Tuberculosis continues to be the infectious disease with the highest mortality worldwide, with more than 1.5 million deaths per year.1 Up to 12.5% of cases are extrapulmonary2 and, although the pancreas is a rare location, its diagnosis is increasing due to the increase in immunosuppressed patients, as well as the improvement of diagnostic tools such as fine-needle aspiration (FNA) by ultrasound endoscopy. There are no pathognomonic clinical or imaging findings, so the index of suspicion must be high to be able to diagnose it.
We present the case of a 59-year-old woman from Venezuela, resident in Spain for 10 years, with no recent trips to her country of origin, and no personal or family history of interest. She was admitted to hospital due to onset of symptoms six months prior, consisting of progressive and continuous epigastric pain of moderate intensity, although with frequent episodes of greater intensity, not clearly related to eating, associated with a recent weight loss of about 5 kg, nausea and occasional feeling of coldness.
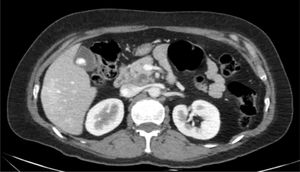
Complementary laboratory tests showed: GGT 180 U/l, ALP 600 U/l, bilirubin 2.5 mg/dl, leukocytes 8,800/mm3, CRP 1.49 mg/dl, CEA 15 ng/mL, CA 19.9 240 U/ml, rest of biochemistry and coagulation normal. An ultrasound and later a CT scan were performed (Fig. 1) which reported: a 45-mm hypodense tumour in the body and head of the pancreas, poorly delimited, surrounding the portal vein and with cystic-necrotic areas inside and presence of peripancreatic adenopathies of 2 cm. Finally, ultrasound endoscopy was performed, where it was observed that the tumour completely surrounded the portal vein without infiltrating it, being in the final stage T2 N1, and because it was a potentially resectable lesion, FNA was not performed. The tumour committee decided on performing a cephalic pancreaticoduodenectomy.
The patient underwent surgery by laparotomy, during which it was noted that the cystic areas of the tumour drained a whitish granular content, an inter-aortocaval node was analysed intraoperatively and showed a caseating granulomatous inflammatory reaction. Due to these findings samples of the adenopathy were sent off in order to perform PCR and culture of Mycobacterium tuberculosis, which were negative. During the postoperative period, HIV−, Mantoux (3.5 mm) and IGRA+ studies were performed. Finally, the pathological anatomy of the surgical specimen reported the absence of malignancy and the presence of foci of caseous necrosis surrounded by epithelioid cells and peri-granuloma lymphocyte reaction in the parenchyma and peripancreatic lymph nodes. Thus the patient was finally diagnosed with pancreatic tuberculosis, a standard anti-tuberculous treatment regimen was started, and during the follow-up appointments the patient reported being asymptomatic, tolerating treatment without complications.
Pancreatic tuberculosis is a disease that is difficult to diagnose. It can readily mimic pancreatic ductal adenocarcinoma (PDAC), and also, on rare occasions (<15%), patients have a history of tuberculosis, which makes its suspicion even more difficult. It is an entity that must be particularly suspected in relatively young patients (40 years) from endemic areas (Asia, Africa, South America), but also in immunocompromised patients, since in up to 20% it is associated with HIV.3 Clinically, it is indistinguishable from an PDAC, although occasionally (46%) low-grade fever may manifest, which can be a clue to the diagnosis. The most common form of presentation is in the form of SOL in the pancreatic head, which is hypodense in up to 90% of cases, and blood vessels may be encompassed in a similar way to PDAC, although more atypical data such as masses that are solid-cystic, heterogeneous or with calcifications may sometimes show.4 The diagnosis is made by EUS + FNA, occasionally showing a macroscopic caseous content, and histologically the most typical finding is the presence of caseating granulomas. Other tests that support the diagnosis, although due to the fact that it is a form of paucibacillary TB there is a certain rate of false negatives, are culture (sensitivity: 40–75%) or PCR (sensitivity: 50–70%) of the FNA sample, as well as Mantoux or IGRA (sensitivity: 70%). The standard anti-tuberculosis treatment regimen (rifampicin 10 mg/kg/day; pyrazinamide 25 mg/kg/day; isoniazid 5 mg/kg/day; ethambutol 15 mg/kg/day/for two months, and then four months of rifampicin 10 mg/kg/day + isoniazid 5 mg/kg/day) is effective, although in most cases treatment must be extended from 9 to 12 months.
Please cite this article as: Velamazan R, García S, Hernandez M, Saura N, Hijos G, Abad D, et al. LOE pancreática ¿otro caso de adenocarcinoma pancreático? Gastroenterol Hepatol. 2022;45:207–208.