Intussusception is a rare cause of obstruction in adults. The most frequent location is the small intestine, with colonic intussusception accounting for only 5% of all cases. Most cases are due to an underlying cause which, in the colonic form, is usually a neoplasm. Benign causes are rare, and colonic anisakiasis is an exceptional aetiology.1,2
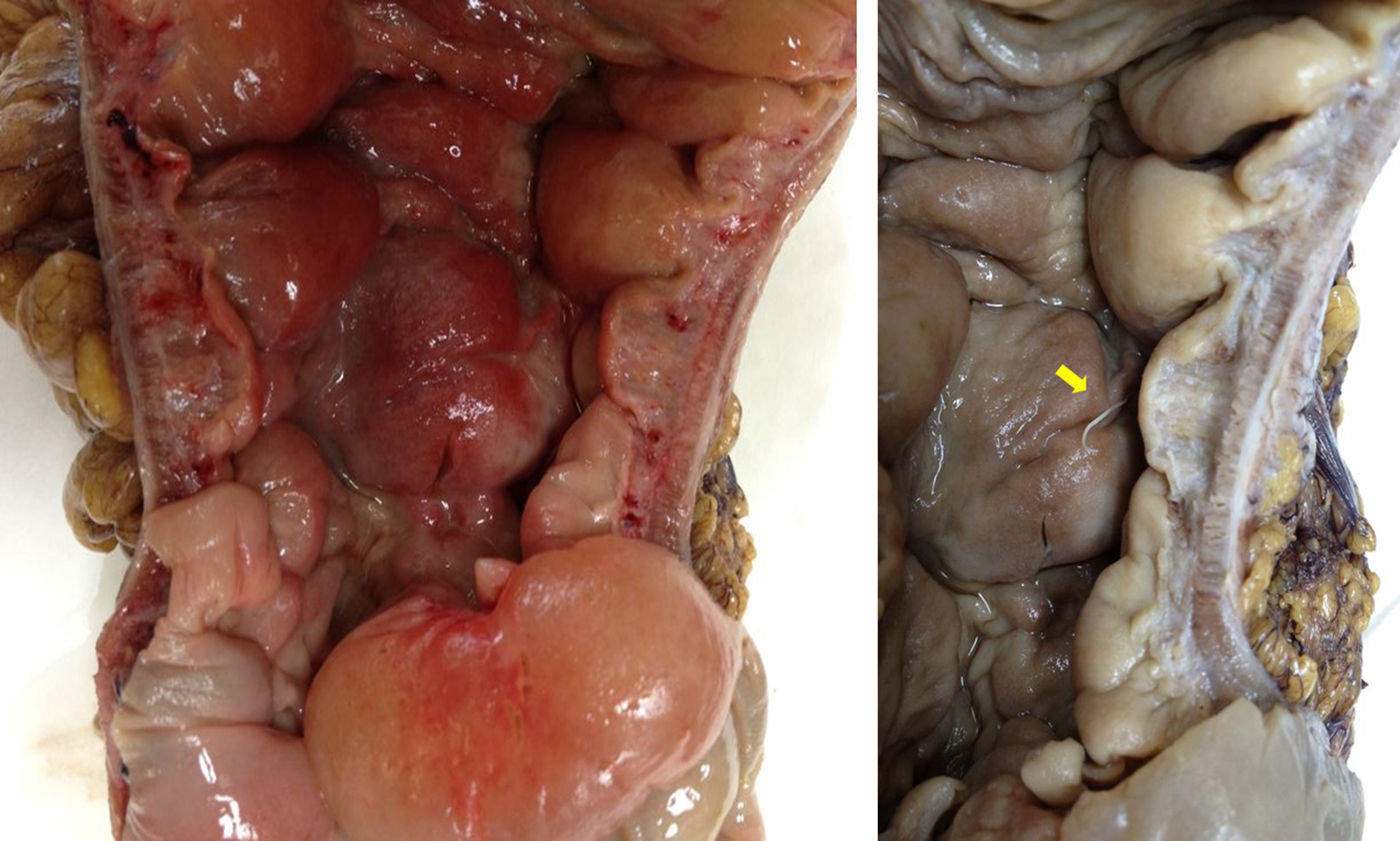
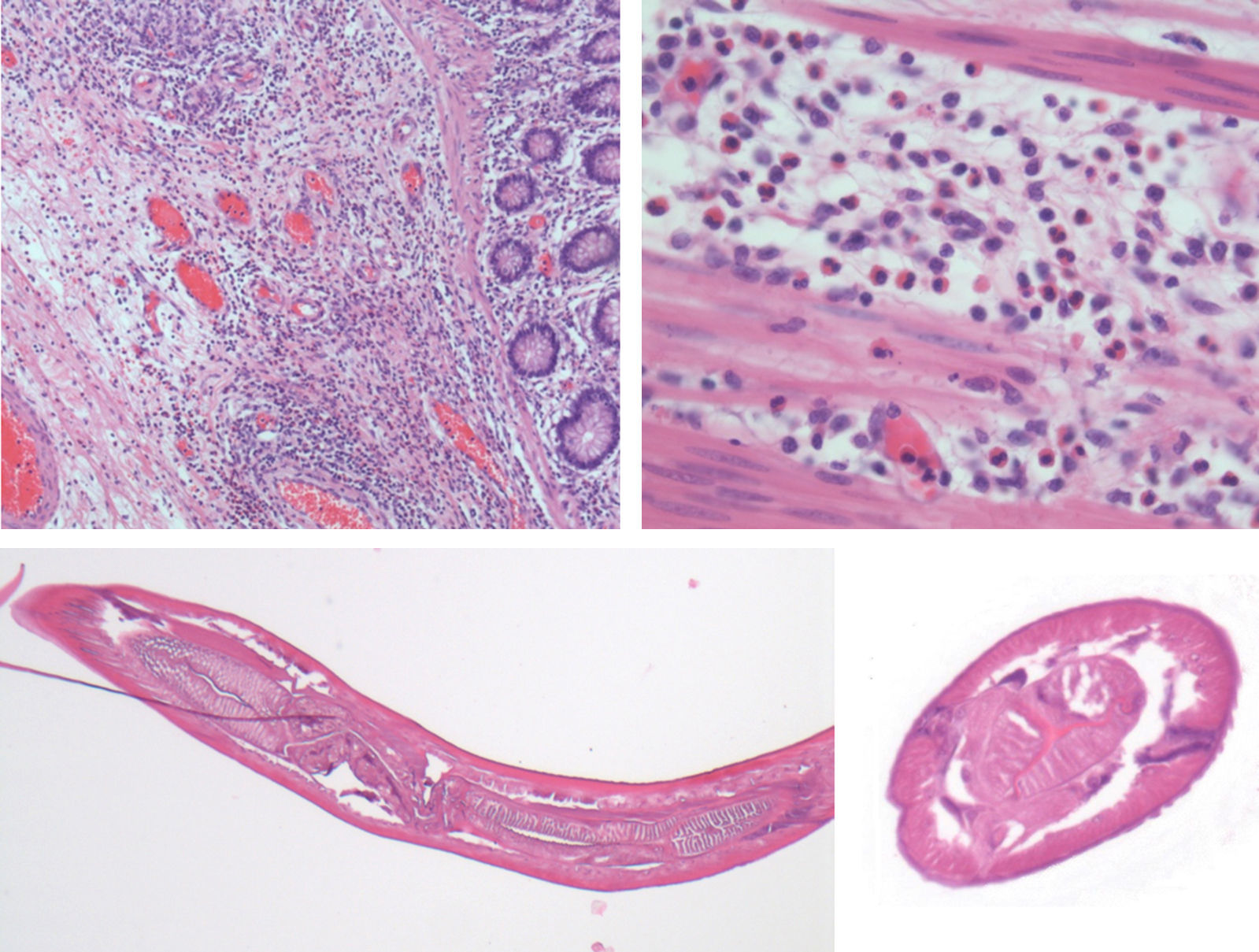
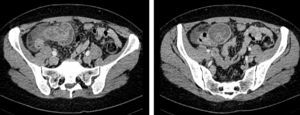
A 48-year-old woman came to the emergency department with mesogastric colic pain lasting 24hours. She reported nausea, without vomiting, and absence of intestinal transit. A tender, palpable periumbilical mass was identified in the examination. Laboratory results showed elevated levels of acute phase reactants, moderate leukocytosis, but no eosinophilia. A CT scan was performed due to suspicion of a complicated tumour, and colonic intussusception of uncertain aetiology was observed, with fluid collection in the right iliac fossa and recto-uterine pouch, as well as evidence of intestinal distress (Fig. 1). Performing a colonoscopy was ruled out due to the suspicion of complicated tumour, and urgent surgery was decided on the basis of the CT findings. The laparotomy showed colonic intussusception extending from the start of the ascending colon to the transverse colon, with no caecal involvement. A right hemicolectomy was performed, with good postoperative progress. Pathological anatomy identified a whitish, filiform structure compatible with an anisakid nematode located in the mucosa of the ascending colon (Fig. 2), as well as significant oedema and inflammatory eosinophilic infiltrate, causing colonic intussusception (Fig. 3).
Colonic intussusception caused by anisakiasis is a rare entity that usually presents in the ascending colon, although it can sometimes occur in the sigmoid colon and rectum.1,3 Preference for the ascending colon is probably due to the distance from the entry point, as the larva must travel from the mouth to the colon, and its survival is affected by the pH changes that occur along the gastrointestinal tract.3,4 Colonic intussusception, i.e. the telescoping of a segment of colon into the lumen of the adjacent segment, is very rare, and is usually caused by a malignancy. For all these reasons, anisakiasis is an exceptional cause of colonic intussusception. Only 6 cases of colonic intussusception due to anisakiasis have been described in the literature, in addition to this case.1,4–8
Accurate diagnosis is difficult, especially in the absence of a history of fish consumption. In cases of diagnostic suspicion, colonoscopy can reduce the intussusception and confirm the diagnosis of anisakiasis.3 Ultrasound can be useful in the diagnosis of intussusception, but the CT scan is the method of choice because it can pinpoint the site of intussusception and assess the extent of the obstruction and intestinal viability.5 Three CT patterns considered pathognomonic of intussusception have been described: the target-like pattern (round mass with intraluminal soft-tissue and eccentric fat density due to the invaginated mesentery), the reniform pattern (a bilobed mass with high peripheral attenuation due to thinning of the bowel wall) or lesion with alternating areas of attenuation related to the bowel wall, mesentery, fluid, contrast material, or gas.2
When the diagnosis is suspected, treatment can be conservative, with nil by mouth and fluid therapy, anthelmintics and corticosteroids to reduce parietal oedema, in addition to endoscopic reduction of the intussusception. However, in the absence of a definitive diagnosis, the optimal treatment is not clearly established. Surgery tends to be necessary in most cases due to obstruction, perforation or suspicion of underlying malignant lesions, since anisakis infection produces submucosal tumours that are the cause of the intussusception and require a histological differential diagnosis.1,4,5
Please cite this article as: Ruiz de la Hermosa A, Ortiz Johansson C, de Fuenmayor ML, Casado Fariñas I, Seoane González JB. Invaginación colocólica por anisakiasis, una causa infrecuente de obstrucción intestinal. Gastroenterol Hepatol. 2017;40:680–682.