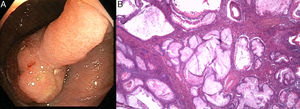
An inflammatory myoglandular polyp (IMGP) or Nakamura polyp is a rare, smooth-surfaced, non-cancerous polyp, reddish in colour, and most often found in the distal colon. It is characterised by typical histological findings which differentiate it from other non-cancerous polyps.1 From a pathology point of view, there are three typical characteristics: inflammatory tissue infiltrating the lamina propria; smooth muscle proliferation; and the presence of hyperplastic glands that can form cysts.2
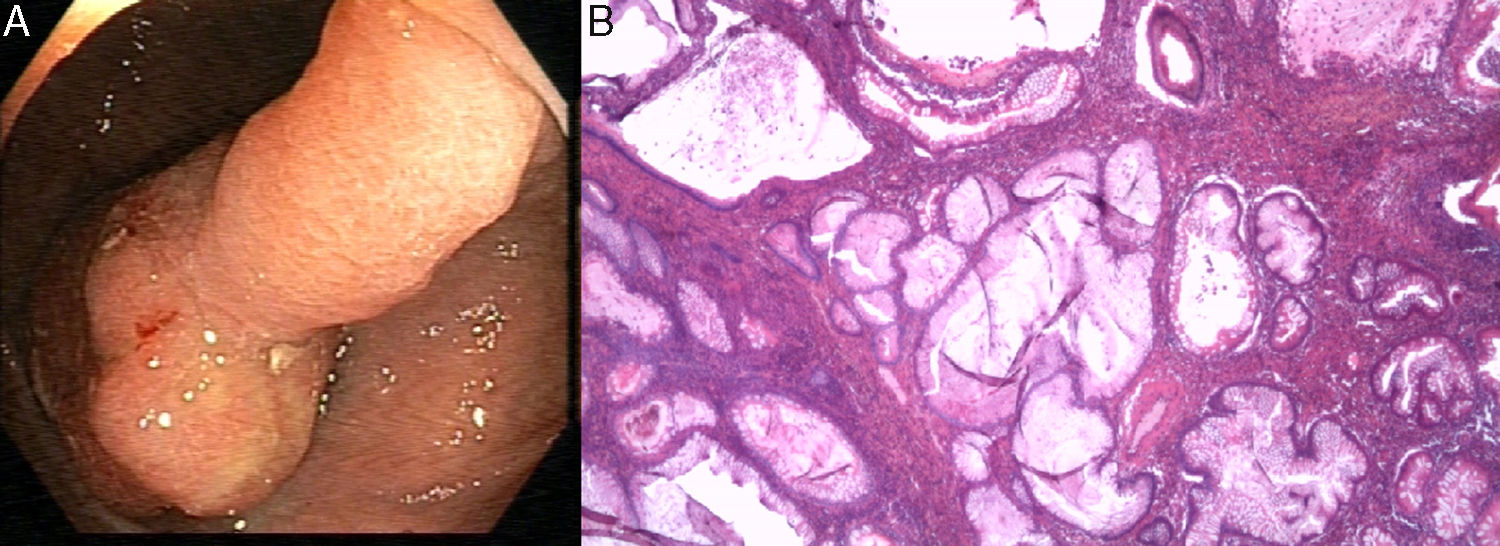
We present the case of a 69-year-old man referred to the endoscopy unit for colonoscopy following a positive faecal occult blood test. The patient denied having had any gastrointestinal symptoms and claimed his bowel habit was regular with no blood or mucus in his stools. On physical examination, his abdomen was non-tender on palpation, with no relevant findings. Blood tests showed a haemoglobin level of 12.9g/dl with no other results of note. The colonoscopy findings were as follows: in the ascending colon, 4cm from the ileocaecal valve, a pedunculated polyp (Paris classification 0-Ip) with a peduncle measuring 10mm and a head measuring 30mm with a lobulated appearance and eroded surface (Fig. 1A). Endoscopic polypectomy was performed with loop diathermy in the same procedure, after submucosal injection with diluted adrenaline solution, indigo carmine and hydroxyethyl starch, subsequently placing a haemostatic clip in the wound. The polyp was retrieved with a Roth net and histological study revealed a tissue formed by glandular proliferations with cystic dilations separated by walls of smooth muscle fibres associated with granulation tissue (Fig. 1B).
The IMGP was initially described by Nakamura in 1992 in a series of 32 patients who had solitary non-cancerous colonic polyps, most of them pedunculated, with a smooth red surface, and predominantly distal to the splenic flexure.3 Since then, 76 cases of IMGP have been published with the following distribution: 40 (52.6%) in sigmoid colon; 14 (18.4%) in transverse colon; 11 (14.5%) in rectum; seven (9.2%) in descending colon; two (2.6%) in ascending colon; one (1.3%) in caecum; and one (1.3%) in terminal ileum. Out of the total, 84% were pedunculated and 16% sessile, generally with a smooth, reddish mucosa, although occasionally with a lobulated appearance.1,2,4,5 The pathophysiology of these lesions is still not fully understood. The cause was first thought to be trauma, with the initial events being damage and/or mucosal prolapse caused by transit through the bowel of formed stools and peristalsis, which are more marked in the distal colon. However, in the case reports published more recently, as in our patient, we see that these lesions can also occur in more proximal areas of the colon, and we therefore presume there must be other additional factors involved in their development.1 Although IMGP can be asymptomatic, low gastrointestinal bleeding is the most common symptom and may appear clinically in the form of haematochezia, faecal occult blood or chronic anaemia. In some patients with large polyps, gastrointestinal symptoms such as abdominal pain and constipation have been reported.2 Diagnosis is made from histological study of the polyp sample, usually obtained by endoscopic polypectomy, on identification of the typical pathology characteristics discussed above. The polyp biopsy study can sometimes be inconclusive if proliferation of smooth muscle cannot be identified or because the sample is too superficial, and this can lead to an incorrect diagnosis. In some cases reported in the literature, the resection was carried out surgically.1 It is important to make a differential diagnosis with other non-cancerous polyps, such as inflammatory polyps, inflammatory “cap” polyposis, polyps secondary to mucosal prolapse, fibroid inflammatory polyps, juvenile polyposis, or the polyps in Peutz-Jeghers syndrome. The distinction is essentially based on the clinical context of the patient and the histological findings.1 IMGP have a good prognosis, since they are both clinically and histologically benign, with no known malignant potential. Moreover, to date no cases of recurrence have been reported following endoscopic resection of this type of polyps.1,2
In conclusion, the inflammatory myoglandular polyp is a rare type of non-cancerous colorectal polyp with distinctive histological characteristics and it is unusual to find one in the ascending colon.
Please cite this article as: Sánchez-Aldehuelo R, Figueroa-Tubío A, García de la Filia I, González-Olivares C, García García de Paredes A, García-Cosío M, et al. Pólipo de Nakamura: un hallazgo endoscópico infrecuente. Gastroenterol Hepatol. 2019;42:34–35.