We present the case of a 62-year-old patient, with no relevant medical history, who came to the emergency department with right upper quadrant pain and low-grade fever lasting 72h. There were no other symptoms and he reported no previous similar episodes.
Laboratory tests showed discrete leukocytosis with neutrophilia and normal bilirubin. Abdominal ultrasound found acute cholecystitis, although it was impossible to rule out associated liver abscess. The magnetic resonance study (Fig. 1) showed an image suggestive of gallbladder cancer with significant inflammation of adjacent liver tissue. A magnetic resonance cholangiopancreatography was requested, which showed general thickening of the gallbladder wall with homogeneous enhancement and signs of adjacent hepatic tissue involvement, suggestive of primary infiltration of the gall bladder.
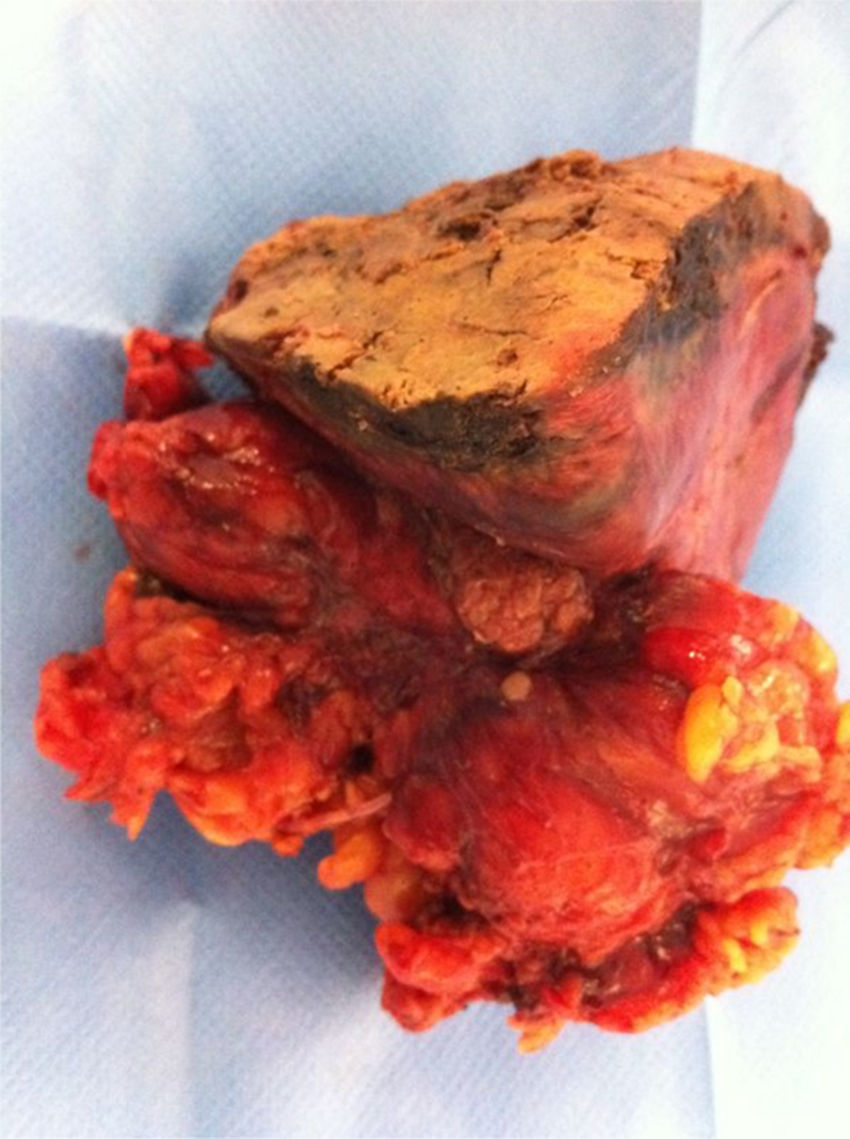
Scheduled surgery was indicated, during which a large hardened tumour-like area of liver tissue was observed. Cholecystectomy and hepatic bisegmentectomy (IV and V) were performed (Fig. 2). No pathological adenopathies were observed. There were no postoperative complications.
Pathological anatomy confirmed a diagnosis of pseudotumoural xanthogranulomatous cholecystitis (XGC) with extensive liver bed involvement.
XGC is a rare variant of chronic cholecystitis that was first described in 1970.1 It represents 0.7% of all cholecystectomy specimens, although it can reach up to 13.2% in oriental series. It is more frequent in men aged from 44 to 63 years.2
Histologically, it is characterised by proliferative fibrosis secondary to chronic inflammation, which causes thickening of the gall bladder wall that extends to adjacent structures, with mottled, dense local adhesions that usually affect the liver bed, duodenum, transverse colon, omentum and even the head of the pancreas. It can be considered a premalignant condition.
The pathogenesis is unknown, but most researchers suggest that extravasation of bile into the gall bladder wall could be an important factor.3 The leakage of bile, caused by both rupture of the Rokitansky–Aschoff sinuses and ulceration of the mucosa, induces severe inflammation of interstitial tissue that leads to the release of destructive enzymes into the gall bladder wall and surrounding area. Obstruction and chronic infection caused by the presence of stones have been implicated as a contributory factor.
The clinical signs, physical examination and laboratory results cannot differentiate this disease from other gall bladder or bile duct diseases, since the clinical presentation can vary greatly.4 Manifestations include acute, chronic cholecystitis (with or without pancreatitis), since cholelithiasis occurs in all patients, as was the case in our patient, episodes of cholangitis with mild jaundice (up to 50% of cases), and complicated forms with fistulous tracts, perivesicular or hepatic abscesses, perforation of the gall bladder, or even cholecystoenteric fistulas, occurring in 23–32% of cases.
Acute symptoms of biliary colic tend to be more present in cases of XGC, while early-stage gallbladder cancer (GBC) is cured in a non-specific way.5 Testing for serum CA 19-9 does not aid diagnosis.
When biliary disease is suspected, the test of choice is abdominal ultrasound, which reveals the presence of lithiasis and wall thickening. The presence of hypoechoic bands in the vesicular wall has been described as highly suggestive of XGC.
Computed tomography (CT) may be of more help in showing hypodense bands in the vesicular wall with enhancement, thickening and intramural nodules. An 18F-fluorodeoxyglucose positron emission tomography scan may be useful for differential diagnosis with malignancy.6 Magnetic resonance cholangiography will not differentiate XGC from gallbladder cancer.
When in doubt, ultrasound- or CT-guided cytological puncture may be indicated, as suggested by Das et al.7 (sensitivity 90.6% and specificity 94.7%) or echo-endoscopy-guided puncture, as well as ERCP in cases of jaundice or cholangitis.
One of the most important aspects of the study of this entity is differential diagnosis,8 since preoperative differentiation between XGC and GBC is of vital importance in selecting the correct surgical strategy. However, it can sometimes be extremely difficult to correctly collate imaging, ultrasound and CT scans.
The definitive treatment of this disease is surgery. During the procedure, the XGC can mimic the appearance of vesicular cancer due to gall bladder wall thickening and local destruction associated with intense adhesions. For this reason, intraoperative frozen section biopsy is advised.9 However, Houston et al.10 reported a 10% incidence of GBC in patients with XGC, leading them to recommend resecting all adjacent affected tissues, at least in cases with extensive involvement, including associated fistulas.
Open cholecystectomy is the technique of choice due to intense fibrosis of Calot's triangle, extensive focal inflammation, and the possible coexistence of cancer due to the high rate of malignant transformation (about 80%, depending on the series).11 There is no firm evidence that all affected tissue needs to be resected.
Please cite this article as: Gómez Cabeza de Vaca V, Alba Mesa F, Piñero González L, Komorowski AL. ¿Colecistitis aguda, crónica o cáncer de vesícula biliar? Gastroenterol Hepatol. 2017;40:671–673.