The histological diagnosis of intrathoracic and lung cancers is a diagnostic challenge for which there are several techniques available. Transoesophageal endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) biopsy of mediastinal lymphadenopathy has been associated with infectious complications, such as mediastinitis and mediastinal or thoracic abscesses.1 The most common bacteria to cause such complications are Enterococcus faecium and Streptococcus viridans.2Streptococcus anginosus belongs to the group of viridans streptococci which mainly inhabit the oropharynx and the gastrointestinal tract. Although infections with a tendency to abscess formation have been described in patients with dental problems and poor oral hygiene,3 the finding of this pathogen in an intrathoracic abscess is less common.
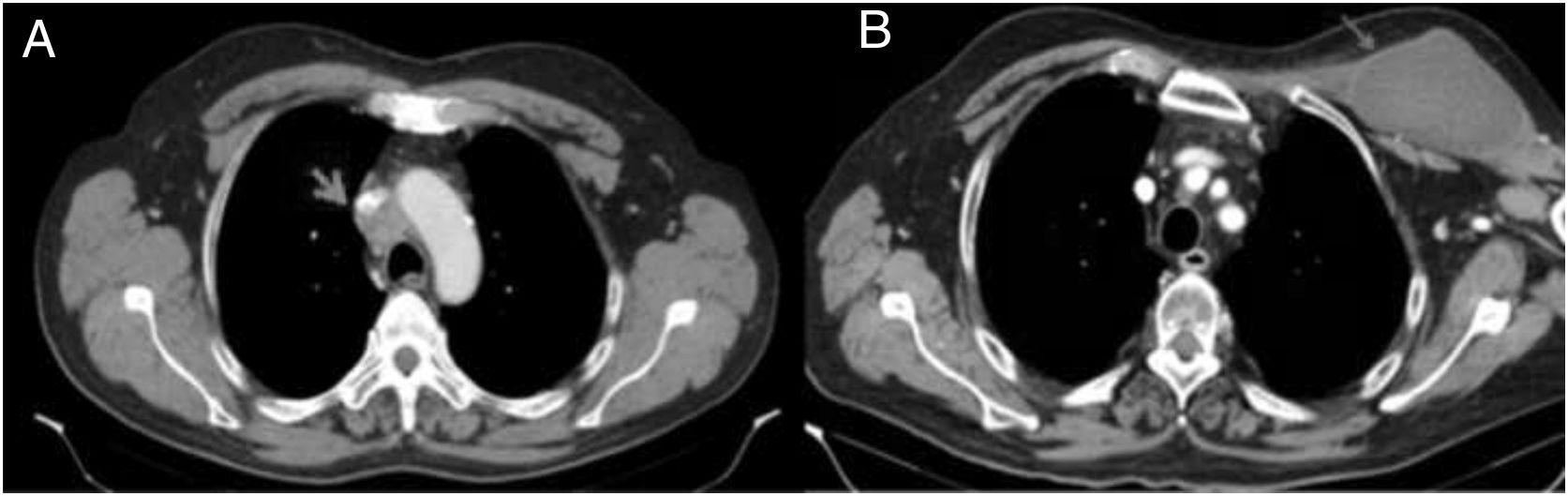
We present the case of a 61-year-old male smoker, with no other relevant medical history, who came to Accident and Emergency with a month-long history of facial oedema. On examination, upper extremity oedema was noted, with swollen neck and distension of both jugular veins. The blood test was normal. In view of these findings, the patient was admitted for investigation, beginning with a chest X-ray in which mediastinal widening was identified. Cervical/thoracic computerised tomography scan showed a spiculated nodule in the right upper lobe, in addition to a mediastinal mass measuring 3×4cm which was invading and obstructing the superior vena cava (Fig. 1A). With the diagnosis of superior vena cava syndrome, intravenous methylprednisolone was administered and a stent was inserted in the vein. A week later, in order to clarify the aetiology, an EUS-FNA (22F) was performed, with three passages through the oesophagus, obtaining adipocytes, myocytes and oesophageal squamous epithelium, but without visualising any tumour cells. As malignancy was still strongly suspected, two weeks after admission a video-mediastinoscopy was performed in the operating theatre with suitable aseptic measures, under prophylaxis with amoxicillin-clavulanic acid, obtaining histological material compatible with poorly differentiated pulmonary adenocarcinoma. The day after the EUS-FNA the patient developed progressively worsening pain in his shoulder and left thoracic region. Once recovered, he started chemotherapy and radiotherapy. Three weeks later, he returned to Accident and Emergency for this same reason, this time associated with a palpable painless tumour in the left thoracic region and spontaneous purulent drainage from the mediastinoscopy incision, without any signs of wound infection. Computed tomography showed a cyst-like mass 12×6cm in size in the subcutaneous cellular tissue of the patient's left cervical/thoracic region (Fig. 1B). Treatment was started with intravenous meropenem and excision and drainage of the abscess was performed, evacuating abundant purulent contents, and drains were placed in the subcutaneous and left sub-pectoral cellular tissue. Bacteriology study of the exudate demonstrated the presence of S. anginosus. The patient was discharged after 20 days in hospital.
Infectious complications (such as mediastinitis and mediastinal or thoracic abscess) after EUS-FNA are very rare. In the review published by Von Bartheld et al.,1 mediastinitis and thoracic abscess formation occurred in 0.08% and 0.03% respectively. They also found that such complications were associated essentially with sarcoidosis and immunodepression, as in our patient, who started treatment with chemotherapy and radiotherapy. In another systematic review conducted by Wang et al.,4 the mediastinal infectious complication rate was 0.38%. Although our patient had undergone two invasive diagnostic tests while in hospital (EUS-FNA and video-mediastinoscopy), the route of entry was the EUS-FNA, as it was after that procedure that he developed symptoms. The FNA passed through the layers of the oesophagus, resulting in direct communication between the oesophagus and the mediastinum. Further support to the FNA as origin is the fact that the microbiology analysis demonstrated the presence of S. anginosus which, although it can be present in other locations, is a commensal bacterial flora of the oropharynx and the oesophagus. Our case was a rare complication caused by a pathogen with a special predisposition for forming abscesses. We did not give our patient antibiotic prophylaxis prior to the EUS-FNA; according to the European Society of Gastrointestinal Endoscopy guidelines, it is not recommended.5 Some authors suggest disinfection of the oral cavity as a means of reducing this complication.2 That has not been assessed in clinical trials, but there is experimental data in favour of such a measure.
Please cite this article as: Tejero-Pintor FJ, Blanco-Álvarez JI, Bailón-Cuadrado M, Rodríguez-López M. Absceso cervicotorácico secundario a punción con aguja fina guiada por ecografía endoscópica transesofágica. Gastroenterol Hepatol. 2019;42:35–36.