The causes of sustained elevation of serum transaminases in asymptomatic adults, both hepatic and extrahepatic, are varied. In order to reach an aetiological diagnosis, a standardised protocol should be applied, aimed firstly at ruling out the most common causes, such as chronic hepatitis (viral or autoimmune), metabolic diseases, and toxic liver diseases. Several biochemical patterns, which take into account transaminase, cholestatic enzyme, muscle enzyme, ferritin and ceruloplasmin levels, as well protein electrophoresis and autoantibody measurement, will identify most causes. In cases in which a diagnosis cannot be reached with the use of these non-invasive methods, a needle liver biopsy will be justified.
Las causas de elevación sostenida de las transaminasas séricas en pacientes adultos asintomáticos son muy variadas, tanto hepáticas como extrahepáticas, y hace falta una sistemática estandarizada para alcanzar el diagnóstico etiológico, orientada a descartar en primer lugar las causas más frecuentes, hepatitis crónica, viral o autoinmune, enfermedades metabólicas y hepatopatías tóxicas. Diversos patrones bioquímicos, que tienen en cuenta los valores de cada transaminasa, de los enzimas de colestasis, de los enzimas musculares, de la ferritina y de la ceruloplasmina, así como el resultado de la determinación del proteinograma y de los autoanticuerpos permitirán reconocer la mayoría de causas. En los casos sin diagnóstico mediante métodos no invasivos estará justificada la práctica de una biopsia hepática.
Asymptomatic hypertransaminasaemia is one of the most common reasons for consulting a hepatologist and a common finding among primary care physicians, who often find that the only abnormality or unexpected anomaly in the results of tests carried out for various indications is an elevation of serum transaminases.
Population studies have estimated the prevalence of hypertransaminasaemia to be between 5% and 10% of the population, a percentage that is expected to increase in the future with the global rise in obesity.1–3
In healthy individuals, plasma transaminase is derived from the normal turnover of cells containing this enzyme, mainly hepatocytes and muscle fibres. Serum levels above normal values damages the cell membranes of tissues containing transaminase, thus releasing more intracellular enzymes into the blood.
In most cases of asymptomatic hypertransaminasaemia, transaminases levels are usually less than 5- or 6-fold the upper limit of normal, and may be accompanied by other alterations in liver function tests, suggesting liver disease. If the other tests are normal, the possibility of a muscular instead of a hepatic origin of the transaminases in connection with an inflammatory, toxic or genetic myopathy should also be considered.4–6 Some extrahepatic diseases also present with hypertransaminasaemia resulting from transaminase-induced muscle injury, as in the case of hyperthyroidism, or liver injury, as in the case of coeliac disease,7–10 diabetes mellitus,11–13 hyperthyroidism14 or Addison's disease.15–18
In this article, we examine the different aetiologies associated with this finding in adult patients, except liver transplant patients, and the best method of identifying their aetiology based on the different clinical presentations.
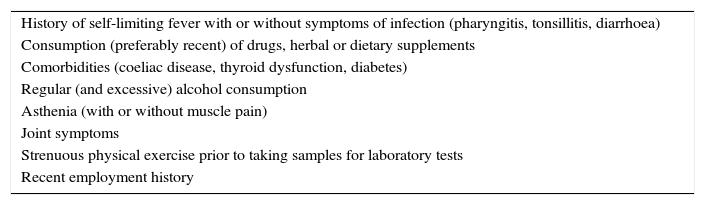
Transient or persistent hypertransaminasemia?It is not uncommon for discreet, isolated hypertransaminasaemia to be detected in a patient with banal symptoms during a medical check-up or blood donation. Before further investigation, which takes time and requires additional tests, a detailed history should be taken in order to identify a possible aetiology (Table 1) and distinguish between a transient and permanent alteration (Tables 2 and 3).
Information elicited when taking the medical history of a patients with asymptomatic elevation of transaminases.
| History of self-limiting fever with or without symptoms of infection (pharyngitis, tonsillitis, diarrhoea) |
| Consumption (preferably recent) of drugs, herbal or dietary supplements |
| Comorbidities (coeliac disease, thyroid dysfunction, diabetes) |
| Regular (and excessive) alcohol consumption |
| Asthenia (with or without muscle pain) |
| Joint symptoms |
| Strenuous physical exercise prior to taking samples for laboratory tests |
| Recent employment history |
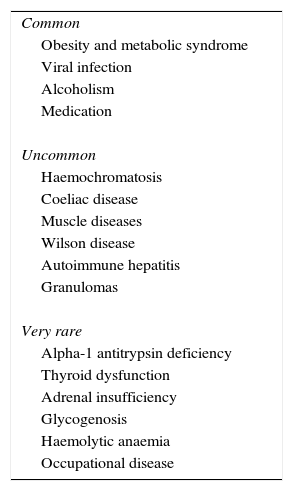
Causes of persistent hypertransaminasaemia (without cholestasis) in adults.
| Common |
| Obesity and metabolic syndrome |
| Viral infection |
| Alcoholism |
| Medication |
| Uncommon |
| Haemochromatosis |
| Coeliac disease |
| Muscle diseases |
| Wilson disease |
| Autoimmune hepatitis |
| Granulomas |
| Very rare |
| Alpha-1 antitrypsin deficiency |
| Thyroid dysfunction |
| Adrenal insufficiency |
| Glycogenosis |
| Haemolytic anaemia |
| Occupational disease |
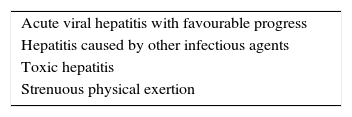
If symptoms suggestive of infection are reported in the days preceding the finding of elevated transaminases, the blood panel should be repeated a few weeks later to see whether levels have returned to normal. If so, the increase will probably have been caused by a self-limiting viral infection such as hepatitis A, Epstein–Barr virus, cytomegalovirus, rotavirus, parvovirus, adenovirus, or some other infectious agent, such as Salmonella or toxoplasma.19–21
If the patient has been taking some form of medication, particularly an antibiotic such as ciprofloxacin or a macrolide, a nonsteroidal anti-inflammatory agent,22,23 or herbal supplement,24,25 these can be discontinued and the blood panel repeated 3 or 4 weeks later. If levels have normalised, the increase can be attributed to the suspended medication.
Some patients with chronic pain take large amounts of paracetamol, without reaching doses that can cause massive liver necrosis (around 10g). A dose of 4g/day or more, taken over a prolonged period of time, can also cause liver damage with elevated transaminases,26 particularly in the presence of dietary hepatic glutathione deficiency (the antioxidant that neutralises the toxic metabolites produced by paracetamol metabolism) or a hepatic enzyme induction due to regular consumption of alcohol.27–30
If the blood panel was performed in the days following unusually strenuous (for the patient) physical effort, such as an athletic endurance test or a bicycle race, the initial suspicion should be release of muscle enzymes. This should be confirmed in a new panel performed a couple of weeks later, in which levels should have normalised.31 Elevated transaminase levels can also occur after physical exercise performed in the gym32 or in patients engaged in body-building.33
If the patient denies the foregoing causes, and the re-test shows persistently elevated transaminase levels, persistent hypertransaminasaemia should be suspected and the following steps taken.
First, determine if transaminase elevation is due to one of the two most common causes of persistent hypertransaminasaemia–non-alcoholic fatty liver disease (NAFLD) and chronic viral infections–for which specific treatment exists.
Metabolic syndrome as a cause of hypertransaminasaemiaThe most common cause of elevated transaminases in adults in the Western world is NAFLD, related to overweight and metabolic syndrome. This is due to insulin resistance, and manifests as the combination of 2 or more of the following disorders: type 2 diabetes, hyperlipidaemia, hypertension and hyperuricemia.34 Therefore, it is reasonable to begin the examination of the patient with asymptomatic hypertransaminasaemia by confirming or ruling out these manifestations. If present, the presumptive diagnosis will be NAFLD-induced hypertransaminasaemia.34 In these cases, an abdominal ultrasound should be performed, in which a hyperechoic pattern caused by fat deposition is usually seen. Attention should be paid to signs suggesting cirrhosis, such as a heterogeneous echogenicity of the liver, an irregular contour, splenomegaly and increased portal vein calibre.
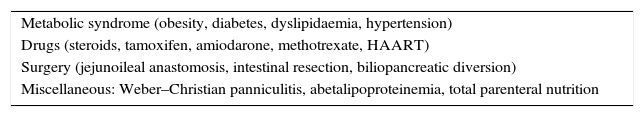
Metabolic syndrome is not always the underlying disease in NAFLD, and other causes (see Table 4) should be considered if a hyperechoic liver pattern is found on abdominal ultrasound. Patients with hepatic steatosis can also present with other diseases associated with hypertransaminasaemia, such as coeliac disease,35,36 Wilson's disease37 or autoimmune hepatitis (AIH).38
Diseases associated with NAFLD.
| Metabolic syndrome (obesity, diabetes, dyslipidaemia, hypertension) |
| Drugs (steroids, tamoxifen, amiodarone, methotrexate, HAART) |
| Surgery (jejunoileal anastomosis, intestinal resection, biliopancreatic diversion) |
| Miscellaneous: Weber–Christian panniculitis, abetalipoproteinemia, total parenteral nutrition |
HAART, highly active antiretroviral therapy; NAFLD, non-alcoholic fatty liver disease.
Anorexia can also cause elevated transaminase levels when it has led to significant malnutrition39; this is more common in young men than women.
Chronic viral hepatitis as a cause of hypertransaminasaemiaThe second most frequent cause of persistent hypertransaminasaemia is chronic viral hepatitis, usually caused by hepatitis B (HBV) or C (HCV) infection in immunocompetent patients. Hepatitis E infection is self-limiting in immunocompetent patients, but can cause chronic hepatitis in transplant patients receiving immunosuppressant therapy.40
In patients with persistent hypertransaminasaemia, a finding of HBsAg and anti-HCV are needed to establish a diagnosis of chronic hepatitis B and C, respectively. The existence of occult HBV and HCV infections that can only be detected by HBV DNA or HCV RNA tests is widely debated. However, irrespective of whether such cases exist or not,41,42 other causes of elevated transaminases should be explored in patients negative for HBsAG and anti-HCV.
Recommended tests in cases of persistent hypertransaminasaemia not attributable to metabolic syndrome or chronic viral hepatitisIf suspicion of a transient alteration not due to NAFLD or chronic hepatitis B or C is not raised during the first visit, further investigations will be needed. The first step should be to rule out the most common, and then the more rare, diseases associated with elevated transaminase levels (Table 3). This can be done with a simple laboratory test. Other studies should include an abdominal ultrasound, which can reveal a diffuse hyperechoic pattern, usually due to steatosis, although glycogenosis should also be considered. It is also helpful to ask the patient about their job to rule out exposure to industrial toxins that are known to cause liver damage.
Assessment of different patterns in blood panel resultsWhen evaluating laboratory findings, it is important to look for certain patterns that can be crucial for diagnosis, particularly serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels.
Elevated AST with normal ALT levels and no abnormalities in other liver function testsThis usually indicates macro-AST. Macro-AST is a high molecular weight macroenzyme formed when AST binds with other plasma components.43,44 Macroenzyme formation delays renal excretion of the enzyme and prolongs its survival, thereby increasing serum levels. It is usually a benign process, although it can be associated with autoimmune diseases or malignancies. It is not associated with liver disease.
AST/ALT ratio above 1In most liver diseases, serum ALT level are usually higher than serum AST, therefore, the AST/ALT ratio is typically less than 1. This rule does not apply to patients with alcoholic liver disease, in which the ratio is usually >2, accompanied by a marked elevation in gamma-glutamyl transpeptidase (GGT),45 greater than that found in non-alcohol-related diseases. The damage caused by alcohol leads, on the one hand, to the release of mitochondrial AST and on the other, to enzyme induction responsible for the elevated GGT levels.46
A high AST/ALT ratio (>1) is also seen in patients with non-alcoholic liver cirrhosis, where, during the chronic hepatitis stage, the ratio will be less than 1.47
In muscle diseases, GGT levels are normal and the AST/ALT ratio is also greater than 1, due to the elevated AST vs ALT content in muscle fibres. The diagnosis of myopathy is confirmed by the finding of significantly elevated creatine phosphokinase (CPK) levels.48,49 When a muscle disease is the underlying cause of elevated transaminases, the patient should be referred to a specialist, as some muscle diseases can remain asymptomatic for many years.
Elevated transaminase and n-alkaline phosphatase levels >3This is usually cause by a cholestatic liver disease, such as primary biliary cirrhosis (PBC) or primary sclerosing cholangitis (PSC). These conditions are always associated with elevated or extremely elevated GGT levels.
If anti-mitochondrial antibodies (AMA) are detected, a diagnosis of PBC can be confirmed without resorting to liver biopsy. In the absence of AMAs, however, imaging studies, such as cholangiopancreatography, must be performed to detect bile duct abnormalities that are typical of PSC. If cholangiopancreatography is normal, a liver biopsy will be needed to confirm or rule out small-duct primary sclerosing cholangitis,50,51 Alagille syndrome,52 granulomas53 or Turner syndrome.54 If the patient presents ulcerative colitis, a diagnosis of small duct cholangitis is very plausible.
Elevated AST, ALT and serum ferritinElevated serum ferritin should not always be taken to indicate haemochromatosis, as it can be due to other causes.55 Haemochromatosis is most likely when transferrin saturation is over 60%. Diagnosis is confirmed with a finding of a homozygous C262Y mutation of the HFE gene.56 If elevated ferritin is accompanied by a hyperechoic liver on abdominal ultrasound and normal transferrin saturation, the most likely diagnosis is not haemochromatosis but NAFLD, which is usually associated with elevated ferritin levels.57
Hypertransaminasaemia with hypergammaglobulinaemiaThe presence of hypergammaglobulinaemia should arouse suspicion that the patient has established cirrhosis or autoimmune hepatitis (AIH). The presence of antinuclear antibodies (ANA) and/or anti-smooth muscle antibodies (ASMA) would confirm the latter diagnosis, while cirrhotic changes observed on ultrasound would suggest the former.
Elevated transaminase and presence of autoantibodiesDiagnosis will depend on the type of antibody found and the presence (or absence) of cholestasis. In the case of anicteric cholestasis with high alkaline phosphatase levels (>3N), the presence of AMAs and/or ANAs suggests primary biliary cirrhosis (PBC). Presence of AMA is the most common finding, however, cases of PBC, formerly known as autoimmune cholangitis, without AMA but with high titres of ANA have been reported.58–60 In the absence of cholestasis, a finding of ANA and/or high titres of ASMA is suggestive of AIH, particularly when accompanied by hypergammaglobulinaemia.61 In these cases, it is best to confirm the diagnosis with liver biopsy before starting immunosuppressant therapy.
Hypertransaminasaemia with decreased ceruloplasmin activityThis is highly suggestive of Wilson's disease. This diagnostic impression is strengthened if 24h urine copper output is greater than 100mcg. The test is only valid when urine output is measured over exactly 24h. The Leipzig score can be used to confirm a diagnosis of Wilson's disease.62 The most reliable non-invasive means of confirming the diagnosis is through genetic testing.63 If this is not available, or if results only show a single mutant allele, liver biopsy should be performed to quantify hepatic copper concentration.64
Hypertransaminasaemia with presence of anti-transglutaminase antibodiesThis is specific for coeliac disease, and rules out the need for duodenal biopsy. These antibodies are more specific than the gliadin and endomysial antibody tests previously used to diagnose this disease. The test can be used to detect coeliac disease in patients with no gastrointestinal symptoms.65,66 A gluten-free diet will usually normalise transaminase levels in the first year of follow-up in most patients.67 However, if high levels persist in a patient with suspected coeliac disease, other possible causes of hypertransaminasaemia, such as coeliac-related AIH, should be investigated.68
Hypertransaminasaemia as the sole laboratory findingThis finding is suggestive of either inflammatory (polymyositis) or congenital muscle disease, and diagnosis should be confirmed by determining serum CPK and aldolase. It is important to bear in mind that myotonic dystrophy type 1 (Steinert's disease) often presents with elevated levels of cholestatic enzymes associated with hypertransaminasaemia.48,49
What if the investigations performed do not give a definitive diagnosis?A series of tests (Table 5) are needed to determine the cause of asymptomatic persistent hypertransaminasaemia. If all these are negative, and the patient does not present any of the aforementioned findings, supplementary tests must be ordered, such as a thyroid panel (TSH and T4), and Addison's disease must be ruled out by means of an ionogram (hyponatraemia) and determination of serum cortisol. Nevertheless, adrenal insufficiency15,69 or hyper- and hypothyroidism rarely manifest as asymptomatic hypertransaminasaemia.14 Both conditions cause asthenia, and the patient could have been misdiagnosed with hepatitis.
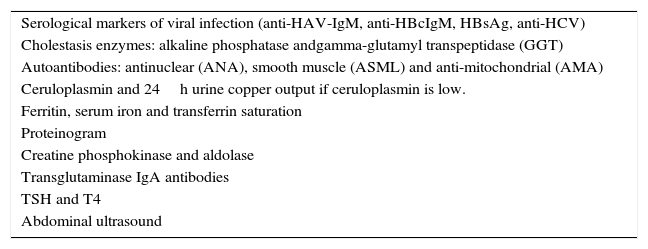
Diagnostic procedures in a patient with persistent asymptomatic hypertransaminasaemia.
| Serological markers of viral infection (anti-HAV-IgM, anti-HBcIgM, HBsAg, anti-HCV) |
| Cholestasis enzymes: alkaline phosphatase andgamma-glutamyl transpeptidase (GGT) |
| Autoantibodies: antinuclear (ANA), smooth muscle (ASML) and anti-mitochondrial (AMA) |
| Ceruloplasmin and 24h urine copper output if ceruloplasmin is low. |
| Ferritin, serum iron and transferrin saturation |
| Proteinogram |
| Creatine phosphokinase and aldolase |
| Transglutaminase IgA antibodies |
| TSH and T4 |
| Abdominal ultrasound |
If the foregoing diagnoses are ruled out, a liver biopsy should be considered. In some asymptomatic adults with normal liver function and mild hypertransaminasaemia, a liver biopsy will not reveal lesions that would explain the elevated enzyme levels. This occurred in 10% of cases in a series of 81 patients with negative liver function and serologic tests,70 in 6% of a series of 354 patients studied by Skelly et al.,71 and in 38% of a series of 88 liver biopsies studied by us, taken from patients in whom all known causes had been ruled out (unpublished findings).
In some cases of persistent hypertransaminasaemia, the liver biopsy will show subtle histological abnormalities, such as idiopathic ductopenia72 or idiopathic bile ductular hyperplasia73 that cause elevated transaminases. In other cases, nonspecific steatosis, inflammation or portal fibrosis are found, and sometimes more common diagnosable lesions are identified, such as granulomas, nodular regenerative hyperplasia,74 glycogenosis,75 diabetic hepatosclerosis76 or hepatic amyloidosis.77
Diagnostic process in a patient with persistent asymptomatic hypertransaminasaemiaStep 1 (first visit): history, physical examination and preliminary decisions- a)
Enquire whether the patient has experienced symptoms of infection immediately before or during the finding of elevated transaminases. If the symptoms have resolved, the blood panel should be repeated after 1 month. If the symptoms of infection persist, appropriate serologic tests and microbiological studies based on the patient's symptoms and epidemiology must be carried out to identify the infectious agent.
- b)
Elicit detailed information about the patient's consumption of medicinal drugs, herbal or dietary supplements (name of the products and when they were taken). If any of these substances might be implicated in transaminase elevation, the patient should be advised to stop using them, and the laboratory tests repeated after 4 weeks.
Suspicion of drug-related liver damage is based on exposure to the drug in question from between 3 months to 2 weeks prior to the positive transaminase finding. With some drugs, including amoxicillin and clavulanic acid, cases of hepatitis with an onset weeks after treatment is completed have been observed.78
Use of anabolic steroids is common among body-builders and people engaged in sports that require considerable muscle development, such as weight lifting. The liver and muscle toxicity of these drugs often causes elevated transaminase levels.79
- c)
Enquire whether the patient has engaged in strenuous physical activity in the days leading up to the test. If so, order CPK and aldolase panels. If the findings are pathological, transaminase elevation can be attributed to muscle damage. If not, a non-muscular aetiology must be found.
- d)
If the physical examination reveals the characteristic cutaneous stigmata of liver disease, the patient has advanced, though asymptomatic, hepatitis, and this will determine subsequent investigations. The first step is to determine whether the hepatitis is viral or alcohol-related.
- e)
In obese or overweight patients, the first diagnostic hypothesis will be fatty liver disease. The presence of the conditions associated with metabolic syndrome (Table 4) should be ascertained.
- f)
If none of the above apply, the tests and studies listed in Table 5 should be performed.
The physician will be able to make a definitive or presumptive diagnosis based on the pattern of findings observed in the results of the tests and studies performed (see above), and prescribe the most appropriate therapy.
The physician should seek answers to the following questions: Is it an chronic viral infection? Is it an autoimmune disease? Is it an iron or copper metabolism disorder? Are the symptoms consistent with fatty liver disease? Is it an alcoholic liver disease? Does the patient have an extrahepatic disease that could cause elevated transaminase levels?
If no definitive diagnosis can be reached, the patient should be re-interviewed to ensure he or she has not overlooked important information. Investigations should focus on identifying an uncommon cause of transaminase elevation, such as thyroid dysfunction, adrenal insufficiency, or Turner syndrome.57
One possible, albeit uncommon, cause of elevated transaminases is occupational toxic liver damage, as various industrial solvents, such as dimethylformamide80 or 1,1,1-trichloroethane81 can cause liver damage. Cotrim et al.82 described NAFLD changes of non-alcoholic steatohepatitis in workers in the petrochemical industry, and asymptomatic hypertransaminasaemia has recently been observed in a high proportion of cobblers, attributed to exposure to solvents,83 and also in workers exposed to hydrocarbons.84
In cases where the cause of the enzyme elevation has been identified, further diagnostic tests should be performed, such a liver elastography and HCV genotype determination in the case of viral infection, before recommending antiviral treatment, prescribing a diet and exercise regimen in patients with NAFLD, confirming coeliac disease before indicating a gluten-free diet, or referring the patient to an expert in muscle pathology to define the myopathy underlying the hypertransaminasaemia.
Step 3 (third visit): evaluate the impact of therapeutic decisions, consider more uncommon causes if no diagnosis is confirmed, and consider liver biopsyThis visit should be used to confirm the appropriateness of the strategy pursued if an aetiological diagnosis has been made and therapy has been recommended or further studies ordered.
If the patient has been treated, or if the offending medicinal product (drug, herbal supplement) or contact with the industrial toxin has been discontinued, tests should be repeated after 4 or 8 weeks to confirm normalisation or persistence of hypertransaminasaemia.
If no diagnosis has yet been reached, make sure that all the procedures recommended for ruling out the various causes of elevated transaminases (Table 5) have been carried out, and if they have, discuss with the patient the pros and cons of a liver biopsy. Liver biopsy can help clarify diagnostic uncertainties and identify the cause of the liver function abnormalities,85–87 although some cases will remain elusive. The procedure is not without its risks, although it is usually well tolerated.88
Conflicts of interestThe author declares that there are no conflicts of interest.
Please cite this article as: Bruguera M. Guía práctica para el examen del paciente adulto con hipertransaminasemia asintomática. Gastroenterol Hepatol. 2017;40:99–106.