Over the last decade, a growing number of acute hepatitis C (AHC) virus cases have been reported in men who have unprotected sex with men (MSM) and who also often have human immunodeficiency virus (HIV).1
Up until just two years ago, AHC treatment was based on the prolonged administration of pegylated interferon plus ribavirin (P/R), which boasted limited efficacy and serious adverse effects. The standardisation of regimens with direct-acting antivirals (DAA) has revolutionised the way in which this infection is treated, with cure rates in excess of 95%.2 Because a cured HCV infection does not result in immunity, patients who continue to engage in high-risk sexual behaviour or substance abuse are at high risk of reinfection.
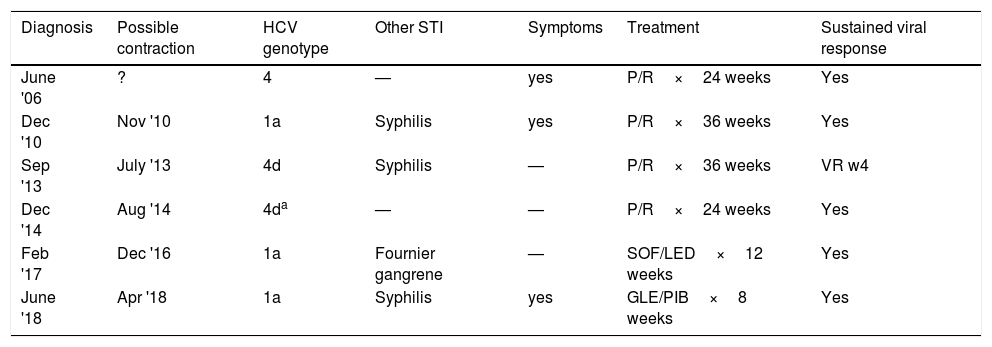
We present the case of a 57-year-old MSM patient with chronic HIV infection and good viral and immune control on antiretroviral therapy who experienced six episodes of AHC (Table 1).
Characteristics of acute hepatitis C episodes.
| Diagnosis | Possible contraction | HCV genotype | Other STI | Symptoms | Treatment | Sustained viral response |
|---|---|---|---|---|---|---|
| June '06 | ? | 4 | — | yes | P/R×24 weeks | Yes |
| Dec '10 | Nov '10 | 1a | Syphilis | yes | P/R×36 weeks | Yes |
| Sep '13 | July '13 | 4d | Syphilis | — | P/R×36 weeks | VR w4 |
| Dec '14 | Aug '14 | 4da | — | — | P/R×24 weeks | Yes |
| Feb '17 | Dec '16 | 1a | Fournier gangrene | — | SOF/LED×12 weeks | Yes |
| June '18 | Apr '18 | 1a | Syphilis | yes | GLE/PIB×8 weeks | Yes |
GLE/PIB: glecaprevir/pibrentasvir; HCV: hepatitis C virus; P/R: pegylated interferon+ribavirin; SOF/LED: sofosbuvir/ledipasvir; STI: sexually transmitted infection; VR: viral response.
The patient exhibited symptoms consistent with acute hepatitis in three of the episodes. In the other cases, the same diagnosis was suspected despite the fact that he did not exhibit suggestive symptoms due to finding high transaminase levels in the patient's six-monthly HIV blood test.
When asked directly, the patient denies parenteral drug use or high-risk behaviour, apart from occasional unprotected anal sex with different sexual partners, although never in a group. He admits to using inhaled vasodilators and, occasionally, oral stimulants. The patient had multiple sexually transmitted infections (STIs) during follow-up, and AHC was concomitantly diagnosed on four occasions. The first four episodes were treated with P/R over 24 weeks, extended to 36 weeks for two episodes in which treatment began more than six months after exposure. A sustained viral response (SVR) was achieved in all cases except one, where reinfection occurred within three months of treatment. On this occasion and at the request of the patient after a high-risk contact, an HCV-RNA test was performed six weeks after treatment, which was positive. Because the viral genotype was 4d, the same as the one treated previously, a phylogenetic study was performed, which confirmed it was a reinfection as the HCV strain was different to the previous one.
A recently-published meta-analysis collected reinfection information from the literature and found that MSM/HIV+patients are the group most susceptible to reinfection.3 This is supported by a broad collaborative European study of 606 AHC cases in MSM/HIV+patients, which found a mean reinfection rate of 7.3 cases per 100 patient years (p/y).4
The increased incidence of sexually-transmitted AHC in MSM/HIV+patients has been attributed to several factors: a higher HCV viral load in the blood and semen of HIV+patients, certain sexual practices that involve a higher risk of mucosal damage, the presence of other ulcerative STIs (found in four of our patient's six episodes), a higher number of sexual partners and the use of recreational drugs or their intentional consumption to enhance and prolong sexual relations.
In 2012, the Hospital Clínic de Barcelona published the first epidemic outbreak of AHC in MSM/HIV+patients in Spain.5 Up to December 2017, 35 episodes of reinfection out of 265 cases of AHC in MSM/HIV+patents had been diagnosed (unpublished data). In light of these findings, the reinfection rate in Spain increases to 22 cases per 100 patient years, which is significantly above the European average. This revelation underlines the need to implement health promotion campaigns, assess screening strategies in this high-risk population, start treatment early and offer damage limitation programmes to prevent new outbreaks. These measures may help us to meet the World Health Organization (WHO) target of reducing the incidence of viral hepatitis by 90% by 2030.
Please cite this article as: Laguno M, Martínez-Rebollar M, de la Mora L, Pérez-del-Pulgar S, Mallolas J. Barreras para la eliminación del virus de la hepatitis C en el colectivo de hombres que tienen relaciones sexuales con hombres infectados por el virus de la inmunodeficiencia humana: el elevado riesgo de reinfección. A propósito de un paciente con 6 episodios.. Gastroenterol Hepatol. 2019;42:555–556.