Immune thrombocytopenic purpura (ITP) is characterised by the production of autoantibodies against platelets, which are then destroyed by the mononuclear phagocyte system. In rare cases, ITP presents as an extraintestinal manifestation of inflammatory bowel disease (IBD), but few studies have explored its treatment in this context.1 We present the case of a patient with ITP secondary to Crohn's disease (CD) with complete response to treatment with anti-TNF.
This was a 55-year-old man with an unstudied history of diarrhoea with a frequency of 2–3 stools per day. In January 2016, during a routine company medical check-up, blood tests found a platelet count of 30,000/l with no bleeding diathesis and no other abnormalities. Suspecting ITP, the patient was started on corticosteroids (1.5mg/kg/day). The study was completed with viral serologies (HBV, HCV, HIV), H. pylori and autoimmunity, which were all negative. The patient's diarrhoea and thrombocytopenia improved, but reappeared after tapering the corticosteroids. A bone marrow study was performed, which showed normal cellularity, with an increase in the number of non-dysmorphic megakaryocytes. A CT of the chest and abdomen was performed which showed inflammation of the ileum. Colonoscopy confirmed multiple superficial ulcerations. Histology showed active chronic ileitis with no granulomas. The patient was diagnosed with non-fistulising ileal Crohn's disease with secondary ITP. In March 2016, azathioprine (AZA) was started, to which eltrombopag was added until control of IBD was achieved, postponing splenectomy. After two months, he presented with acute pancreatitis and AZA was discontinued. At follow-up, thrombocytopenia was poorly controlled (<30,000/l) and diarrhoea persisted. Accordingly, in July 2016, anti-TNF (infliximab 5mg/kg) was started. The patient's platelet count tripled after three weeks (from 21,000/l to 61,000/l), reaching 70,000/l at 12 weeks, which allowed corticosteroids to be withdrawn. By November 2016, the platelet count was over 100,000/l. We also observed improvement in CD, with resolution of diarrhoea (baseline Crohn's Disease Activity Index [CDAI] 251 and final CDAI 44) and evidence of mucosal healing in a colonoscopy performed in November 2016. Currently (January 2018) the patient is asymptomatic, with platelets >100,000/l and mucosal healing (18 months after starting infliximab).
IBD is chronic inflammation of the intestine caused by an immune system dysfunction with CD4 T cell-mediated Th1 immune response that stimulates production of INF-γ and TNF.2 In idiopathic ITP, a Th1 immune response with increased TNF also causes peripheral platelet destruction. Some authors have suggested that IBD may produce bacterial translocation, in which bacterial antigens pass into the bloodstream.3 This would trigger a Th1 immune response and synthesis of antibodies which, in rare cases, can cross-react against platelet antigens, giving rise to secondary ITP.4
Many different approaches to treating ITP secondary to IBD which are also useful in idiopathic ITP have been suggested1,3: steroids, gamma globulins, AZA, rituximab and splenectomy. Specifically, in non-responders, the use of anti-TNF for IBD and colectomy has been described in the case of ITP associated with ulcerative colitis.5 Another anti-TNF (etanercept) which is not effective in CD has been used successfully in refractory idiopathic ITP.6 Variations in the effectiveness of different anti-TNFs has been attributed to structural differences (for example, infliximab and adalimumab fix complement, but etanercept does not), which have a different modulatory effect on the immune response of Th1 cells.6,7
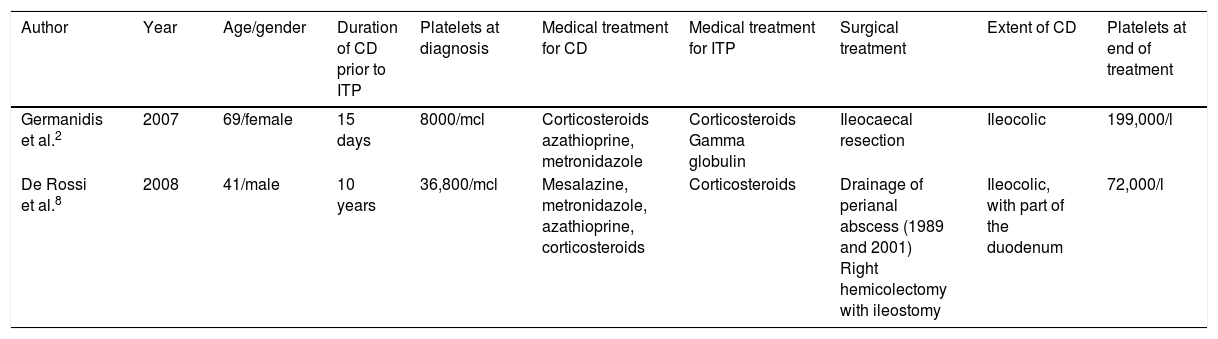
In order to verify the effect of anti-TNF in the treatment of ITP secondary to IBD, we conducted a systematic review of PubMed, Web of Science and SCOPUS databases for studies in adult populations published up to August 2017 in English and Spanish. The following MeSH terms were used: (“Crohn disease” OR “ulcerative colitis” OR “inflammatory bowel disease”) AND (“thrombocytopenic purpura” OR “thrombocytopenia”) AND (infliximab OR adalimumab OR anti-TNF). After screening for duplicates, 63 studies were identified. We chose seven articles; anti-TNF (infliximab) was used to treat CD and ITP in only two of these studies (Table 1).2,8 Response was positive in both cases.
Characteristics of case reports.
| Author | Year | Age/gender | Duration of CD prior to ITP | Platelets at diagnosis | Medical treatment for CD | Medical treatment for ITP | Surgical treatment | Extent of CD | Platelets at end of treatment |
|---|---|---|---|---|---|---|---|---|---|
| Germanidis et al.2 | 2007 | 69/female | 15 days | 8000/mcl | Corticosteroids azathioprine, metronidazole | Corticosteroids Gamma globulin | Ileocaecal resection | Ileocolic | 199,000/l |
| De Rossi et al.8 | 2008 | 41/male | 10 years | 36,800/mcl | Mesalazine, metronidazole, azathioprine, corticosteroids | Corticosteroids | Drainage of perianal abscess (1989 and 2001) Right hemicolectomy with ileostomy | Ileocolic, with part of the duodenum | 72,000/l |
In conclusion, ITP is a rare extraintestinal manifestation of IBD which usually responds to conventional treatment. Biological anti-TNF agents (such as infliximab) can be effective in refractory cases.
Please cite this article as: Brunet E, Martínez de Sola M, Garcia-Iglesias P, Calvet X. Púrpura trombocitopénica inmune asociada a enfermedad de Crohn con respuesta completa a infliximab. Gastroenterol Hepatol. 2019;42:37–38.