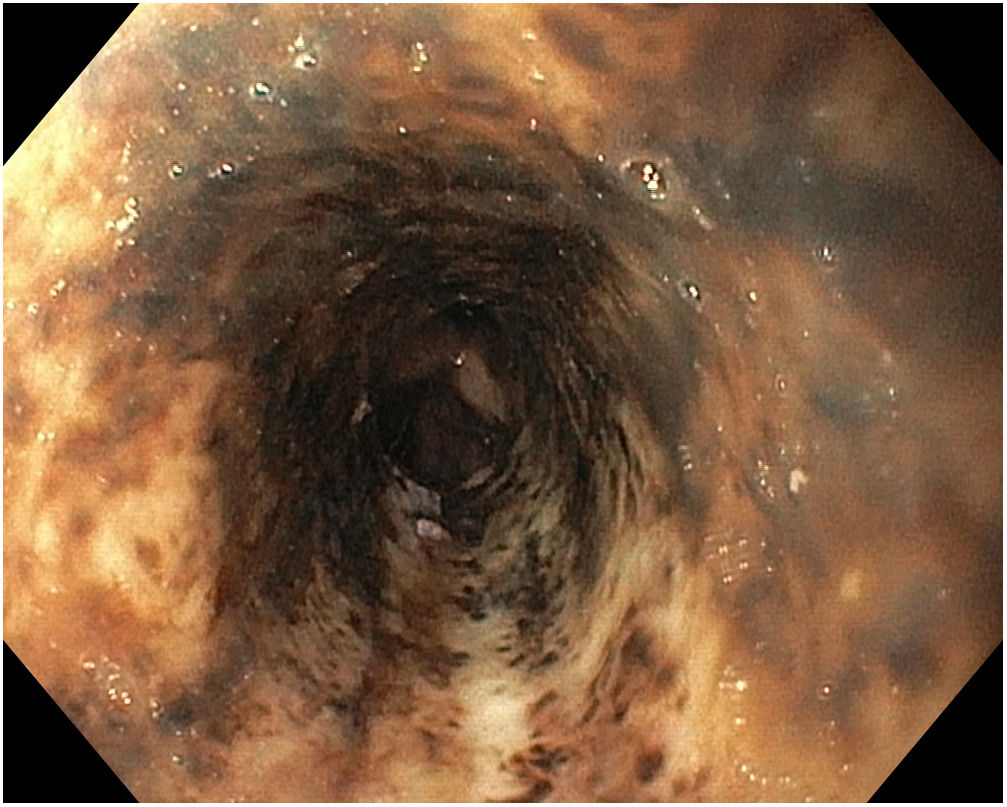
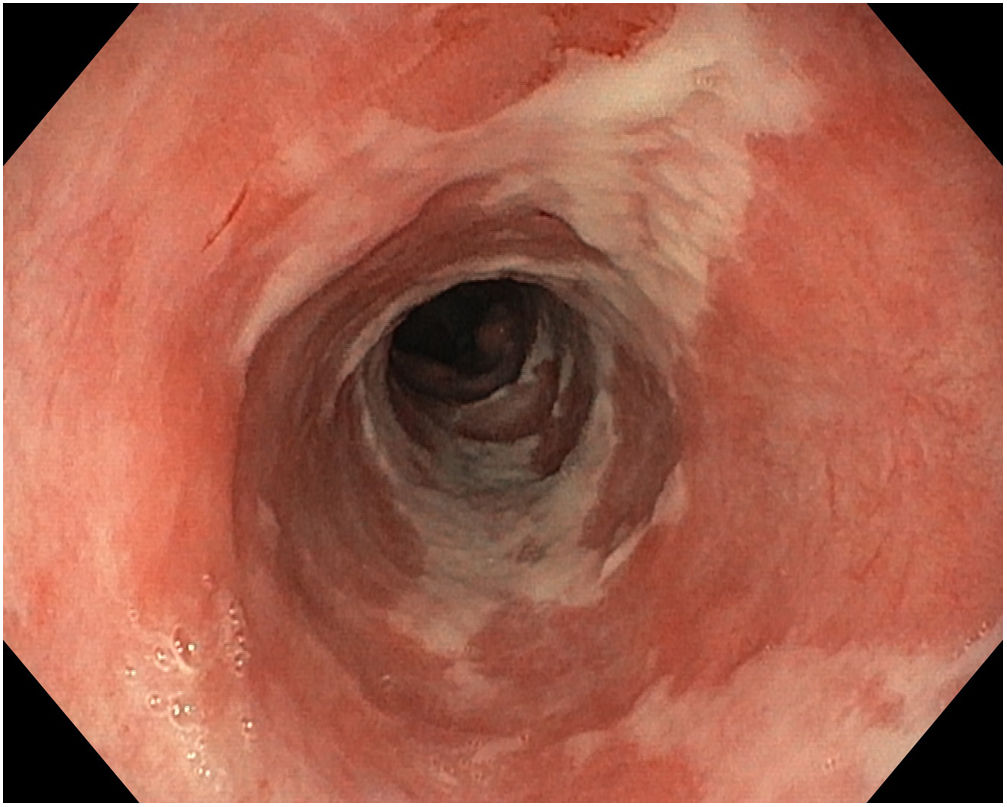
A 60-year-old man, an active smoker and drinker with multiple diseases, was admitted for Wernicke–Korsakoff syndrome, severe hypocalcaemia and hypomagnesaemia, urinary sepsis, respiratory infection, and Ogilvie syndrome. After presenting haematemesis, he underwent an emergency gastroscopy which visualised from 23 cm to oesophagogastric transition, oesophagus with continuous blackish mucosa found to be highly friable with the passage of the endoscope and possessed a necrotic appearance (Fig. 1). The proximal oesophagus was left intact. Following 10 days of NPO, parenteral nutrition and omeprazole infusion, the patient’s oesophageal mucosa was re-evaluated and found to show improvement and re-epithelialisation (Fig. 2). His diet was gradually reintroduced, and his condition followed a suitable clinical course.
Acute necrotising oesophagitis or black oesophagus is rare, is of unknown aetiology and has a multifactorial pathophysiological mechanism.
It usually manifests in the form of upper gastrointestinal bleeding in patients with multiple diseases, malnourished patients and patients with ischaemic and infectious conditions. It is diagnosed when a black, friable and haemorrhagic oesophageal mucosa located in the distal third of the oesophagus with proximal spread is visualised on endoscopy.1
Treatment is based on bowel rest, suitable hydration and nutrition, and proton-pump inhibitors at high doses, associated with specific management of adjacent diseases.2 A mortality rate of up to 32 % has been reported3, although it is also linked to the patient’s underlying disease.
Please cite this article as: Roa Colomo A, García Robles A, Ruiz Escolano E. Esófago negro ¿es tan malo como parece? Gastroenterol Hepatol. 2019;42:632–633.