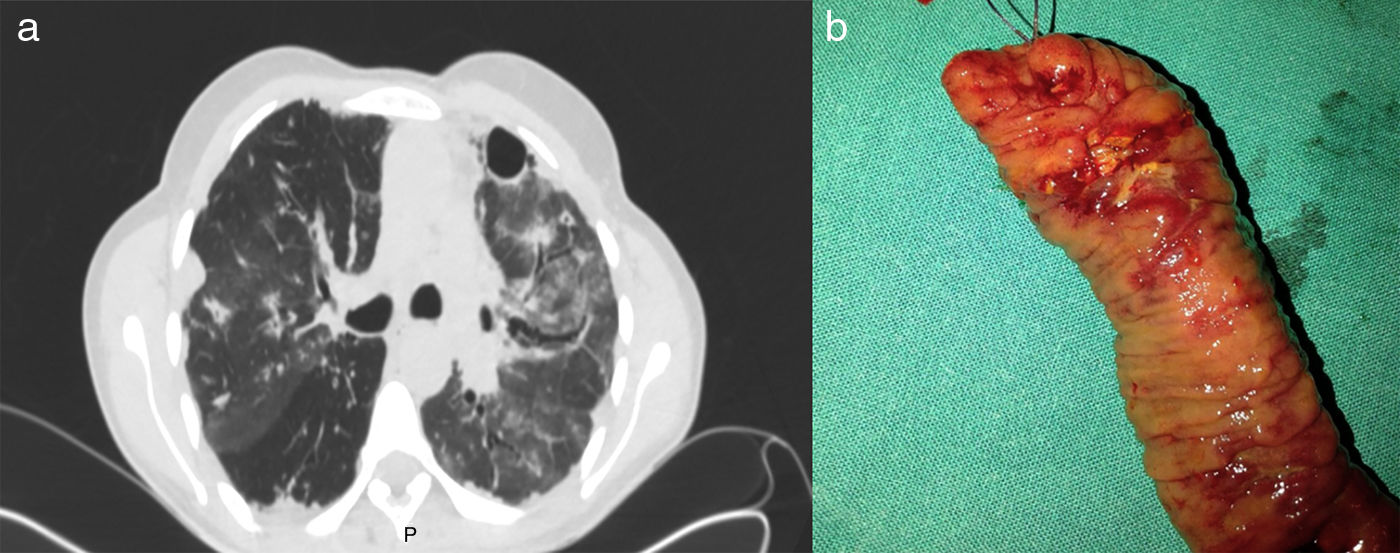
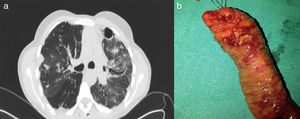
This case involved a 49-year-old woman with a history of bronchial asthma who consulted with dyspnoea. Blood tests showed a normal white blood cell count with 60% eosinophils and chest X-ray revealed an emphysematous chest with symmetrical bilateral interstitial infiltrates. Computed tomography of the thorax showed fibrothorax with a “honeycomb” pattern, bronchiectasis and subpleural bullae (Fig. 1a). Tests were completed with Legionella/pneumococcal antigens in urine, Mantoux and smear microscopy, antinuclear antibodies, anti-neutrophil cytoplasmic antibodies, angiotensin-converting enzyme, immunoglobulins and alpha-1-antitrypsin; all negative, apart from isolation in the culture of an Aspergillus fumigatus and confirmation in the smear of peripheral eosinophilia. With the suspected diagnosis of either chronic eosinophilic pneumonia or pulmonary aspergillosis, treatment was started with methylprednisolone (1.5mg/kg/day) and voriconazole (4mg/kg iv/12h for 7 days) with a good clinical/radiological response. The patient was discharged ten days later on a descending corticosteroid regimen and oral voriconazole (200mg/12h). Forty-eight hours later she was re-admitted with acute abdominal pain and generalised peritonism. Laboratory tests showed leucocytes 9100 (PMN: 91.5%, eosinophils 0%). An X-ray of the abdomen was requested, which showed pneumoperitoneum, and an abdominal computed tomography confirmed the diagnosis of intraperitoneal perforation with associated fluid collection in the right iliac fossa. The patient had emergency surgery, with intraoperative findings of purulent peritonitis with interloop abscesses and multiple perforations in the proximal ileum (Fig. 1b). Examination of the surgical specimen found an eosinophilic inflammatory infiltrate in lamina propria and submucosa, and granulomas and eosinophilic infiltrates in small vessels, compatible with eosinophilic vasculitis. The patient was diagnosed with eosinophilic granulomatosis with polyangiitis and started on treatment with cyclophosphamide (2mg/kg/24h) in addition to the corticosteroids for six months (Five-Factor Score criteria). At present she is on maintenance therapy with azathioprine (1.5mg/kg/day).
(a) Computed tomography (CT) scan of the thorax. Signs of fibrothorax with patchy honeycomb pattern, and increase in density due to possible left interstitial pneumonia. Small cylindrical bronchiectasis and bullous pattern with some subpleural bullae. (b) Surgical specimen. Segment of ileal resection with macroscopic evidence of ulcers in the surgical specimen.
Eosinophilic granulomatosis with polyangiitis or Churg-Strauss syndrome is one of the most uncommon forms of vasculitis. It affects small and medium-sized vessels and is characterised by a vascular and extravascular eosinophilic infiltrate and the formation of granulomas.1
Eosinophilic granulomatosis with polyangiitis usually has three distinct phases1,2: (a) prodromal phase, characterised mainly by respiratory symptoms (asthma, rhinitis, etc.); (b) eosinophilic phase, defined by peripheral eosinophilia and infiltration in multiple organs, particularly lung and gastrointestinal tract; and (c) vasculitis phase, with systemic vascular involvement of small and medium-sized vessels.
Gastrointestinal symptoms affect half of patients and may precede or run concurrently with the vasculitis phase.3 The sections most commonly affected are the stomach and duodenum, followed by the colon, and in most cases ulcers and erythematous lesions are detected by endoscopy. Involvement of the ileum is uncommon, with few documented cases like our patient where it became a surgical emergency.4,5
The American College of Rheumatology proposes six defining criteria for diagnosis of eosinophilic granulomatosis with polyangiitis: asthma; eosinophilia >10% of leucocytes (or absolute count >1500/mm3); paranasal sinus abnormalities; migratory/transient lung infiltrates detected radiologically; poly/mononeuropathy; and biopsy of the vessels showing accumulation of eosinophils in extravascular areas.2 If four or more of these criteria are met, the diagnosis can be made with a sensitivity of 85% and a specificity of 99.7%, respectively. However, it is unusual for the symptoms to occur acutely. At the time of diagnosis, most patients do not meet the four necessary criteria as they tend to develop gradually, so a high degree of suspicion is essential.
The difficulties in demonstrating vasculitis histologically complicates the diagnosis. In the vast majority of patients with gastrointestinal involvement, endoscopy biopsies tend only to show apparently non-destructive eosinophilic vascular infiltration. Typical vasculitis or granulomas are usually only documented in surgical specimens or post-mortem examinations, greatly broadening the differential diagnosis to other conditions that cause gastrointestinal eosinophilia.3 Moreover, the sequential onset of the different symptoms and the treatments used can also mask some signs, making diagnosis even more difficult. In our case, corticosteroid therapy for the patient's respiratory condition would have masked the peripheral eosinophilia when she was re-admitted with abdominal pain.
To conclude, a high degree of suspicion is required for diagnosis of eosinophilic granulomatosis with polyangiitis with gastrointestinal involvement because of the different ways in which it presents and its sequential course. Histological documentation of vasculitis and granulomas is rare, as in most cases only perivascular eosinophilic infiltrate is evident, and this can make diagnosis even more difficult.
Please cite this article as: Martín-Lagos Maldonado A, Pérez Moyano S, Gallart Aragón T. Granulomatosis eosinofílica con poliangitis: informe de un caso. Gastroenterol Hepatol. 2018;41:638–639.