Disseminated peritoneal leiomyomatosis is a benign and rare condition, with some 150 cases reported in the literature.1 It is characterised by multiple smooth muscle cell-containing nodules in the abdominopelvic cavity. It tends to affect premenopausal women,2,3 while an association with hormonal hyperactivity caused by oral contraceptives and ovarian neoplasia, etc., has also been reported in select cases.1,4,5 Most cases are asymptomatic, although clinical manifestations will depend on the number and size of the lesions, as well as their rapid growth. It is usually diagnosed by chance in a radiological study or during surgery.1,5 The biggest challenge is establishing a differential diagnosis with peritoneal carcinomatosis,3,5 with a histological diagnosis required for confirmation.2
Treatment should be personalised according to the characteristics and symptoms of each individual patient.
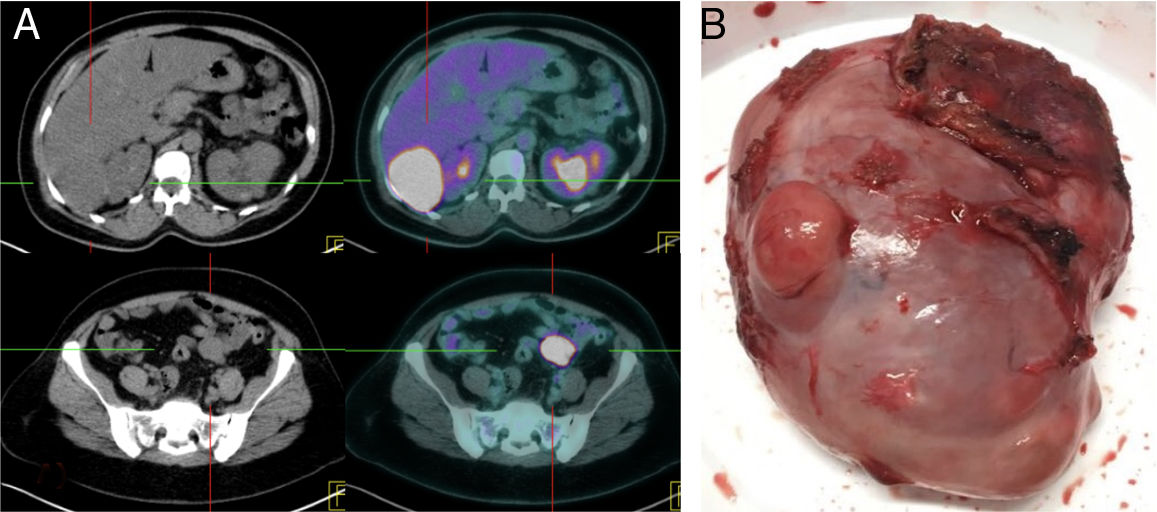
We present the case of a 42-year-old female patient with a history of hypertension and polycystic kidney disease under follow-up with Nephrology, and taking combined oral contraceptives (COCs) for the last two years. She underwent laparoscopic surgery in 2013 due to a uterine fibroid with a pathological diagnosis of leiomyoma. She was referred to the clinic following the chance finding of two masses measuring 6.3 and 3.1cm on the control CT scan for her polycystic kidney disease, located in Morison's pouch and in the mesosigmoid. It was not possible to rule out peritoneal implants. The patient was asymptomatic and her abdominal examination was normal. Fine-needle aspiration biopsy (FNAB) was performed on both lesions, revealing mesenchymal neoplasia with a low proliferation rate. The lesions expressed oestrogen receptors, Bcl-2 and vimentin, consistent with leiomyoma as well as other diagnoses, so their excision was required for correct identification. The study was completed with a PET/CT scan (Fig. 1A), which showed intense uptake of both lesions, with peak standardised uptake values (SUVs) of 26.4 and 24.8, respectively, as well as an enlarged uterus of myomatous appearance.
The patient underwent a midline laparotomy to identify and perform complete resection of both lesions (Fig. 1B). Pathology revealed mesenchymal neoplasia of low malignant potential (Ki-67=2%, <1mitosis/10 HPF) with smooth muscle cell phenotype and positive oestrogen receptors, consistent with leiomyoma. Both the haematoxylin and eosin and immunohistochemistry results were compared with the myomectomy performed in 2013. Both sets of lesions were found to be very similar, with the primary difference being that the current lesions were more vascularised and had lower positivity for desmin. In light of these findings, the discrepancy between the high SUV values found in the PET/CT scan and the apparent low histological grade (minimal mitosis and lack of signs of malignancy such as pleomorphism and necrosis) were striking. The patient was therefore referred to Gynaecology for a hysterectomy and bilateral adnexectomy assessment.
After three months, the patient underwent an abdominal hysterectomy with bilateral adnexectomy and a new 1-cm lesion adhered to the wall of the peritoneum was discovered during the procedure. The pathology findings for this lesion were the same as for the previously resected lesions, although with a Ki-67 of 35%, without identifying any pathological findings in the specimen from the hysterectomy and bilateral adnexectomy. She was referred to Oncology, where adjuvant hormone therapy with tamoxifen was started, with no signs of relapse in the six-month follow-up CT scan.
Although it is normally a benign condition, progression to malignancy has been reported in 3–5% of cases.3 The differential diagnosis is primarily established with leiomyosarcomas, peritoneal carcinomatosis and lymphomas.
Microscopically, mesenchymal neoplasia are made up of smooth muscle fibres with oestrogen and progesterone hormone receptors,1,2 although patients’ hormone levels are normal in the majority of cases. In light of the foregoing, an individual's predisposition is believed to be a very important factor in the development of the disease.3
Because of the limited number of cases reported, the treatments reviewed in the literature vary based on the characteristics of each patient,1,3 ranging from a conservative approach with clinical-radiological follow-up to radical surgery (hysterectomy with bilateral adnexectomy and excision of all lesions), in an attempt to reduce the hormonal impact and thereby prevent malignant degeneration. For residual tumours, adjuvant hormone therapy may be useful. Chemotherapy is reserved for cases that exhibit malignant degeneration.
Please cite this article as: Rodríguez García P, Castañer Ramón-Llín J, Romera Barba E, Sánchez Pérez A, Vázquez Rojas JL. Leiomiomatosis peritoneal diseminada, un reto diagnóstico. Gastroenterol Hepatol. 2019;42:554–555.