In many cases, the differential diagnosis of subacute and chronic diarrhoea represents a challenge. It represents an even greater challenge in patients with underlying psychiatric disease, in whom it can be difficult to distinguish disorders caused by this morbidity from other unrelated signs and symptoms.
We present the case of a 26-year-old patient, a smoker with a history of borderline personality disorder and long-term bulimia nervosa, who had required admission to a psychiatry department for a month, during which time her medication had been adjusted. She visited the emergency department because, after adhering to a highly restrictive diet for two weeks, she presented signs and symptoms consistent with epigastric pain and an increased frequency of bowel movements (up to 10 per day), with watery stools without blood or mucus.
Blood testing revealed compensated metabolic acidosis and mild hypokalaemia, as well as a slight increase in acute-phase reactants. A decision was made to admit the patient to the internal medicine department for testing.
During her stay on the ward, a full microbiology test was done, including for C. difficile, which was negative. With these results, the patient was started on treatment with loperamide, and the frequency of her bowel movements decreased by half. In addition, full immunology and endocrinology tests were ordered, along with clinical chemistry testing of faeces. These showed no indicators of malabsorption, occult blood in faeces, presence of immediate substances or markers of exocrine pancreatic failure.
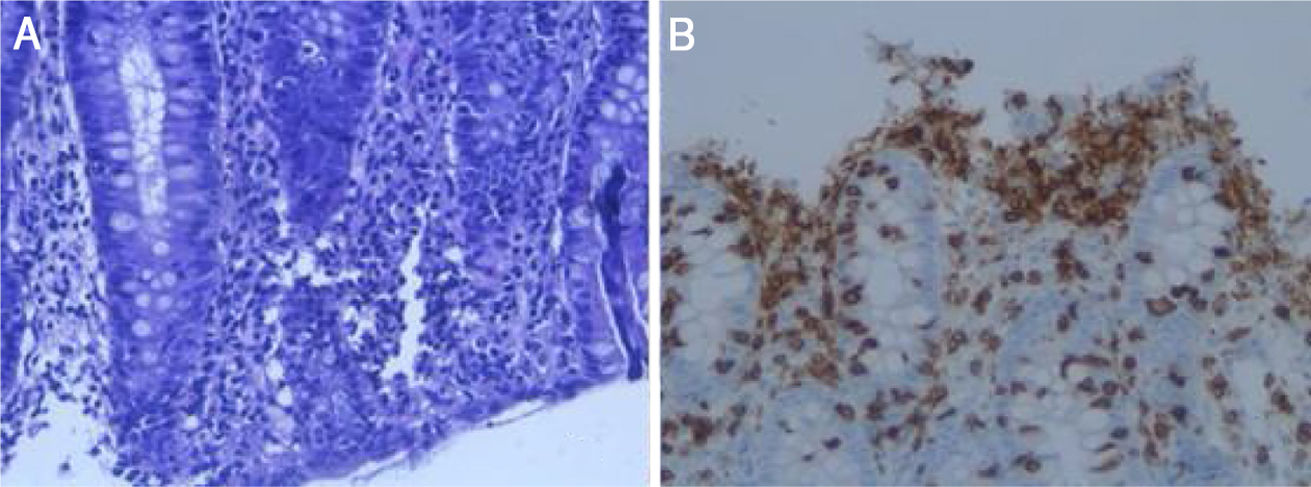
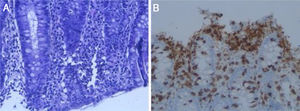
As the patient’s symptoms persisted, an upper gastrointestinal endoscopy was performed. This showed antral gastritis and suspected duodenal atrophy. The biopsies taken revealed no abnormalities. Moreover, a colonoscopy was performed and showed no macroscopic abnormalities. However, mucosal biopsies taken identified a pattern consistent with lymphocytic colitis (Fig. 1).
The patient’s medical record was reviewed and it was confirmed that, during her prior admission, she had been started on duloxetine. Given the reported link between this drug and lymphocytic colitis, a decision was made to suspend this treatment.
The final diagnosis was lymphocytic colitis in relation to duloxetine, a serotonin and norepinephrine reuptake inhibitor that had been recently added to her treatment as an antidepressant. The patient's condition improved after she was taken off duloxetine.
Lymphocytic colitis is a subtype of microscopic colitis that clinically manifests as chronic watery diarrhoea without blood or mucus.1 Its diagnosis requires a strong suspicion, as its main characteristic is the absence of macroscopic abnormalities in the colon mucosa.1 Hence, a pathology study of the colon mucosa is crucial, since it demonstrates the presence of intraepithelial lymphocytes (≥20 lymphocytes per field) in the colon mucosa.
Regarding aetiology, a genetic susceptibility has been found. In addition, it is reportedly linked to tobacco use and certain drug groups, including proton pump inhibitors, non-steroidal anti-inflammatory drugs and serotonin reuptake inhibitors.1
The main treatment consists of stopping the drug that triggered the diarrhoea. In some cases, it is advisable to use loperamide for managing symptoms. If the episode is not managed with these measures, treatment with budesonide can be added. In recent years, the use of mesalamine, cholestyramine and beclometasone has also been proposed, although there is not yet enough evidence in this regard.2
To date, only two cases of lymphocytic colitis associated with duloxetine have been reported in the literature,3,4 which means there is a lack of evidence as to the best treatment for these patients. However, in the previously reported cases, as in the case reported herein, it was not necessary to use budesonide to improve the patient's lymphocytic colitis symptoms. The severity of and the treatment of this pathology may vary, depending on what triggered it. More studies are needed to establish guidelines for the most suitable management of this condition.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Millán-Nohales C, Ordieres-Ortega L, García-Martínez R. Colitis microscópica linfocítica asociada a duloxetina: descripción de un caso y revisión de la literatura. Gastroenterol Hepatol. 2021;44:222–223.