Mantle cell lymphoma, which was first described in 1991 and recognised by the World Health Organisation (WHO) as a disease in 1994, is a type of B-cell non-Hodgkin lymphoma originating from B lymphocytes located in the mantle of a lymph node. It is characterised by expression of B-cell lineage markers (CD19, CD20 and CD5), where CD3, CD10 and CD23 are negative and a chromosomal translocation t(11; 14) causes overexpression of cyclin D1.1 Mantle cell lymphoma is a rare type of B-cell non-Hodgkin lymphoma, and accounts for just 3–10% of all non-Hodgkin lymphomas.2 Its incidence in Spain is very low (0.5 per 100,000 inhabitants/year),3 mainly affecting men (2:1) and individuals over 60 years of age. This aggressive lymphoma has a mean survival of 3–5 years after diagnosis,1 but, thanks to therapeutic advances and intensive strategies, survival has doubled in the last decade (60% survival at 5 years).4
Gastrointestinal involvement, with an incidence of 10–25%, is rare, with the most common manifestation being multiple lymphomatous polyposis, in which multiple lymphoid polyps are identified in the large and small intestine. The polyps usually occur in the ileocaecal region, although they can develop at any site from the stomach to the rectum.5 They affect the colon and rectum in 90% of cases, the small intestine in 69%, the stomach in 57%, and the duodenum in 52%.6 Endoscopic diagnosis is rare. Cases with microscopic invasion and normal mucosa on examination have been reported.4
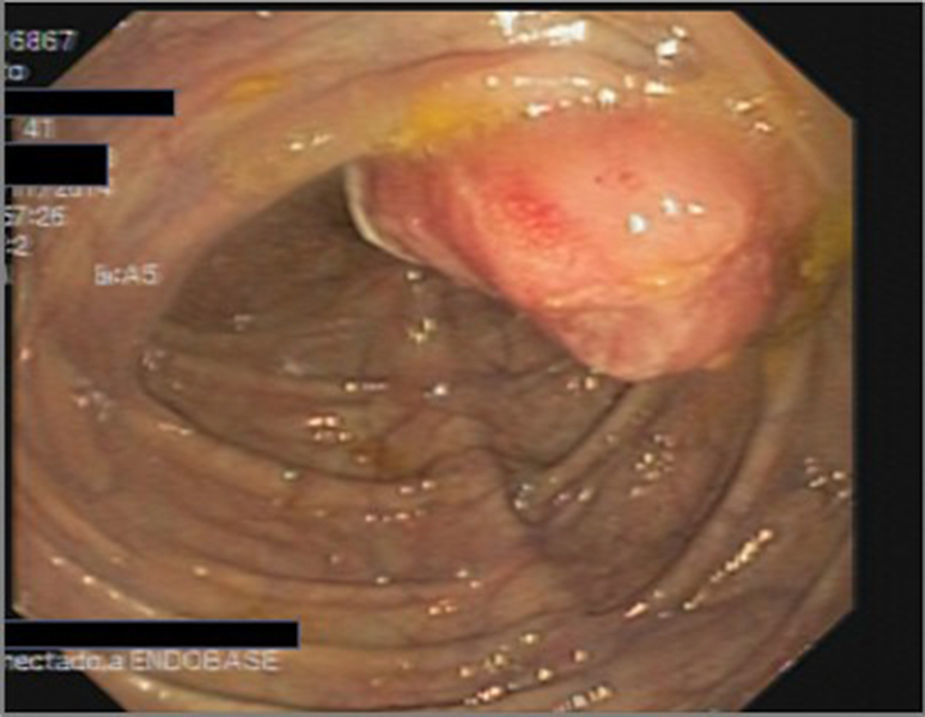
We present the case of a 41-year-old man with a history of hypercholesterolaemia. He was seen by the gastroenterologist due to an increase in the number of bowel movements and rectorrhagia lasting several days, with no other accompanying symptoms and no weight loss, abdominal pain or fever. The physical examination revealed splenomegaly. Laboratory tests found significantly elevated LDH levels; other biochemical parameters and blood count were normal. A colonoscopy was requested, which revealed a friable, ulcerated sessile polypoid lesion (Fig. 1) measuring about 30–40mm located in the caecum, from which multiple biopsies were taken. It was impossible to pass the scope through the ileocaecal valve, despite several attempts. Based on our findings, we requested a contrast-enhanced thoracoabdominal CT scan (Fig. 2), which showed multiple mediastinal, mesenteric, retroperitoneal and pelvic adenopathies, as well as a large mass extending over the superior retroperitoneal vessels.
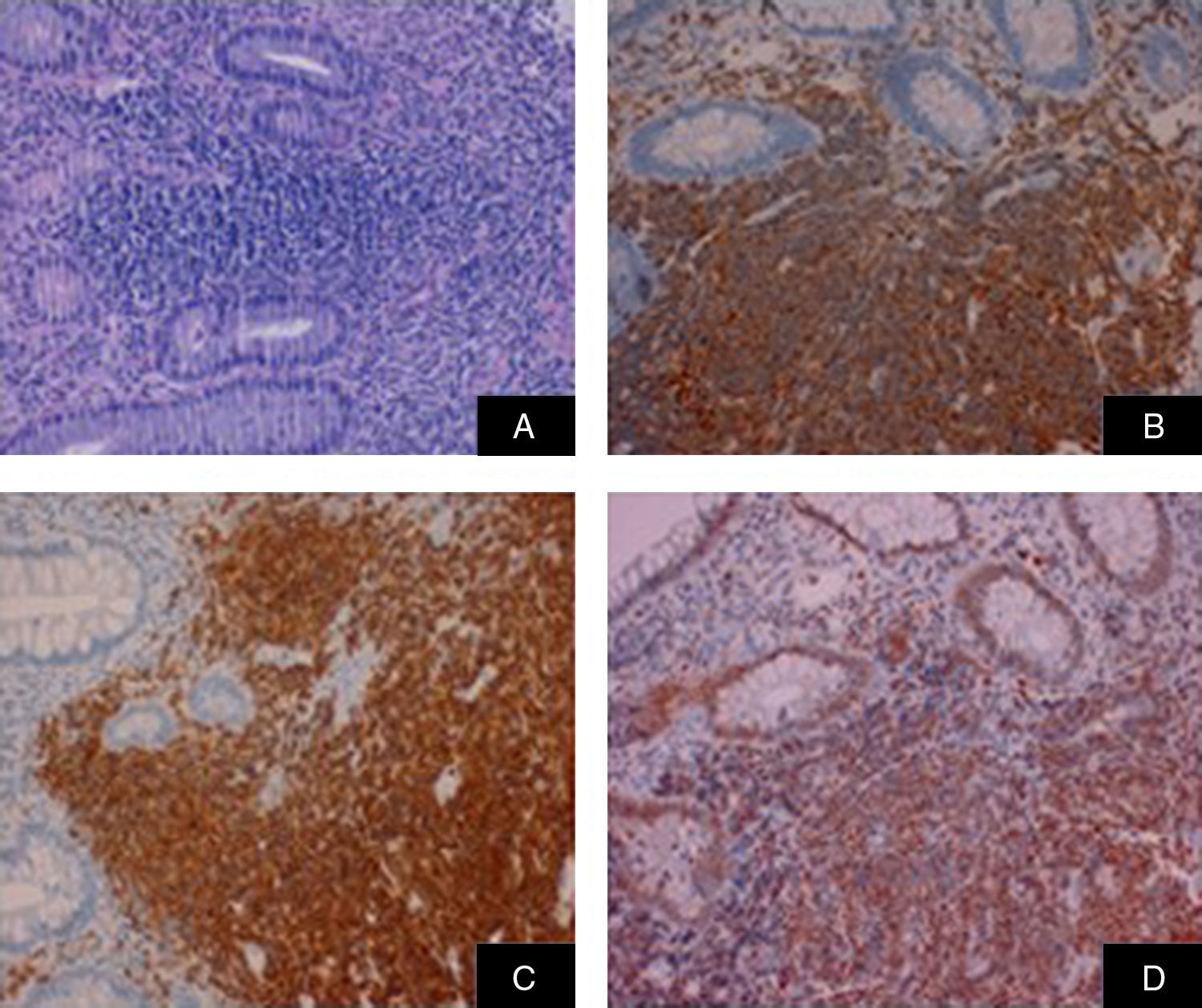
The histological outcome (Fig. 3) of the endoscopic biopsies showed an atypical lymphoid proliferation with strong expression of CD20, CD5 and cyclin D1 in over 75% of B lymphocytes, compatible with infiltration by B-cell non-Hodgkin mantle cell lymphoma. The study was completed with a PET/CT scan that showed supra- and infra-diaphragmatic lymphatic involvement, lymphomatous splenomegaly, diffuse bone marrow and colon involvement, compatible with metabolic stage IV of the disease.
The patient was started on an alternating regimen of 6 cycles of rituximab-cyclophosphamide, vincristine, prednisone (R-macro CHOP)/rituximab-dexamethasone, cisplatin, cytarabine (R-DHAP), with complete response. The 6-month follow-up thoracoabdominal PET/CT scan showed no evidence of pathological radiotracer uptake. Follow-up gastroscopy and colonoscopy showed no lesions. Given the patient's good response to intensive therapy, treatment was consolidated with autologous peripheral blood stem cell transplantation (PBSCT). One year after the PBSCT, the patient remains in full remission on maintenance treatment with rituximab.
Our patient is under 60 years of age, with the distinctive characteristic of presenting with a single large polyp instead of multiple lesions. In 90% of patients, symptoms are non-specific, and include: weight loss, asthenia, lethargy, fatigue, anaemia, palpable abdominal or rectal mass and palpable lymphadenopathy. Bone marrow involvement is seen in advanced stages.7 In the case of gastrointestinal involvement, digestive symptoms have been reported in 15–30% of patients. Endoscopic studies are recommended mainly if there is abdominal pain, changes in bowel movement or rectal bleeding, which was observed in our patient.6
Mantle cell lymphoma is considered an aggressive, rapidly progressive type of lymphoma, and 80% of patients are diagnosed at advanced stages.7 A prognosis must be performed to improve treatment. Prognostic indices permit clinicians to develop treatment strategies based on the patient's particular risk factors. The Mantle Cell Lymphoma International Prognostic Index (MIPI) is used for prognosis in mantle cell lymphoma.8 In patients under 60 years of age and/or with a high MIPI index score, intensive therapeutic strategies with R-CHOP, R-bendamustine and/or R-DHAP followed by PBSCT are recommended.9 Our patient had a score of 8 points on the MIPI, which indicates a high risk (estimated average survival of 29 months), and for this reason received intensive therapy with R-macro CHOP/R-DHAP followed by consolidation with PBSCT. He remains in full remission 30 months after the initial chemotherapy treatment.
Prognosis is poorer in older patients with advanced disease at diagnosis, low albumin, splenomegaly, anaemia and elevated LDH levels.9
We would like to thank the staff of the Anatomical Pathology Department of the Hospital Virgen Macarena for providing complete biopsy images, and the Haematology Department of the Hospital Virgen de Valme for providing information on the management of these cases.
Please cite this article as: Guerra Veloz MF, Maldonado Pérez MB, Caunedo Álvarez A, Gutiérrez Domingo A. Pólipo único colónico como forma de presentación de linfoma del manto. Gastroenterol Hepatol. 2017;40:682–684.