Cicatricial pemphigoid (CP) is an uncommon disorder, with oesophageal involvement being particularly rare. Awareness of this condition is vital when performing a differential diagnosis of oesophagitis with ulceration, in order to ensure that fresh biopsies are appropriately processed so as to enable the pathologist to make a definitive diagnosis.
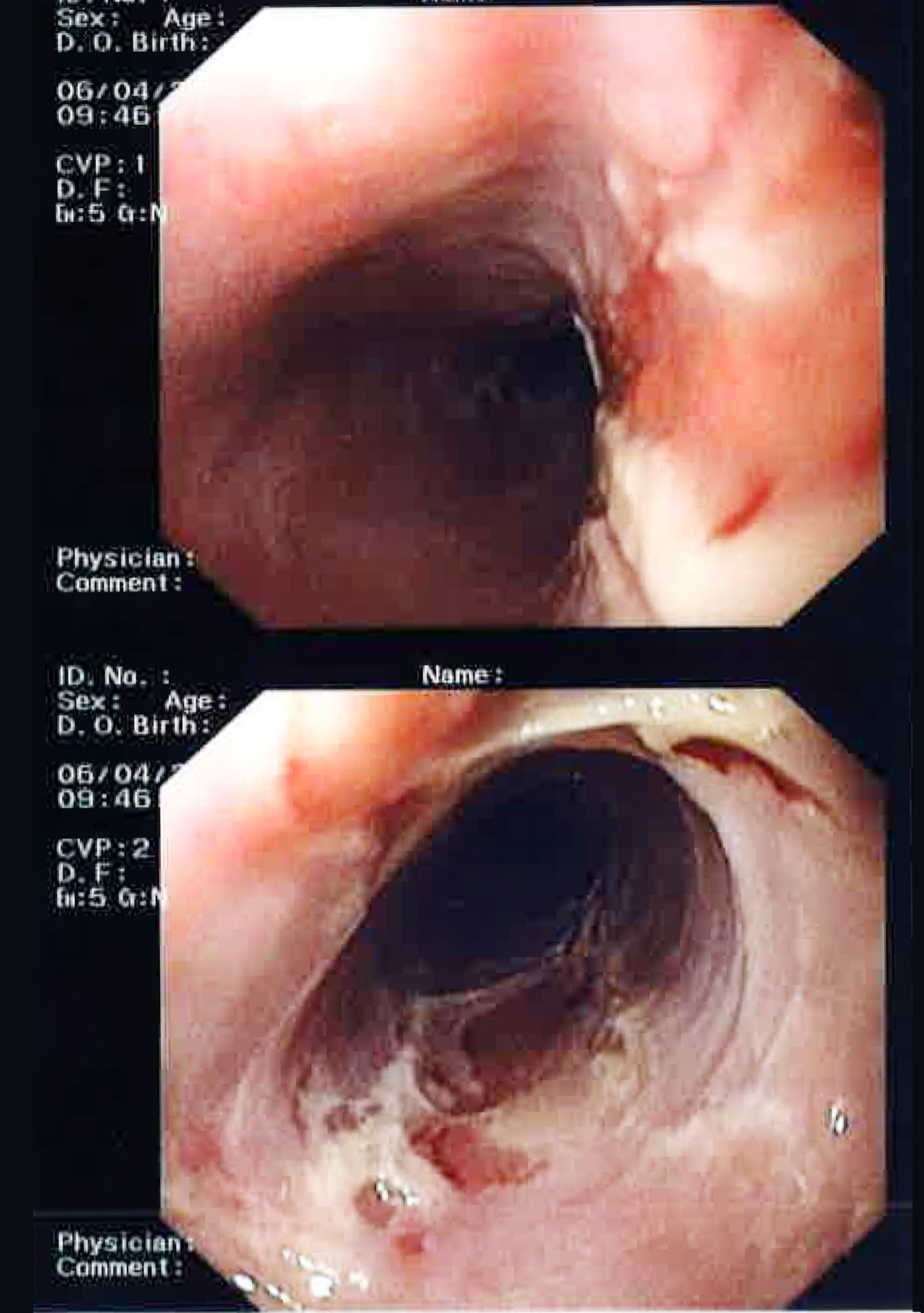
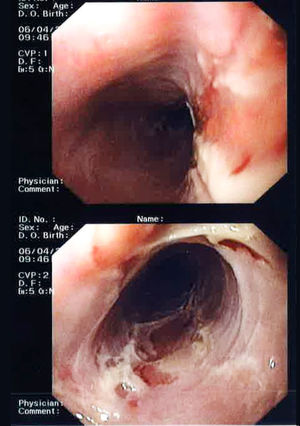
We present the case of a 62-year-old woman who attended the clinic due to a six-month history of dysphagia, primarily to solids. Prior history of interest included the recurrence of sores in the oral cavity that had not previously been examined. A gastroscopy was performed that revealed denuded oesophageal mucosa with widespread superficial ulceration and fibrinoid material, with no apparent stenosis (Fig. 1). The histological study confirmed mucosal changes consistent with ulceration; the Grocott stain for fungi and the stains and cultures for cytomegalovirus (CMV), herpes simplex virus (HSV) and Epstein-Barr virus (EBV) were negative. The patient began empirical treatment with omeprazole for two months with negligible improvement, before being referred to dermatology for examination of her mouth sores. Examination of the buccal mucosa revealed whitish, reticulated plaques of cicatricial appearance, which were biopsied. The histological report identified spongiotic dermatitis with a tendency to subepithelial microvesiculation on the edge of the slide itself in the presence of histiocytic and neutrophilic infiltrate, all suggestive of mucosal CP. In light of these results, a second gastroscopy was ordered and a direct immunofluorescence (DIF) histological study on fresh specimens was performed, which confirmed the diagnosis of CP. The patient started treatment with oral prednisone and azathioprine, as well as 0.05% clobetasol propionate, 1% clotrimazole, 2% lidocaine and Orabase® (benzocaine) to treat the mouth sores, with complete resolution of all lesions.
CP, which is also known as benign mucous membrane pemphigoid, is a rare autoimmune disease characterised by the formation of subepithelial blisters, predominantly of the mucous membranes and less commonly affecting the skin.1 Its estimated incidence is 1 per 100,000 population/year and it primarily affects middle-aged women.2–4
It is characterised by the recurrence of blisters on the mucous membranes with a significant tendency to scarring and fibrosis.4 The most commonly affected surfaces are the oral cavity, followed by the conjunctiva, but lesions can also appear on the pharynx, larynx, oesophagus, nasal mucosa and the genital mucosa.3 Skin involvement tends to be less common and predominantly affects the periorificial region, face, scalp and upper trunk.4
The oesophagus is only affected in 3% of cases, generally in disseminated forms of the disease.3 The cervical oesophagus is the region most commonly affected by cicatricial stenosis, membranes and rings.5 Membranes are the initial manifestation, which then give rise to the formation of fibrotic rings and stenosis of the lumen in more advanced stages as a result of the scarring process.1 This leads to the onset of symptoms like dysphagia, gastro-oesophageal reflux, bronchopulmonary aspiration and chronic cough. Involvement of the extraoral mucosa, including the oesophageal mucosa, is considered to be of higher risk due to its greater tendency to scar and the subsequent onset of functional limitations.2
The aetiopathogenesis of CP is the deposit of IgG or IgA autoantibodies and complement in the epidermal and/or mucosal basement membrane. The identification of these complexes with a linear pattern in a tissue sample by DIF is the diagnostic gold standard, with high sensitivity and specificity (80–100%). In 25% of cases, circulating antibodies can be detected at low titres. Diagnostic suspicion is essential to ensure biopsies are taken, processed fresh and subsequently analysed by DIF.1,6
CP management depends on the clinical manifestation and severity of the symptoms. Oesophageal involvement usually requires systemic treatment with corticosteroids and even immunomodulators like azathioprine or mycophenolate to induce remission and control the underlying disease over time. Therapeutic endoscopy with dilation may be required in refractory cases with stenosis. Follow-up of these patients is essential due to the chronic and recurrent nature of this condition.3,6
Oesophageal cicatricial pemphigoid is a rare condition that clinicians should consider in the differential diagnosis of oesophagitis with ulceration. The conditions to be ruled out include subepithelial bullous dermatosis (bullous pemphigoid, epidermolysis bullosa acquisita, bullous systemic lupus erythematosus), pemphigus vulgaris, lichen planus and infectious oesophagitis.6,7 However, it is important not to forget conditions with which we are more familiar, like Crohn's disease and eosinophilic oesophagitis.
Please cite this article as: Diéguez Castillo C, Martín-Lagos Maldonado A, del Moral Martínez M, Ruiz Escolano E. Penfigoide cicatricial esofágico. Gastroenterol Hepatol. 2019;42:372;373.