Splenosis is defined as the heterotopic transplantation of splenic tissue after abdominal trauma or splenectomy.1 It is a benign and acquired condition. Implants can be multiple in number, and located both intraperitoneal and extraperitoneal; other locations include pleural cavity, pelvis, subcutaneous tissue, thoracic cavity, cerebrum and liver.2 Most cases are incidental findings during surgery, autopsy or after imaging studies for other purposes. Splenosis occurs in up to 67% of patients with a history of traumatic splenic rupture.3
Splenosis was first described in 1937 by Shaw and Shafi, and the term was introduced in 1939 by Buchbinder and Lipkoff when describing an intraabdominal splenic deposit in a young woman following splenectomy for splenic rupture.4 The average interval between trauma and abdominal or pelvic splenosis is 10 years (range 5 months to 32 years).5
Here we present the case of a 46 years old man with a history of traumatic splenic rupture without splenectomy in 1993. He had a past history of smoking, hypercholesterolemia, and HIV infection diagnosed in 2008, under HEART treatment and with good clinical and analytical control.
A lumbar CT scan was performed in March 2015 to assess chronic lower backpain. Images showed the presence of a gastrohepatic lymphadenopathy, and nodules located adjacent to the pancreatic tail, warranting an abdominal CT scan.
Physical examination of the patient was normal, without abdominal pain or presence of palpable masses in the abdominal cavity. Laboratory tests (hemoglobin 15.90g/dL, red cell count 4.88×1012/L, platelets 321,000/mL, bilirubin 0.4mg/dL, lactate dehydrogenase 161U/L) were within normal parameters. Tumoral marker CA 19.9 (carbohydrate antigen 19.9) level was within normal range (15.98U/mL).
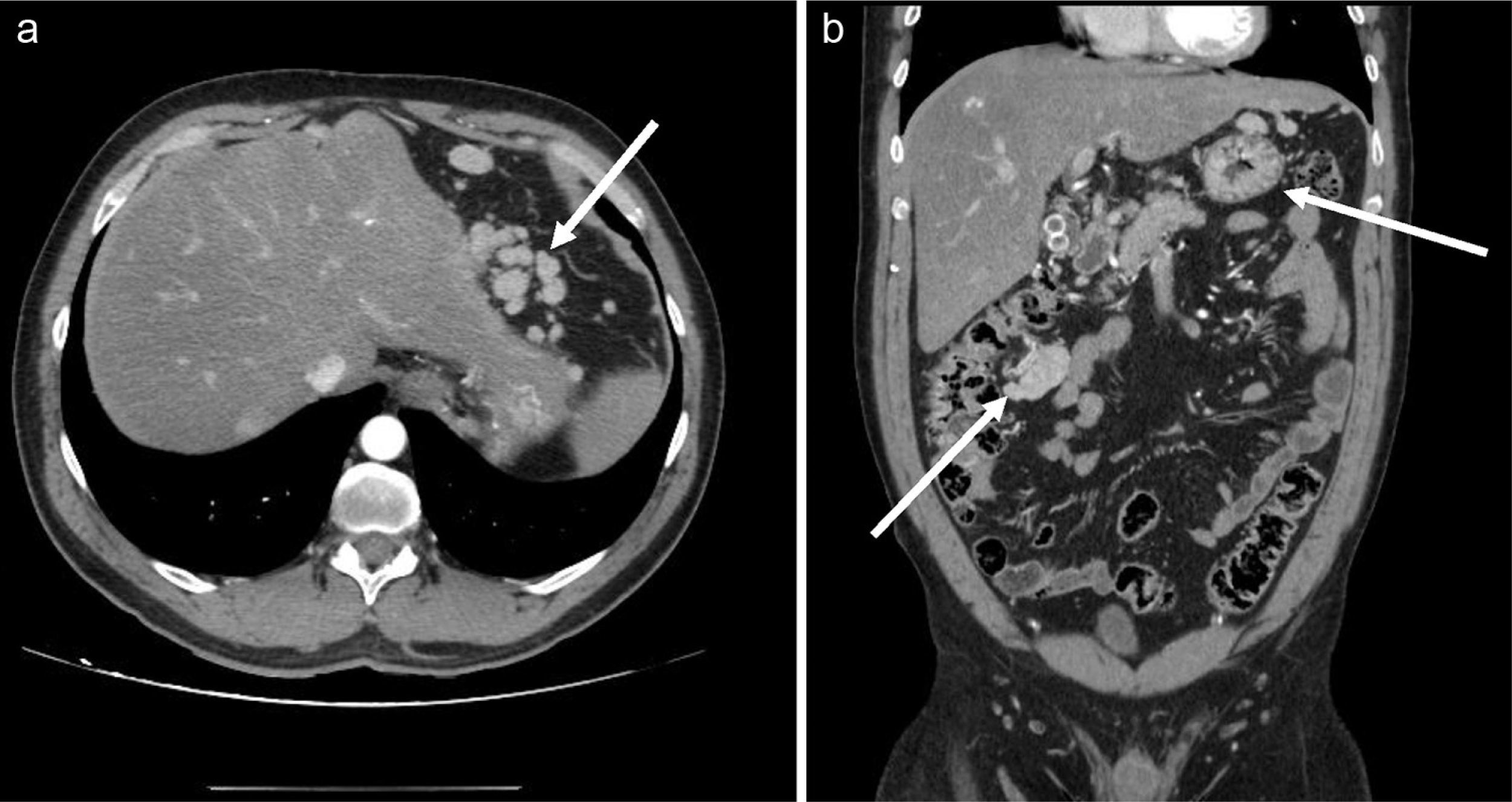
The CT study (May 2015) showed multiple intraperitoneal nodules of various sizes, located in left and right hypochondriac regions, epigastric region, subdiaphragmatic region, and gastrohepatic, compatible with splenosis (Fig. 1). An MRI scan was recommended for diagnostic confirmation. Images show multiple pseudonodular lesions located intraperitoneously, which are consistent with the diagnostic approach. A gastroscopy was also performed, with normal results, ruling out the presence of masses.
Due to the increase in imaging studies performed for diagnostic purposes, incidental findings are acquiring greater importance. When imaging studies of a lesion in a patient with splenic trauma or splenectomy are compatible with normal splenic tissue, the diagnosis of splenosis should be considered.
Pre-contrast MRI shows a homogenously hypointense lesion on T1-weighted images with a hypointense rim around the mass, and hyperintense on T2-weighted images. After contrast administration, the lesion is hyperintense as compared to the liver. The presence of a rim surrounding the lesion is a characteristic finding of splenosis. The rim represents a thin layer of fat or fibrous capsule, showing low signal intensity on T1- and T2-weighted images.
It is believed that splenosis is a fairly common phenomenon of splenic injury, with a reported occurrence in 16–67% of patients with splenic trauma or surgery history.6 Because of the increase in prevalence of abdominal trauma due to all kinds of accidents, abdominal splenosis may appear more frequently in clinical practice than in the past.7 Splenosis has scarce clinical significance. Patients may occasionally present with unspecific abdominal pain, enlarged abdominal mass, intestinal obstruction, gastrointestinal hemorrhage, or hydronephrosis.8 Occasionally, these findings can be confused with malignant pathology, leading to invasive techniques, frequently unnecessary.