To evaluate the effectiveness of nursing care against constipation and to identify, analyse and evaluate causes and consequences.
MethodologyObservational, descriptive and prospective study in polyvalent ICU tertiary hospital (2013–2015). Inclusion criteria: >18 years, stay >7 days, connected to respiratory support, with nasogastric tube and enteral or mixed nutrition. Patients with gastrointestinal pathology, encephalopathic and jejunostomy/ileostomy were excluded. The studied variables (age, sex, weight, height, pathology, medical treatment, nutrition and volume type, depositional characteristics, quantity and frequency, corrective measures and complications) were collected by ad hoc grill. It is authorised by the CEIC.
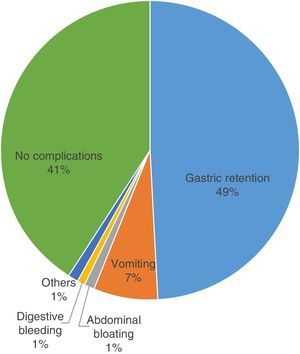
Results139 patients with a mean age of 62 years and average stay of 11 days were analysed; 63% suffered from constipation. Opiates and antacid were the drugs administered most frequently (99%), even though patients who took muscle relaxants, iron supplements and/or calcium and anti-hypertensive were the ones who suffered most from constipation (77%; 75%; 70%) The fibre free diet was the most widely used (60% constipated), followed by dietary fibre (51% constipated), and the combination of both (85% constipated). 56% used laxatives as a corrective measure, magnesium hydroxide being the most widely used; 54% began the first day. Gastric retention was the most relevant complication (49%).
ConclusionConstipation is a real multifactorial problem. We recommend:
- •
Intensified surveillance in patients with drugs that promote constipation.
- •
Use high-fibre diets from the outset.
- •
Apply laxatives and prokinetics early and in combination. We need to create a protocol for prophylaxis and management of constipation.
Valorar la eficacia de los cuidados enfermeros frente al estreñimiento e identificar, analizar y evaluar sus causas y consecuencias.
MetodologíaEstudio observacional, descriptivo y prospectivo, en UCI polivalentes de un hospital de tercer nivel (2013-2015). Criterios de inclusión: >18 años, estancia >7 días, con ventilación mecánica, portadores de sonda nasogástrica y nutrición enteral o mixta. Se excluyeron pacientes con enfermedad digestiva, encefalopáticos y con yeyunostomía/ileostomía. Las variables estudiadas (edad, sexo, peso, talla, enfermedad, tratamiento médico, tipo de nutrición y volumen, características deposicionales, cantidad y frecuencia, medidas correctoras y complicaciones) se recogieron mediante parrilla ad hoc. Dispone de autorización CEIC.
ResultadosSe analizaron 139 pacientes con edad media de 62 años y estancia media de 11 días; un 63% padecieron estreñimiento. Opiáceos y antiácidos fueron los fármacos más administrados (99%), aunque los relajantes musculares, suplementos de hierro y/o calcio y antihipertensivos fueron los que dieron más estreñimiento (77, 75 y 70%). La dieta sin fibra fue la más utilizada (60% estreñidos), seguida de dieta con fibra (51% estreñidos) y la combinación de ambas (85% estreñidos) Un 56% usó laxantes como medida correctora, siendo el hidróxido de magnesio el más utilizado; un 54% las iniciaron el primer día. La retención gástrica fue la complicación más relevante (49%).
ConclusiónEl estreñimiento es un problema real multifactorial. Recomendamos:
- •
Intensificar la vigilancia en pacientes con fármacos que favorecen el estreñimiento.
- •
Utilizar dietas con fibra desde el inicio.
- •
Aplicar de forma precoz y combinada procinéticos y laxantes. Creemos necesario crear un protocolo para la profilaxis y manejo del estreñimiento.
During their stay in the ICU critically ill patients suffer major physiological changes due to their pathological process. Although constipation is a common complication, less attention has been paid to it than others and few studies treat it as a specific problem. There is no agreed definition of constipation in critically ill patients, so that its incidence varies widely between studies, from 5% to 83%. Several studies show that constipation may be associated with a poor prognosis. This is because it has negative effects on the colon mucosa and tolerance of an enteral diet, and it may be connected with weaning failure or prolongation of the stay in the ICU, among many other gastrointestinal complications.
From a nursing point of view complications are detected every day which derive from or are connected with the pathologies of critically ill patients. These caring staff are therefore the first to detect these and raise the alarm if a complication is found to be present. Knowing the causes and the best corrective measure to take in case of constipation is vitally important for the good management of bowel movements.
Implications of the studyThis study contributes to raising awareness about the main causes of constipation in critically ill patients, as well as analysing which corrective measures should be implemented to prevent and manage the condition. It evaluates the latter and offers justified and common results-based measures to be agreed for implementation. A change in the current therapeutic management of constipation may be of key importance to reduce its incidence and therefore the complications arising because of it over the short to long terms.
Nursing staff play an important role in monitoring and checking bowel movements which, although it is not a priority in initial care, has to be taken into account to prevent the development and appearance of complications other than the initial reason for admittance.1,2
The problem we found in undertaking this study lies in the lack of agreement among experts in defining constipation.3 After analysing different definitions we decided that constipation may be defined as delayed and infrequent bowel movements (less than 3 times per week), with excessively dry stools or the feeling that the movement was incomplete.4
From our viewpoint as professionals in the field of critically ill patient care, it must be taken into account that the above definition of constipation cannot be extrapolated into the context of an intensive care unit (ICU), so that following a review of the bibliography, we define constipation as the absence of bowel movements 3 days after commencing enteral nutrition (EN).5,6
Although constipation is a problem that is rarely treated, it is a common problem in critically ill patients.7 According to several studies the prevalence of constipation in critically ill patients varies from 5% to 83%.8,9 This disparity between data is the result not only of the lack of an agreed definition, but also the lack of a protocol to prevent and treat it.2 Its causes have not been elucidated by controlled studies, and it may be associated with factors such as: alterations in intestinal mobility secondary to the pathological process, changes induced by different widely used drugs, and insufficient dietary fibre in comparison with the content of a normal diet.2,5,8,10 Due to the pathological process we are unable to act on some causes, including patient immobility or restricted physical activity. Nevertheless, other causes such as diet or the medication administered, may be revised or changed to prevent constipation.3,5
Several studies state that drugs such as the morphine-based ones, benzodiazepines and myorelaxants, among others, reduce intestinal mobility, increasing the need to administer laxatives.11 This is why authors such as Masri et al.9 state that laxative prophylaxis can be used safely and effectively to stimulate intestinal movement in critically ill patients. In their publication Rodriguez Fuentes et al.3 raise the problem that artificial emptying of the intestine may itself cause a new episode of constipation.
On the other hand it is beneficial to commence EN early in critically ill patients, as several studies point out that this is associated with reductions in days of admission, mechanical ventilation (MV), infections and even mortality,5,7,9,11,12 as well as preventing malnutrition secondary to hospital admission.13
Montejo et al.5 and Montejo González and Estébanez Montiel11 state that constipation is the second most common complication in EN, together with increase in gastric residue, diarrhoea, vomiting, regurgitation of the diet and abdominal bloating.2,5,7 These gastrointestinal complications may be the reason why in many cases the diet supplies insufficient nutrition for patient requirements.5,6,8 This is also affirmed by Serón Arbeloa et al. in their study,12 as they state that the actual calorie intake in critically ill patients is far lower than what is desirable, recommended or measured. They also support parenteral nutrition as a supplementary option to EN, to achieve optimum nutritional requirements.
After consulting several studies we reached the conclusion that there is no single diet which could be considered “ideal” for critically ill patients, but rather that the different situations patients may pass through mean that it is necessary to select the best diet at each time.6
In several studies, Montejo et al.,5 Montejo González and Estébanez Montiel,11 together with García de Lorenzo y Mateos and Montejo González6 state that dietary fibre plays an important role in preventing constipation in patients receiving prolonged EN. “If there is no contraindication, the choice of a diet containing fibre would be ideal. In constipated patients insoluble dietary fibre […] improves intestinal transit and increases the size of the faecal bolus while reducing the need for laxatives”.5 To prevent constipation, García de Lorenzo y Mateos and Montejo González6 propose an enteral diet that contains a mix of soluble and insoluble fibre, supplying 20–30g/day of total fibre, or 10–13g/1000kcal.
Studies published in the last decade7 have shown that constipation may be associated with a poor prognosis. Due to this the majority of authors2,7 mention the importance of creating a universal protocol for the identification, prevention and treatment of constipation.
In 1997 Lewis and Heaton14 suggested a scale for the visual evaluation of faeces in terms of their consistency and shape. This is known as the Bristol scale, and it classified faeces into 7 types in which the first and second are associated with constipation, while the sixth and seventh are associated with diarrhoea. This scale was revised by Mínguez Pérez and Benages Martínez15 in 2009, and they also evaluated its efficacy; although the results were positive, there is a logistical difficulty in using this tool in our everyday work as it is subjective, and different workers evaluate and care for these critically ill patients.
Evaluation and care in cases of constipation are mainly performed by nurses, as they spend the most time with patients. No studies show that expert nurses detect this problem and act on it sooner than relatively inexperienced staff.3
In a study undertaken in the Intensive Care Unit of San Jorge Hospital (Huesca), Serón Arbeloa et al.12 found that in a one-year period 93.5% of the patients who received EN or mixed feeding had gastrointestinal complications, and of these, 82% had constipation. Montejo González and Estébanez Montiel,11 in a study performed in 37 ICU with a sample of 400 patients over a 30 day period found that 56.25% of them had gastrointestinal complications and that of these, 15.7% had constipation as a complication. Additionally, Martínez et al.1 in a study undertaken in a cardiac surgery unit, found that applying an intestinal standard protocol reduced the incidence of constipation in this type of patients by 60%, while also minimising the use of invasive techniques to re-establish the standard.
Various studies undertaken in intensive care units confirm that constipation is a real complication in critically ill patients and that the use of an agreed protocol minimises its incidence.1,3,16 In the Hospital Universitari, Bellvitge (HUB) there is currently no protocol for action in case of constipation. As nurses we detect this problem every day, and we believe that to prevent it, it is first necessary to study its incidence, possible causes and the actions taken. This will make it possible to correct it and ensure better care of our patients.
The objective of this study was therefore to evaluate the efficacy of nursing care in cases of constipation and to identify, analyse and evaluate its causes and consequences in the patients admitted to the intensive care medicine department of the HUB.
Material and methodThe studyThis study was quantitative, observational, descriptive and prospective. It was undertaken during the years 2013–2015 in 2 multipurpose ICU; the Intensive care medicine Department of the HUB has 59 beds in a total of 6 units, of which 24 beds (2 units) are for acute critically ill patients of all types.
Inclusion criteriaPatients over the age of 18 years old were included, who stayed in the unit longer than 7 days, connected to MV and fed using an enteral or mixed (enteral and parenteral) diet. Following a review of the bibliography, the research team agreed that 7 days in the ICU were required to evaluate intestinal behaviour, given that in acute critically ill patients EN does not commence immediately after admission. Patients with spontaneous breathing are able express the need for a bowel movement themselves; this is why it was decided to restrict our study to patients with MV, as almost all of them are unable to express themselves.
Exclusion criteriaAll of the patients admitted due to a digestive disease were excluded from this study, including all types of surgery and complications that arose in this area (unrelated to EN and/or constipation), as well as patients with encephalopathy treated with lactulose. Those fitted with a narrow calibre polyurethane nasogastric catheter, nasojejunal catheter, percutaneous endoscopic gastrostomy, jejunostomy, ileostomy or colostomy were also excluded, due to the difficulty of evaluating their gastric residue. Patients fitted with a rectal catheter were not considered to fulfil an exclusion criterion.
The sampleThe population studied were all of the patients admitted to the Intensive care medicine Department of the HUB from November 2013 to November 2014; 140 patients fulfilled the inclusion criteria, and formed the sample studied. Subjects were selected by non-probabilistic random sampling.
VariablesThe following variables were included:
- •
Universal variables: age, sex, weight, height and medical speciality.
- •
Exposure variables: medical treatment, the type and volume of fibre contained in the EN.
- •
Bowel movement variables: faeces characteristics, amount and frequency of bowel movements.
- •
Efficacy of nursing care variables: corrective measures taken against constipation, tolerance of diet and/or complications.
Data were recorded using an ad hoc grid; they were extracted by means of daily consultation of nursing chart, medical treatments and patient histories. The SAP ASISTENCIAL® computer program was used to track daily admissions in the intensive care medicine department. Data gathering commenced after the start of EN (so that the diet started on day 1) and it ended in the case of non-compliance with the inclusion criteria or in the case of change of unit, exitus, disconnection of MV during a period of time longer than 48h, withdrawal of the EN during more than 48h or extubation.
Statistical analysisData analysis was descriptive: qualitative variables were expressed as frequencies and percentages, while quantitative variables were expressed as averages±standard deviation.
The following tools were used to analyse the relationships between the variables: the chi-squared test (if there was any relationship between the application or not of corrective measures and the appearance of complications), Anova (if there was any relationship between the type of drug administered and constipation, or whether there was a relationship between corrective measures and the existence or not of constipation), the Student t-test of independent groups (if there was a relationship between the type of medical disease and constipation) and the Student t-test of repetitive measurements (if the administration of laxatives was effective in preventing constipation). The statistical program used was Microsoft Office Excel.
Before starting the study permits were requested from the Hospital Management and the Clinical Research Ethics Committee was asked for approval. The study commenced once it had been approved. The treatment, communication and transfer of the personal data of all the subjects taking part followed the stipulations of Organic Law 15/1999, of 13 December on personal data protection.
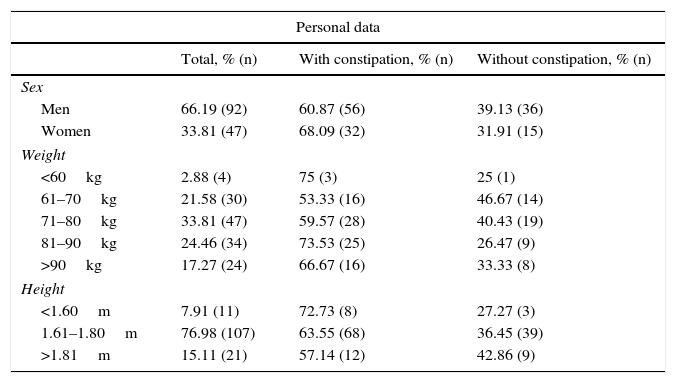
ResultsDuring the duration of the study 140 patients were initially included, although one was finally ruled out due to faults in data recording. Of the total, 92 were men (66.19%) and 47 were women (33.81%). The average age was 62.69 years old, with a standard deviation of ±13.05. Table 1 shows the anthropometric values of the subjects studied. The average duration of data gathering was 11.24±6.32days.
Anthropometric values.
| Personal data | |||
|---|---|---|---|
| Total, % (n) | With constipation, % (n) | Without constipation, % (n) | |
| Sex | |||
| Men | 66.19 (92) | 60.87 (56) | 39.13 (36) |
| Women | 33.81 (47) | 68.09 (32) | 31.91 (15) |
| Weight | |||
| <60kg | 2.88 (4) | 75 (3) | 25 (1) |
| 61–70kg | 21.58 (30) | 53.33 (16) | 46.67 (14) |
| 71–80kg | 33.81 (47) | 59.57 (28) | 40.43 (19) |
| 81–90kg | 24.46 (34) | 73.53 (25) | 26.47 (9) |
| >90kg | 17.27 (24) | 66.67 (16) | 33.33 (8) |
| Height | |||
| <1.60m | 7.91 (11) | 72.73 (8) | 27.27 (3) |
| 1.61–1.80m | 76.98 (107) | 63.55 (68) | 36.45 (39) |
| >1.81m | 15.11 (21) | 57.14 (12) | 42.86 (9) |
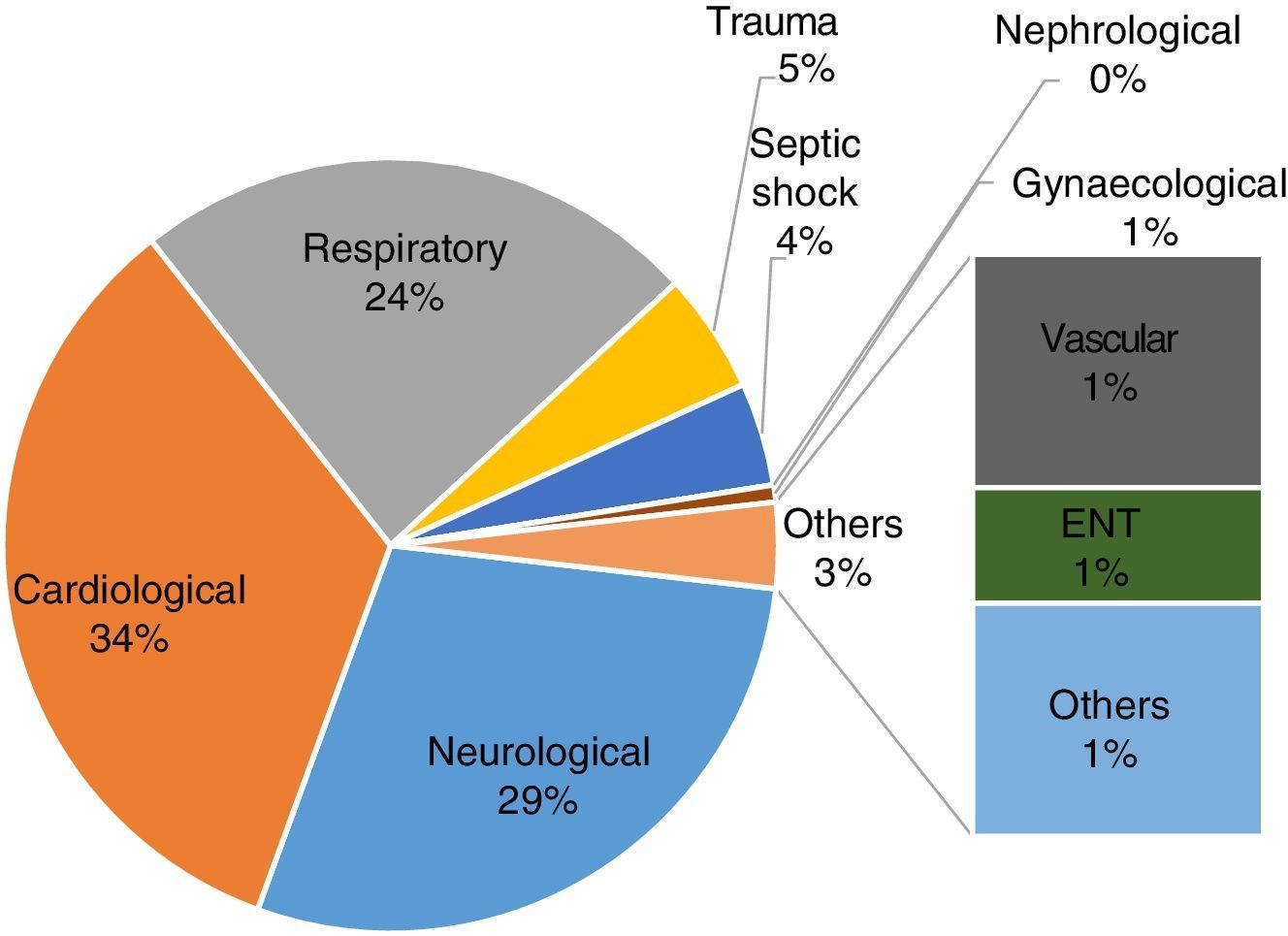
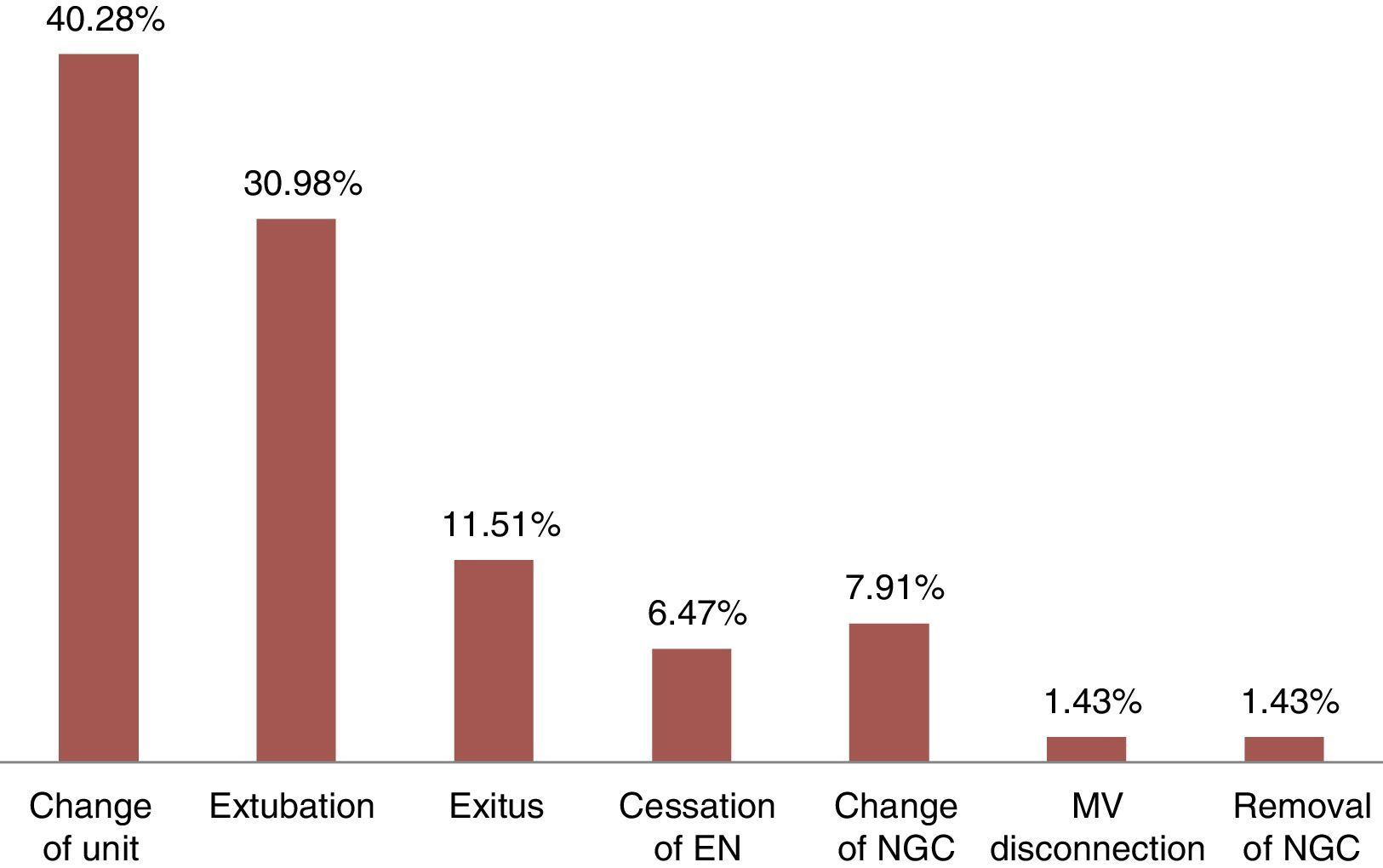
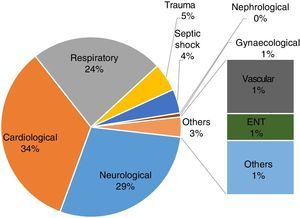
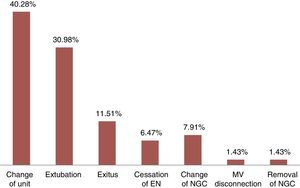
The most common diseases (Fig. 1) were cardiological, at 33.81% (47 patients), neurological, at 28.77% (40 cases) and respiratory, at 23.74% (33). The most frequent diagnoses were aortic prosthesis, subarachnoid haemorrhage and pulmonary failure, respectively. The main reasons for ending the study, as shown in Fig. 2, were change of unit (40.28%; 56 patients) and extubation (30.93%; 43 cases).
63.31% (88 patients) suffered constipation at some time during the time they were included in our study. It should be pointed out that constipated patients had longer times of admission than non-constipated ones (13.33±6.41 days; 8.11±4.31 days, respectively).
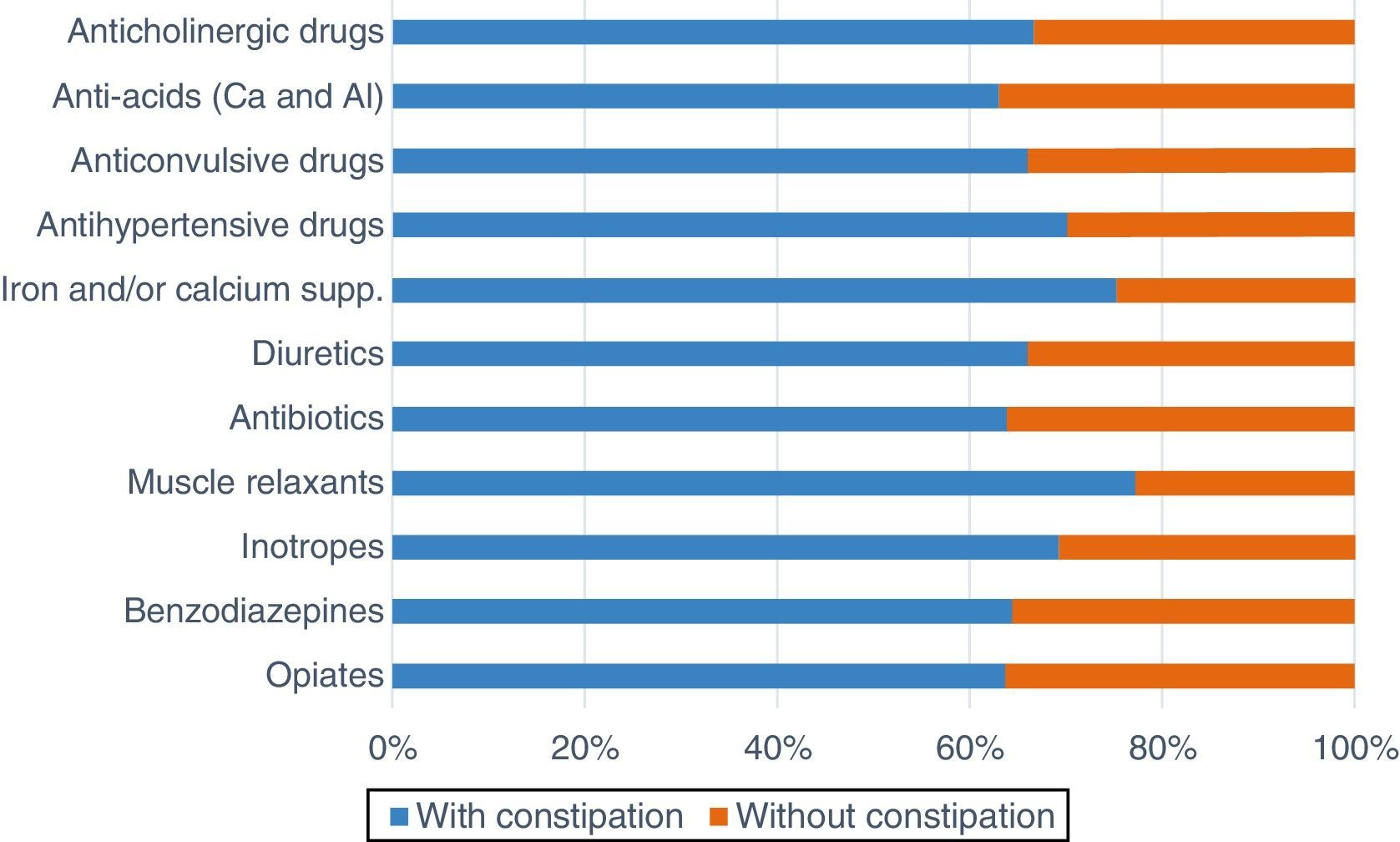
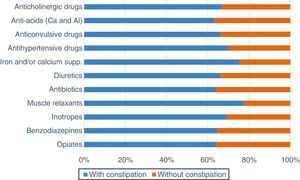
Regarding pharmacological treatment (Fig. 3) the ones administered the most widely were opiates and anti-acids (99.28%; 138 patients for each group); 88 and 87 patients (63.76%; 63.04%) respectively, suffered constipation. The highest rate of constipation was in the patients taking muscle relaxants (77.19%; 44 patients), iron supplements and/or calcium (75.34%; 55) and/or antihypertensive drugs (70.21%; 33).
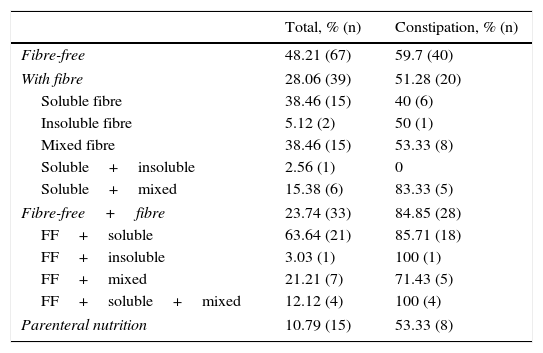
The most widely used type of diet was fibre-free, in 48.2% (67 patients); 59.7% of these patients (40 cases) suffered constipation. Only 29.05% (39 patients) received a diet containing fibre, with a 51.28% incidence of constipation (20 cases). 23.74% (33 patients) were switched from fibre-free EN to one containing fibre; 84.84% (28 patients) were constipated (Table 2).
Types of enteral nutrition given and in association with constipation.
| Total, % (n) | Constipation, % (n) | |
|---|---|---|
| Fibre-free | 48.21 (67) | 59.7 (40) |
| With fibre | 28.06 (39) | 51.28 (20) |
| Soluble fibre | 38.46 (15) | 40 (6) |
| Insoluble fibre | 5.12 (2) | 50 (1) |
| Mixed fibre | 38.46 (15) | 53.33 (8) |
| Soluble+insoluble | 2.56 (1) | 0 |
| Soluble+mixed | 15.38 (6) | 83.33 (5) |
| Fibre-free+fibre | 23.74 (33) | 84.85 (28) |
| FF+soluble | 63.64 (21) | 85.71 (18) |
| FF+insoluble | 3.03 (1) | 100 (1) |
| FF+mixed | 21.21 (7) | 71.43 (5) |
| FF+soluble+mixed | 12.12 (4) | 100 (4) |
| Parenteral nutrition | 10.79 (15) | 53.33 (8) |
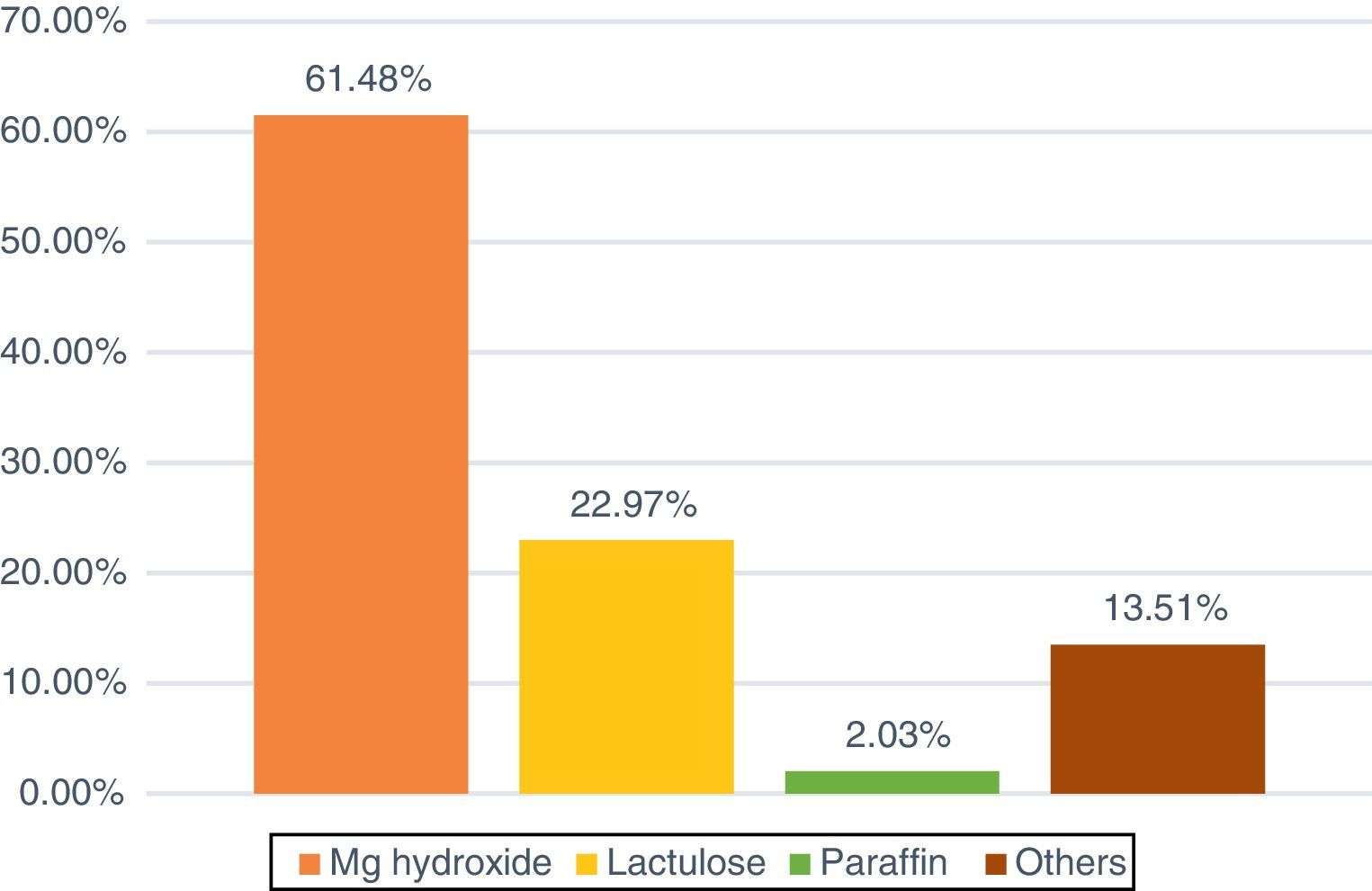
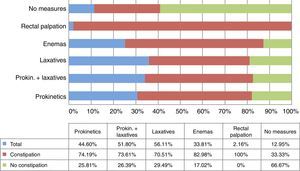
Respecting corrective measures (Fig. 4), laxatives (56.11%; 78 patients), following by laxatives combined with prokinetics (51.79%) were the most widely used. There was a high level of constipation in both groups (70.51; 73.61%). Only 33.81% (47 patients) were given enemas (82.97% of those with constipation) while 12.94% (18 patients) received no treatment (33.33% of those with constipation).
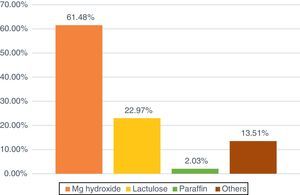
The laxative that was used the most (Fig. 5) was magnesium hydroxide, in 61.48% of patients, followed by lactulose, at 22.97% (34 patients). In the case of the enemas, one for washing was used (1–1.5L warm water with a soap solution, or 2–3 trisodium citrate/lauryl sulfoacetate micro-enemas) were used the most (51.66%; 31) followed by the one by Casen® (31.66%; 19).
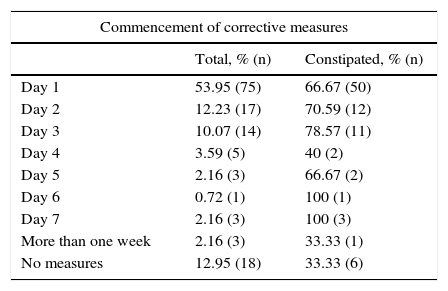
Of the 139 participants in the study, 75 of them (53.95%) started the first day of EN with a corrective measure; 66.67% (50 patients) were constipated (Table 3). Of the 75 who commenced taking some sort of corrective measure, 55 (39.56%) took prokinetics and 40 took laxatives (28.77%).
The association of constipation with the day corrective measures commenced.
| Commencement of corrective measures | ||
|---|---|---|
| Total, % (n) | Constipated, % (n) | |
| Day 1 | 53.95 (75) | 66.67 (50) |
| Day 2 | 12.23 (17) | 70.59 (12) |
| Day 3 | 10.07 (14) | 78.57 (11) |
| Day 4 | 3.59 (5) | 40 (2) |
| Day 5 | 2.16 (3) | 66.67 (2) |
| Day 6 | 0.72 (1) | 100 (1) |
| Day 7 | 2.16 (3) | 100 (3) |
| More than one week | 2.16 (3) | 33.33 (1) |
| No measures | 12.95 (18) | 33.33 (6) |
Fig. 6 shows the complications that arose. 58.76% of the total sample had some type of complication, the most important of which was gastric retention, at 49.32% (69.86% had constipation). On the other hand, 41.21% had no complication (55.7% with constipation).
DiscussionAnalysis of the results of this study shows that there is a significant incidence of constipation. Taking our classification of constipation into account as the lack of a bowel movement 3 days after the commencement of EN,5,6 63% of the sample fulfilled this. Under similar conditions Martínez et al.1 show an incidence of 73.9%, Mostafa et al.2 mention 83% and Martín Orejana et al.18 cite 84.06%.
After recording and analysing data on the frequency, amount and characteristics of stools, we were unable to find a common intestinal pattern of behaviour for the same due to the disparity of the results obtained. It should be pointed out that the amount and characteristics of stools are subjective data recorded by nurses, and that on several occasions these data are not shown.
Pharmacological treatmentAccording to the study by Lerga et al.,16 “Evaluation of the intestinal pattern in ICU patients using nursing records” it was found that patients who received opiates, benzodiazepines and myorelaxants showed a greater alteration in their intestinal rhythm and stool characteristics. Our study, which analyses a broader range of medications, found that opiates, anti-acids, benzodiazepines and antibiotics are the most widely used, while the highest rate of constipation occurred in the patients receiving myorelaxants (77%), iron and/or calcium supplements (75%) or antihypertensive drugs (70%). It has to be said that many of the medications used in critically ill patients may alter gastric emptying and slow intestinal transit by reducing peristaltic action. Due to this we are unable to conclude that a single drug is the cause of constipation, but rather that this may be due to a combination of several drugs. Due to the complexity of these patients, the drugs they are given are vital and indispensable for their recovery.
NutritionThe study results show the range of diets given to patients, and in some cases different diets were administered to a single subject.
As Montejo González and Estébanez Montiel11 among other authors underline, the use of diets containing fibre improves intestinal transit by increasing the size of the faecal bolus and reducing the need for laxatives. Only 28% of our patients received a diet containing fibre, and of these the lowest rate of constipation was in those patients taking soluble fibre. On the other hand, 48% of the sample received a fibre-free diet, and of these 60% suffered constipation. During admission 23% of the subjects received a fibre-free diet that was subsequently changed to one containing fibre. It should be pointed out that this group suffered the highest rate of constipation (85%), so that this fact was probably due to the presence of constipation before the change to a diet with fibre.
Taking the relatively small size of the sample into account, we agree with several studies6 that there is no single ideal diet, but rather that patient context and their evolution will determine which diet is the most suitable at any time. In our units we have specific diets for specific diseases, although many of them do not contain the necessary amount of fibre, so that a large number of patients are given fibre-free diets.
Corrective measuresA range of pharmacological and non-pharmacological methods are used in ICUs to prevent or resolve constipation. The main methods used are prokinetics, laxatives and enemas.3,9–11,17
Prokinetics favour EN tolerability by increasing intestinal mobility and thereby minimising gastrointestinal slowing, which is one of the side effects of many of the drugs used in critically ill patients.11 According to the results of our study, only 40% of the patients received prokinetics from the first day of EN.
Lubricant-type laxatives (liquid paraffin) are the most widely used in our ICUs, together with osmotic ones (magnesium hydroxide and lactulose), of which magnesium hydroxide is the most used. 54% of the total sample received laxatives in the first 72h following the start of EN, while 22% did so subsequently. We believe that administering laxatives in the first 72h may be a preventative measure against constipation, while after this period it would be used to resolve an existing problem.
Although a significant number of patients started to receive a corrective measure in the first days following the start of EN, the rate of constipation was very high (73% prokinetics; 68% laxatives). In a similar study, in which laxatives were given late and prokinetics were given according to a unit protocol, the incidence of constipation was higher (84.06%).18 We therefore believe that the early administration of prokinetics and laxatives may be the best way of preventing constipation in critically ill patients.
On the other hand, enemas are usually given as a means of resolving constipation.1,3,6,10,18 34% of our sample received them, and the enema wash was the type most widely used. An enema is normally used once laxatives have proven to be ineffective; it has to be said that this method is not infallible, as due to the fact that it is used at a late stage, several enemas are usually required to resolve the problem.18
ComplicationsThe data show that the main gastrointestinal problems arise in association with EN. Gastric retention, at 49%, is the most common among our patients, and in some cases it caused the suspension of the diet. Mentucci8 mentions 63% of complications in his study, of which an increase in gastric residue was the most frequent (42.1% of cases).
70% of these patients suffered constipation, and this may be due to alteration of gastrointestinal behaviour, with a reduced rate of gastric emptying as well as a fall in intestinal mobility. 41% of the total presented no associated complication.
LimitationsOne of the limitations of this study was that the results cannot be extrapolated to all of the patients who are admitted to the HUB.
Few studies of this subject have been carried out, so that searching the bibliography was an additional difficulty. Nevertheless, this was worthwhile, given that the results may be of scientific interest.
Another difficulty was the number of cases which were lost during the research (patients who were discharged before the seventh day, or ones who died), given that this reduces the number of subjects included in the study.
Another limitation was lack of knowledge about the intestinal behaviour of patients prior to admission.
Lastly, the difficulty in obtaining data should be mentioned. This was due to incomplete recording by the nursing team regarding stools (appearance and amount) as well as the types of enema given.
ConclusionsWe conclude that constipation is a real problem in patients admitted to the HUB ICUs, with an incidence of 63%. There is no single cause for this, but rather a series of factors influence it: alterations in intestinal mobility secondary to pathological processes, an insufficient supply of fibre and changes induced by several drugs used in critically ill patients (sedatives and relaxants, etc.), so that we make the following recommendations:
- •
Intensify monitoring to detect constipation in patients treated with drugs such as muscle relaxants, iron and/or calcium supplements and antihypertensive drugs.
- •
Use diets containing fibre from the first, given that fibre aids the normalisation and frequency of bowel movements.
- •
Use prokinetics and laxatives in combination and at an early stage, given that they improve gastrointestinal mobility and prevent constipation.
Lastly, we believe it is necessary to create a nursing protocol for the prophylaxis and management of constipation. This would help to prevent it in many cases, and it would also raise the awareness of the nursing team to improve this area of care.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank the Continuous Training Unit of the HUB for its trust and support. We would also like to thank our families for their patience throughout this project. Lastly, we would like to thank Víctor López Balcells and Jaume Tejero Ambrosio for their help in statistics and translation.
Please cite this article as: Pérez-Sánchez J, Fernández-Boronat J, Martínez-Méndez E, Marín-Cagigas ML, Mota-Puerto D, Pérez-Román MC, et al. Evaluación y abordaje del estreñimiento en el paciente crítico. Enferm Intensiva. 2017;28:160–168.