starting or already utilizing CSII with or without sensor augmentation receive education, training, and ongoing support to help achieve and maintain individualized glycemic goal. However, due to the lack of high-quality comparative studies evaluating the effectiveness of educational protocols, no other recommendations regarding specific components and strategies for transitioning patients from MDI to CSII are made.4,5
There are numerous long-term studies that have indicated that the use of ambulatory CSII systems is associated with improved overall glycemic control as evidenced by lower HbA1c. However, whether the pump itself brings the observed benefits of CSII, or via the management that accompanies the pump, is still matter of debate. A systematic review that included five observational studies and no RCTs explored the effectiveness of educational components and strategies associated with insulin pump therapy, although it was unable to draw strong conclusions due to the small sample sizes, lack of control groups for comparisons, and the variability of methods, authors found that no educational method was significantly more effective than any other method.6 Despite the limitations of the available literature and the absence of strong consensus statement about which should be the components of education and training, protocols are relatively consistent in including: instructions for managing daily living and sick-day rules, using CSII, adjusting insulin doses, carbohydrate counting, preventing and managing hypoglycemia and diabetic ketoacidosis, and understanding the role of either self-monitoring blood glucose (SMBG) or rtCGM.
It is important to be aware that in clinical practice, initial training is often provided by insulin pump company employees or contracted consultants mainly for primary care settings, and less frequently performed at clinics with significant insulin pump experience and carefully applied protocols of patient selection and education in a long-term basis. In this regard, even less research has been conducted on evaluating the clinical impact of the selection criteria, educational approach, or ongoing evaluation and support that experienced health-care providers and clinics implement. The present study aimed to estimate the effectiveness of a Comprehensive Diabetes Program (CDP) in terms of glycemic control, adherence, and selection of candidates for Sensor-augmented insulin pump therapy (SAP) in patients with uncontrolled type 1 diabetes.
MethodologyA retrospective analytical observational study of patients with uncontrolled type 1 diabetes candidates for SAP therapy, comparing diabetes control before and 6 months after CDP was conducted at a reference center for diabetes (Clínica Integral de Diabetes – CLID) at Medellín, Colombia, between August 2015 to December 2016. Eligible patients were age 15 years or older, with uncontrolled diabetes, who were enrolled into an intensive follow-up program prior to decide whether or not starting on SAP therapy. Pregnant women were excluded. The indications for SAP therapy were established in accordance with institutional protocol based on guidelines recommendations: (1) poor glycemic control (HbA1c>7.5%) with MDI insulin regimen for the last six months, (2) dawn phenomenon, (3) frequent and/or symptomatic hypoglycemia, (4) diabetic gastroparesis, and (5) episodes of severe hypoglycemia. Relative contraindications for SAP include: unwilling patient, psychiatric disorder, inability to handle the pump, or non-adherence. Non-adherence was defined as infrequently SBMG (<4 times/day), less than 80% of appointment attendance, and not counting carbohydrates.
The program was based on the disease management concept. According to the Care Continuum Alliance (formerly the Disease Management Association of America), disease management “is a system of coordinated health care interventions and communications for populations with conditions in which patient self-care efforts are significant”. The overall structure and interventions of the CDP is summarized in the logic model shown in Fig. 1. During this 6-month intensive program, patients had monthly out-patient appointments of 30min duration with endocrinologist as well as direct communication with disease manager via e-mail, phone calls, text or SMS as needed. CDP also included at least four visits with nutritionist and diabetes coach each, and psychologist or psychiatrist as needed by only under medical indication.
The main outputs were: (i) case management, (ii) education and coaching, (iii) nutritional assessment, and (iv) mental health; through a broad brochure of nonpharmacologic strategies and activities as listed in the logic model. All patients were on treatment with multiple daily insulin injections and self-monitoring of blood glucose (SMBG). The primary outcome was the effectiveness of CDP in terms of HbA1c reduction, as well as the percentage of patients who achieved their individualized HbA1c goal at the end of the program. The secondary outcome was the CDP impact in terms of adherence and change in the indications for SAP before and after CDP. At the end of CDP, well-controlled patients were returned to their primary care physician or specialist who had referred the patient to the clinic considering scale to SAP therapy. Patients with adherence issues continued psychological support and were referred for psychiatric treatment as needed. Ideal candidates were finally stared on SAP.
Clinical data was extracted from a database containing information of pre-specified and systematically registered electronic medical record, and included sociodemographic variables (age, sex, educational level), anthropometric (height, weight, body mass index), comorbidities (hypertension, dyslipidemia, micro and macrovascular complications, heart failure, coronary artery disease, peripheral artery disease and cerebrovascular disease), diabetes (type, duration, and antidiabetic medications including type of insulin and oral agents). Qualitative variables were described as absolute and relative frequencies and quantitative variables presented as measures of central tendency and dispersion. The normal distribution of quantitative variables was evaluated using the Kolmogorov–Smirnov test. The percentage of patients with at least one episode of severe and non-severe hypoglycemia was obtained, at least one hospital admission for associated complications and acute decompensation of diabetes in the last year upon entering the program. The mean level of HbA1c at admission and at 6 months was compared using paired t-test. The level of significance of the hypothesis tests was <0.05 with 95% confidence interval. The study was previously approved by the Institutional Review Board at the Universidad Pontificia Bolivariana at Medellín, Colombia, and conducted in accordance with the ethical principles of the Declaration of Helsinki.
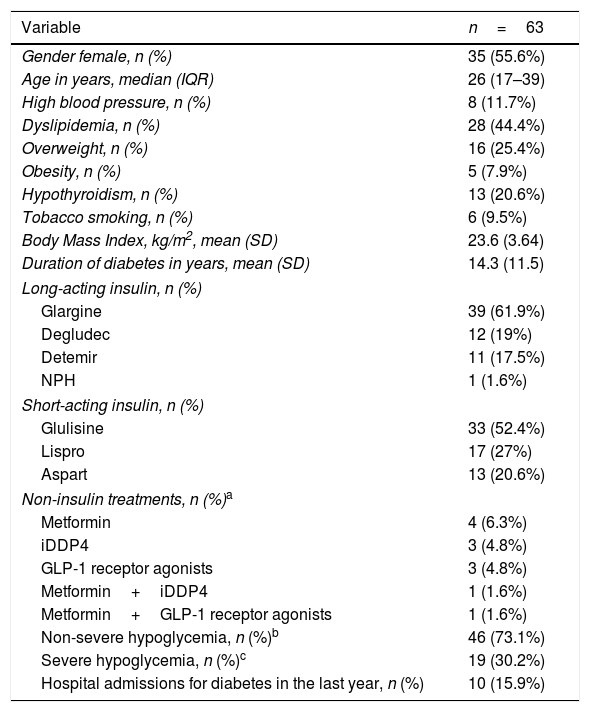
ResultsBaseline characteristics of the 63 patients with uncontrolled diabetes are presented in Table 1. Briefly, the median age was 26 years, with a HbA1c mean level of 9.2% (SD±1.9). In addition to insulin therapy, 12 patients (19%) had non-insulin medication, mainly metformin. All patients had health insurance by the Colombian contributive regime of health. Thirty five (55,6%) had a higher level of education followed by High school in 27 (42.8%), only one patients had none formal education. Regarding the chronicity and complications of the disease, the mean duration of diabetes was 14.3 (SD±11.5) years with micro and macrovascular complications reported in 20.6% and 3.2% of patients, respectively. Retinopathy in 9 (14.3%), nephropathy in 7 (11.1%), neuropathy in 5 (7.9%), coronary artery disease in 1 (1.6%), and stroke in 2 (3.2%) patients. Prior to the beginning of the 6-month CDP, 73.1% reported at least one non-severe hypoglycemia episode in the past 14 days, 30.2% with at least one severe hypoglycemia episode in the past year, and 15.9% of the patients were hospitalized due to diabetes in the last year, respectively. The main reasons for hospitalization were diabetic ketoacidosis (11.1%) and severe hypoglycemia (3.2%).
Baseline characteristics of 63 patients with uncontrolled type 1 diabetes.
| Variable | n=63 |
|---|---|
| Gender female, n (%) | 35 (55.6%) |
| Age in years, median (IQR) | 26 (17–39) |
| High blood pressure, n (%) | 8 (11.7%) |
| Dyslipidemia, n (%) | 28 (44.4%) |
| Overweight, n (%) | 16 (25.4%) |
| Obesity, n (%) | 5 (7.9%) |
| Hypothyroidism, n (%) | 13 (20.6%) |
| Tobacco smoking, n (%) | 6 (9.5%) |
| Body Mass Index, kg/m2, mean (SD) | 23.6 (3.64) |
| Duration of diabetes in years, mean (SD) | 14.3 (11.5) |
| Long-acting insulin, n (%) | |
| Glargine | 39 (61.9%) |
| Degludec | 12 (19%) |
| Detemir | 11 (17.5%) |
| NPH | 1 (1.6%) |
| Short-acting insulin, n (%) | |
| Glulisine | 33 (52.4%) |
| Lispro | 17 (27%) |
| Aspart | 13 (20.6%) |
| Non-insulin treatments, n (%)a | |
| Metformin | 4 (6.3%) |
| iDDP4 | 3 (4.8%) |
| GLP-1 receptor agonists | 3 (4.8%) |
| Metformin+iDDP4 | 1 (1.6%) |
| Metformin+GLP-1 receptor agonists | 1 (1.6%) |
| Non-severe hypoglycemia, n (%)b | 46 (73.1%) |
| Severe hypoglycemia, n (%)c | 19 (30.2%) |
| Hospital admissions for diabetes in the last year, n (%) | 10 (15.9%) |
Significant improvement was seen in glycemic control after 6 months of CDP, with an absolute reduction in HbA1c mean levels of 0.56% (p-value=0.004; 95% CI: 0.14–0.98). At the end of this intensive program, 19.1% patients reached their individualized HbA1c goal without hypoglycemia, 47.6% persisted with uncontrolled disease, and 33.3% were classified as non-adherent. Among the 30 ideal candidates for SAP therapy, 60% did not reach HbA1c goal and 40% had either hypoglycemic episodes (severe or persistent) or dawn phenomenon. Contrastingly, SAP therapy was not indicated in 33 patients (52.4%) due to a better glycemic control (36.4%) or non-adherence issues (63.6%) as shown in Fig. 2.
DiscussionThis is the first study we are aware of that assess the impact of a disease management program in the selection of ideal candidates for SAP therapy. We used the logic model as a tool for simplify complex relationships between various components of the program and outcomes as shown in Fig. 1. The logic model of CDP was based on a multidisciplinary and intensive approach for a proactive disease management before prescribing SAP therapy, as recommended by current guidelines.4,5 As a result, CDP identified 47.6% of patients as ideal candidates for SAP therapy, 33.3% as non-adherent, and 19.1% as well-controlled patients who achieved their HbA1c goal without severe or persistent hypoglycemic episodes. This means, 52.4% reduction of the initial candidates for SAP. These findings provide real-world evidence of the effectiveness of nonpharmacologic interventions (patient education, psychological support, dietary education, self-monitoring, and intensive coaching and monitoring) in selection of candidates for SAP or any other diabetes care technology in settings of highly experienced clinic.
Regarding the selection criteria of candidates for SAP therapy, poor glycemic control was the main indication for switching the treatment regimen from MDI to CSII, as we have previously reported.7,8 This finding is consistent with data that shown that problems with glycemic control are the main reasons for switching the treatment regimen from MDI to CSII, among these problems are not meeting the individualized HbA1c goal, large glucose excursions, frequent hypoglycemic events or dawn phenomenon.1,5,9–15 The lack of world-wide standardization in these criteria contributes to RCTs do not consistently use uniform criteria for the selection of ideal candidates to diabetes care technologies. Current indications for CSII derived from few studies that have specifically determined which factors successfully predict CSII use; main factors to consider are baseline A1c, adherence to medical treatment, and mental illness that is likely to impact adherence.1,12,16 Of them, adherence has important implications, because nonadherence to medical treatment is a significant predictor of all-cause mortality and hospital admission among patients with diabetes.17 Rodrigues and colleagues have shown that CSII can be an effective and safe therapy in some patients with classic contraindications in the setting of a specialist multidisciplinary service;18 however, treating non-adherent patients is challenging worldwide. Data from 16,061 participants in the T1D Exchange clinic registry showed that insulin pump was being used by 60% of participants, but only 30% of adults aged >30 years had achieved target HbA1c levels.19 As a strategy for improving metabolic control and long-term clinical outcomes we used the logic model for CDP based on disease management, particularly the mental-health and coaching components which encourage the patient to overcome psychological or social barriers that impede autonomy or improvement in medication compliance.
Furthermore, our findings confirm the moderate but significant impact of disease management programs on glycemic control, mean HbA1c decreased 0.56% by the end of 6-month CDP (p-value=0.004; 95% CI: 0.14–0.98). In three meta-analyses, disease management was associated with an improvement in glycemic control, as assessed by a mean reduction in HbA1c concentration of 0.51%, 0.52% and 0.81%.20–22 Disease management seems to be more effective than single strategies;21 however, short-duration intensive structured education courses such as DAFNE or BERTIE have reported relatively consistent evidence that appropriate education and support is likely to improve glucose control in motivated patients with inadequate glucose control. These education courses have reported HbA1c reductions between 0.2 and 0.7%, with a mean difference of 0.3% and 0.46% for BERTIE and DAFNE pooled data, respectively.23–30
The strengths of the present study are the effectiveness under real-world conditions in population of a developing country as Colombia and the scope beyond the structured education to a more comprehensive diabetes management program based on disease management. Among limitations are the relatively small population and retrospective nature with no control group available for comparison, the referral bias of patients with uncontrolled diabetes, and the lack of specific and standardized indicators to estimate the individual impact of each component.
In conclusion, intensive and multidisciplinary program based on disease management optimized the suitability of ideal candidates for SAP therapy by improving glycemic control and identifying adherence issues. This study provides real-world evidence of carefully applied protocols of patient selection and education in the setting of a highly experienced clinic. More evidence is needed regarding program evaluation, costs, and impact of each component.
Conflicts of interestAll authors declare no conflicts of interest.