Peripheral primitive neuroectodermal tumour (PNET) is a malignant mesenchymal tumour. Although PNETs can occur in numerous solid organs, it is an extremely rare tumour entity, specially involving the liver.
We report a 19-year-old boy with Hepatitis B Virus (HBV) infection who was diagnosed with a primary PNET of the liver.
Los tumores neuroectodérmicos primitivos periféricos (TNPP) son un tipo de tumor mesenquimal maligno. A pesar de que pueden aparecer en numerosos órganos sólidos, es una entidad tumoral muy poco frecuente, sobre en el hígado.
Se presenta un joven de 19 años de edad con hepatitis B (VHB) que fue diagnosticado con un TNPP primario en el hígado.
Peripheral primitive neuroectodermal tumour (PNET) is a malignant mesenchymal tumour belonging to the family of “small round-cell tumours”. The majority of patients are younger than 30 years of age. Although PNETs can occur in numerous solid organs, they are extremely rare,1 specially involving the liver.
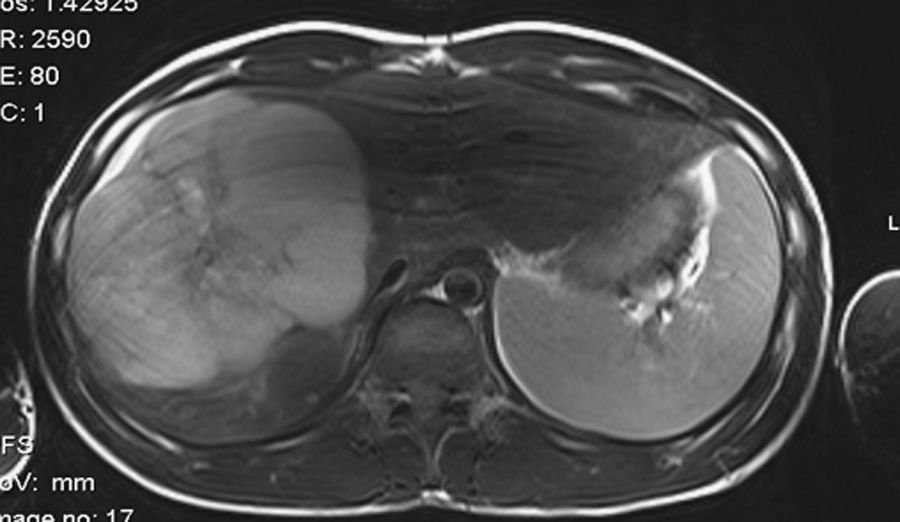
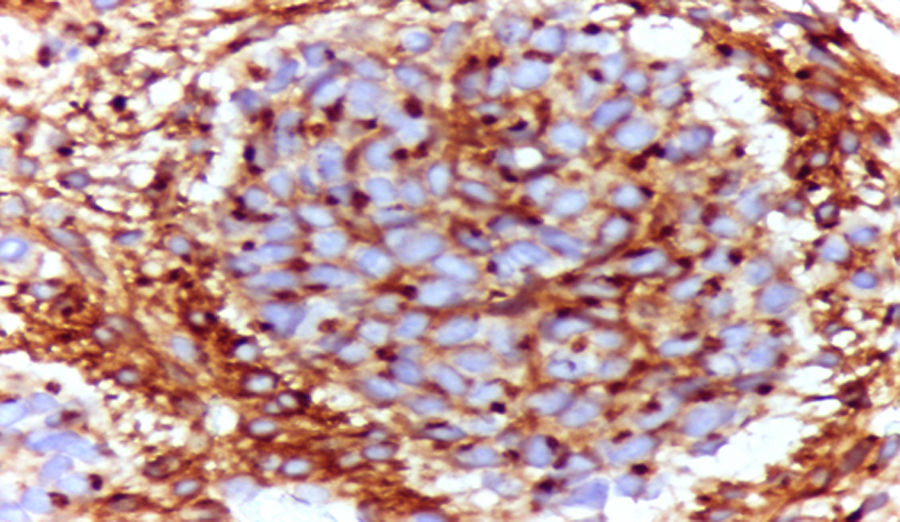
Case reportHerein we report a case of a 19-year-old male, referred to our Hepatology Department, after detecting Hepatitis B Virus (HBV) DNA by polymerase chain reaction (PCR) amplification following an attempted blood donation. He was otherwise healthy, asymptomatic, and neither he nor his family had risk factors for HBV infection. We confirmed the diagnosis of chronic hepatitis B: HBsAg positive, HBeAg positive, with a HBV DNA PCR>8.04log10, with genotype D. The only abnormal laboratory results were elevated ALT=125U/L and total bilirubin=15mg/dL. Hepatitis C virus infection, as well as other liver diseases were excluded, and entecavir (0.5mg/day) was started. An abdominal ultrasound revealed a hypoechoic tumour with a hyperechoic central area, with 10cm, and MRI showed a hepatic mass with 15cm (Fig. 1), well defined, heterogeneous, with a necrotic central area, with atypical behaviour to the contrast, with mild enhancement in the arterial phase and becoming isodense in the portal and delayed phases, suggesting a hepatic neoplasm. The patient was submitted to an ultrasound-guided biopsy of the liver mass, and the histological exam identified a primitive neuroectodermic tumour (PNET): on microscopic examination a small round blue cell malignant tumour was described (Fig. 2); immunohistochemical staining was CD99 positive. Exams were performed in order to detect other sites of involvement by the tumour including CT-scan of the head and full body bone scan that were negative, and computed tomography (CT)-scan of the chest, abdominal cavity, and pelvis that revealed 4 pulmonary lesions, with less than 1cm each. The cell blood count was normal. The patient was referred to an Oncology Department, specialized in sarcomas, with the diagnosis of a peripheral PNET of the liver, with pulmonary metastases, and started on systemic chemotherapy having completed 5 cycles. Further ahead, a PET-scan showed an 8cm hepatic mass, with significant reduction of viable cells. The patient was then proposed for tumour resection, after chemoembolization, but unfortunately, there was a sudden and rapid progression of the disease. He became jaundiced, and therapeutic ERCP was performed to place some drainage stents. He also became quite painful, so he started palliation with analgesic drugs and none other treatment was tried because patient was in a poor condition. He died 4 months later.
DiscussionThe Ewing Family of Tumours (EFT) includes Ewing Sarcoma (ES) and peripheral PNET.2 PNET is a rare neural crest tumour classified on the basis of the site of origin into central nervous system (CNS) PNET and peripheral PNET. There is considerable overlapping between PNET and ES, sharing a common and unique translocation t (11; 22) (q24; q12). PNET constitutes less than 1% of all sarcomas.3
PNET is a member of the family of “small round cell tumours”. Although PNET can occur in numerous solid organs such as kidney, ovary, vagina, testis, uterus, cervix uteri, urinary bladder, parotid gland, heart, lung, rectum, pancreas and gall bladder, it is an exceptionally rare tumour entity. Liver involvement is highly uncommon and is usually in the form of metastases from other primary cancers.3
PNET tumours affect primarily white and Hispanic individuals and are extremely rare in those of African or Asian origin. The majority of patients with PNET are younger than 30 years of age, with a peak incidence at the age of 15 years.4
Although most sarcomas arise spontaneously, some risk factors have been identified. Exposure to ionizing radiation increases the incidence of sarcomas, typically more than 7–10 years after exposure, most commonly in patients treated with radiation therapy for breast and cervical cancer as well as lymphoma. Other risk factors include chronic lymphedema and exposure to some chemicals. The only virus known to play a role in the development of sarcoma in humans is the human herpes virus 8.2 It is known that hepatitis B virus DNA is capable of integrating into the host genome. Recently, it has been assumed that HBV affects many human cell types in addition to hepatocytes. Among children with lymphoid and solid tumours the HBV markers are much more frequent than in control groups.5 Naumova and Kisselev have described a considerable prevalence of HBV markers in children with embryonic tumours and in their parents.6 The mutagenic/oncogenic effect of HBV DNA integration should be considered in a wider context than previously thought.5 HBV insertion into cellular genes is frequent (around 70%) and integration can occur in genes encoding proteins that are important in the control of cell signalling, proliferation, and viability.7 Although all of these facts hold true for sarcomas, little is known about PNET.
Typical histological features include sheets of monomorphic round cells with small hyperchromatic nuclei, inconspicuous nuclei, and scant cytoplasm. There is usually extensive necrosis with peritheliomatous preservation of viable tumour and a lack of intracellular material. The histogenesis of ES and PNET is unknown; however a neuroectodermal origin has been proposed based on variable expression of neuronal immunohistochemical markers, ultrastructural features, and the ability of ES/PNET cell lines to differentiate along a neural pathway in vitro. In the vast majority of cases, PNET have been shown to express extremely high levels of an antigen determined by the MIC 2 gene; the product of this gene is a glycoprotein, designated CD99.4
In ES and PNET, several factors have been considered to be of prognostic importance: stage, primary tumour site, size, age, and response to therapy. Staging is based on physical examination, CT or MRI scan of the primary tumour, and chest and bone scan. In addition, a bone marrow aspiration should be done.
Poor prognostic factors in adult patients are large tumours (>5cm), primary tumour of the pelvis, metastases at presentation, and advanced age. Advanced age as a poor prognostic factor may either be related to biological aspects of a more aggressive disease or a lower dose intensity of chemotherapy to be delivered. Metastases at presentation are correlated with a poor prognosis. The location of metastases is of importance. A long term disease free survival was observed in five out of six patients with lung metastases. In contrast, patients with bone metastases have a more progressive disease.8 Approximately 25% of patients have detectable metastatic disease to the lung, bone, and bone marrow at diagnosis, but nearly all patients have micrometastates, as evidenced by a 10% cure rate with local therapy alone. The most important negative prognostic factor is tumour dissemination at the time of diagnosis.4
Despite improvement in the treatment outcome of ES and PNET during past decades, almost half of all patients ultimately die of this disease. The five-year overall survival, in adult patients with non metastatic disease, ranges from 35 to 60%. Large series report an overall survival of 20–30% for patients with metastatic disease.8
Due to the low incidence of this tumour, it is strongly advocated that these patients be referred to specialised oncology centres with participation in international trials.
PNET outside the CNS are mostly found within the deep soft tissue of the extremities and the paravertebral areas. The kidney is the most common visceral organ involved by PNET. Involvement of the liver has been reported in the form of metastases from other primary sources presenting as liver abcess.3 Nevertheless, primary visceral PNET are exceedingly rare. Two cases of small intestine and hepatic duct involvement, respectively, have been reported in children.3 To the best of our knowledge, this is the second case to be reported of PNET primarily involving the liver: the other case published in the literature was of a 20-year-old woman presenting with massive hepatomegaly, in which the liver biopsy revealed a PNET in the form of diffuse infiltration.
Once PNET is diagnosed, the standard treatment is systemic multi-agent chemotherapy combined with surgery and/or radiotherapy.3 There is no proven regimen of chemotherapy. This patient has made a regimen based on doxorrubicin, with dacarbazin.
In conclusion, PNET of the liver is an extremely rare tumour as this is the second case to be reported. Although uncommon, PNET has to be considered in the differential diagnosis of atypical hepatic tumours in young patients. Combined modality therapy with a curative intention and a multidisciplinary approach by experienced medical oncologists, surgeons, gastroenterologists, and radiotherapists are crucial in order to achieve optimal efficacy.