Analgesics are widely used, but evidence regarding whether their use increases the risk of inflammatory bowel disease (IBD) flares or complications is unclear. Therefore, self-medication with analgesics in IBD is usually not recommended. The aim of this study was to explore the prevalence of self-medication with analgesics in a cohort of ulcerative colitis (UC) patients and to identify reasons and factors associated with self-medication.
MethodsThis cross-sectional study included consecutive unselected adult patients with UC. Participants were asked to complete an anonymous web-based survey with multiple-choice questions and closed responses. No clinical data were collected.
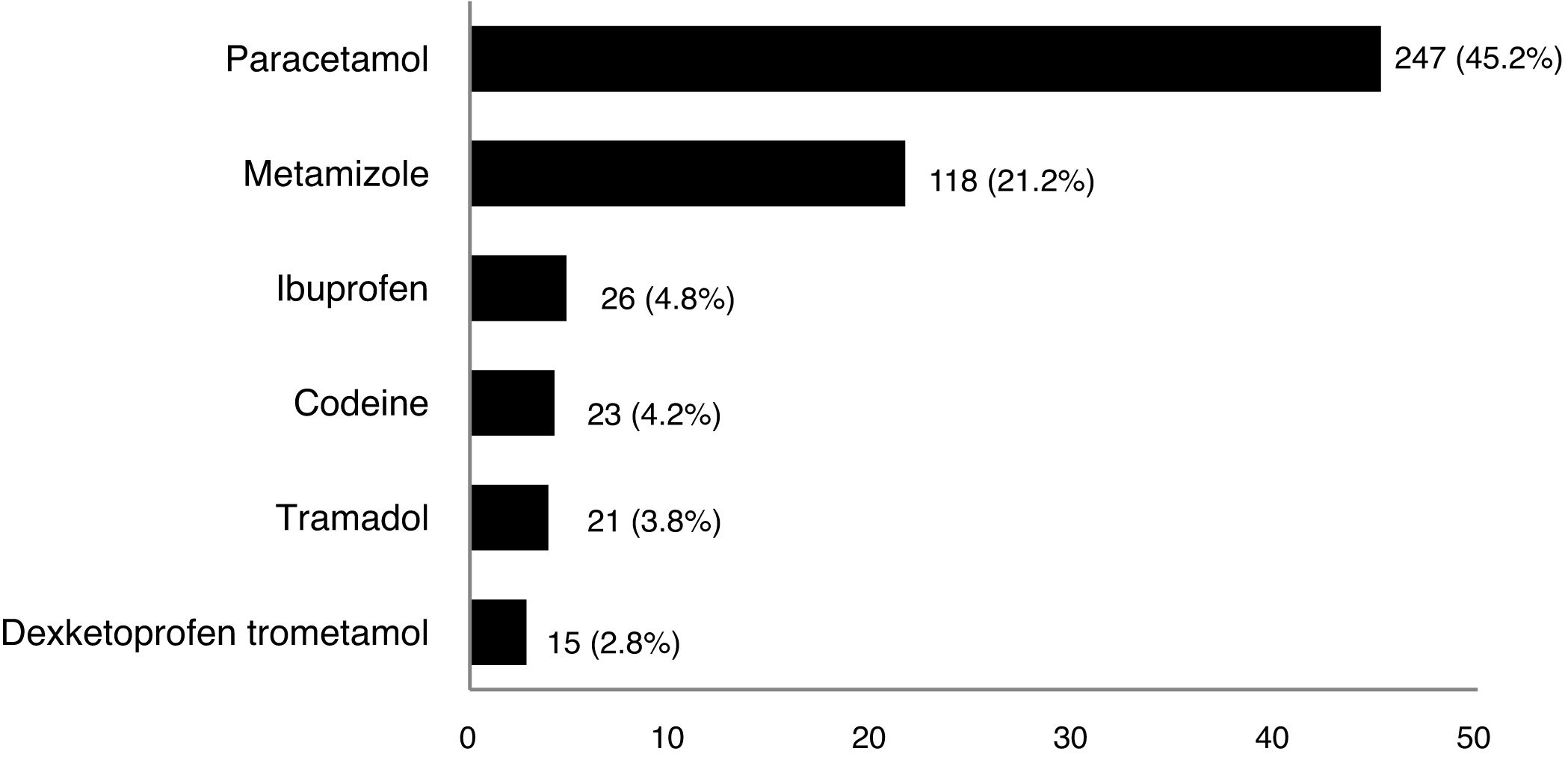
ResultsA total of 546 patients (61.2% women, mean age 39.9 years) completed the survey. The prevalence of self-medication with analgesics was 49.8% (272/546). Paracetamol (45.2%) and metamizole (21.2%) were the most frequently used drugs; frequencies of self-medication were <5% for other analgesics (nonsteroidal anti-inflammatory drugs, opioids). The most frequent reasons for self-medication were the need for quick symptom relief and that it had been agreed with/prescribed by the treating physician. Multivariable analysis identified female sex (odds ratio [OR]=1.9), sick leave (OR=2.2), treatment with intravenous drugs (OR=2.9), and emergency room visit (OR=2.3) as variables associated with self-medication, whilst follow-up by a nurse was associated with less self-medication (OR=0.6).
ConclusionThe frequency of self-medication with analgesics in UC patients is high and appears to be associated with variables suggesting worse disease control. Closer follow-up, including a specialized nurse, could decrease self-medication. Strategies to improve disease control, including close monitoring of symptoms such as pain, are needed.
Los analgésicos son medicamentos ampliamente utilizados, pero las evidencias sobre si su uso aumenta el riesgo de brotes o complicaciones de la enfermedad inflamatoria intestinal (EII) no están claras; por lo tanto, en general, no se recomienda la automedicación con analgésicos en la EII. El objetivo de este estudio fue explorar la prevalencia de automedicación con analgésicos en una cohorte de pacientes con colitis ulcerosa (CU) e identificar los motivos y los factores asociados a la automedicación.
MétodosEn este estudio transversal se incluyeron pacientes adultos con CU consecutivos y no seleccionados. Se pidió a los participantes que completasen una encuesta anónima por Internet con preguntas de elección múltiple y respuestas cerradas. No se recogieron datos clínicos.
ResultadosCompletaron la encuesta un total de 546 pacientes (61,2% mujeres; edad media 39,9 años). La prevalencia de automedicación con analgésicos fue del 49,8% (272/546). El paracetamol (45,2%) y metamizol (21,2%) fueron los fármacos utilizados con más frecuencia; la tasa de automedicación con otros analgésicos (antiinflamatorios no esteroideos, opioides) fue <5%. Los motivos más frecuentes para la automedicación fueron la necesidad de alivio sintomático rápido y que había sido acordado con/prescrito por el médico responsable del tratamiento. El análisis multivariante identificó el sexo femenino (odds ratio [OR]=1,9), la baja laboral (OR=2,2), el tratamiento con fármacos intravenosos (OR=2,9) y las visitas a urgencias (OR=2,3) como variables asociadas a la automedicación, mientras que el seguimiento por el personal de enfermería se asoció a menos automedicación (OR=0,6).
ConclusiónLa frecuencia de automedicación con analgésicos en pacientes con CU es alta y parece estar asociada a variables que sugieren peor control de la enfermedad. Un seguimiento más estrecho, incluyendo personal de enfermería especializado, podría disminuir la automedicación. Se necesitan estrategias para mejorar el control de la enfermedad, incluyendo un seguimiento estrecho de síntomas como el dolor.
Analgesics are among the most commonly used medications worldwide. Recent data from the Spanish population, including over-the-counter acquisition, revealed a prevalence of nonsteroidal anti-inflammatory drug (NSAID) consumption of nearly 30%, with a higher frequency in women and a step-down trend with age.1 Regarding other analgesics, paracetamol (27.4%) and metamizole (5.5%) are the most commonly used in the Spanish population.2
NSAID consumption, unlike paracetamol, is associated with upper and lower gastrointestinal tract damage,3,4 sometimes producing lesions that may resemble inflammatory bowel disease (IBD),5 and it is considered to be associated with an increased risk of IBD flares.6 Moreover, the prevalence of analgesics prescriptions seems higher in IBD patients than in the general population, including both narcotic (48.1% vs 34.1%) and non-narcotic analgesics (12.8% vs 8.1%),7 with a substantial additional percentage being self-medicated.8 Similarly-designed studies showed a 30–50% prevalence of NSAIDs use in IBD patients.9,10 A meta-analysis of 24 studies found no association between NSAID use and the risk of IBD flares.11 However, when analyzing only studies with a low risk of bias, NSAID use appeared to increase the risk of CD (relative risk [RR] 1.53, −95% CI 1.08–2.16), but not UC, flare. Contrary to expectations, paracetamol use was associated with an increased risk of IBD flares (RR 1.56, −95% CI 1.22–1.99).11 Based on this evidence, current IBD guidelines state that short-term use of NSAIDs is unlikely to be detrimental, and it should be used if considered necessary, although long-duration treatments are not recommended.12,13
With regard to opioid analgesics, a Canadian study reported 5% of IBD patients became heavy opioid users within 10 years of diagnosis.14 This is worrisome as opioid use is associated with high rates of serious infection and mortality,14,15 and IBD guidelines recommend that long-term opioid use should be discouraged.16
Finally, evidence regarding metamizole use and risks in IBD patients is scarce, as it has been withdrawn from many markets,17 but the frequency of use of this drug by IBD patients in marketed countries seems low (about 10%).18,19
To our knowledge, there are no data in Spain collected directly and anonymously from patients regarding self-medication with analgesics in UC patients. Thus, we designed a cross-sectional survey, with the aim of assessing the frequency of self-medication with corticosteroids (primary objective, information already published20) and with analgesics (secondary objective, subject of the current work) in a cohort of adult patients with UC, as well as to identify the factors associated with self-medication.
MethodsThis study was a cross-sectional, anonymous web-based survey of adult patients with UC. No data from clinical charts were collected. Patients were invited to participate by the Spanish Confederation of Associations of Patients with Crohn's Disease and Ulcerative Colitis (ACCU) and by their gastroenterology healthcare providers (either physicians or nurses) from the Spanish Working Group on Crohn's Disease and Ulcerative Colitis (GETECCU) and the Spanish Nurses Working Group on Inflammatory Bowel Disease (GETEII). Additional information on the design has been described previously.20 The study was approved by the Clinical Research Ethics Committee of the University Hospital Ramón y Cajal, Madrid, Spain. As the survey was voluntary and anonymous, completion of the survey was considered as implied patient consent to participate; this was approved by the Clinical Research Ethics Committee.
The survey was composed of multiple-choice questions with closed responses (no open-text questions were included) on patients’ demographics, patients’ perceptions of UC burden, characteristics of healthcare received and on self-medication. Subject recall for all survey questions was within the past year. To assess self-medication with analgesics, patients responded with “Yes” or “No” to the question “During the past year, have you started treatment with analgesics by your own initiative for treating the pain related to ulcerative colitis?”. A list of the most frequent therapies used for pain relief in Spain was provided.
Quantitative variables are expressed as mean and standard deviation (SD), or median and interquartile range (IQR) and qualitative variables as frequencies or percentages. Comparisons of the frequency of self-medication were performed using the χ2-test or Fisher exact test. A logistic regression model was developed to assess variables associated with self-medication; age, gender and variables with p values<0.05 in the bivariate analysis were included in the model. Odds Ratio (OR) and 95% confidence intervals (CI) are provided.
ResultsFrom February to April 2019, 546 patients completed the survey: 212 men (38.8%) and 334 women (61.2%), with a mean age of 39.9 years [SD 11.9] and a median duration of UC since diagnosis of 7 years. A total of 272 patients (49.8%) reported self-medication with analgesics during the past year by responding “yes” to the above-mentioned question. Self-medication was more frequent with paracetamol and metamizole (Fig. 1); frequencies were<5% for other analgesics including NSAIDs and opioid derivates.
Self-medication with analgesics was reported more frequently by women than men (56.0% vs 40.1%, p<0.001), and was less frequent in the upper quartile of age (49 years or more, Table 1). The frequency was similar in patients with UC duration above or below the median. The frequency did not differ significantly among patients with different educational degrees. Patients on sick leave reported a higher frequency of self-medication (75.5%) than those actively working (47.3%), unemployed (51.3%) housekeeping (56.3%) or than students (52.0%) (p=0.003).
Frequency of self-medication by different demographic and disease-related variables. Bivariate analysis.
| Frequency, n (%) | p | |
|---|---|---|
| Sex | ||
| Male (n=212) | 85 (40.1) | <0.001 |
| Female (n=334) | 187 (56.0) | |
| Age (quartiles) | ||
| Q1 (≤31 years; n=146) | 78 (53.4) | 0.053 |
| Q2 (32–39 years; n=130) | 71 (54.6) | |
| Q3 (40–48 years; n=145) | 74 (51.0) | |
| Q4 (≥49 years, n=125) | 49 (39.2) | |
| Perception of disease activity | ||
| Mostly inactive (n=125) | 49 (39.2) | <0.001 |
| Mild (n=188) | 85 (45.2) | |
| Moderate (n=170) | 97 (57.1) | |
| Severe (n=63) | 41 (65.1) | |
| Number of regular medical appointments per year for UC | ||
| Once a year (n=102) | 46 (45.1) | 0.021 |
| Two-three times per year (n=214) | 95 (44.4) | |
| Four or more times (n=211) | 123 (58.3) | |
| No regular scheduled medical appointments (n=18) | 8 (44.4) | |
| Needed telephone assistance | ||
| No (n=309) | 133 (43.0) | <0.001 |
| Yes (n=237) | 139 (58.6) | |
| Needed emergency room visit | ||
| No (n=417) | 184 (44.1) | <0.001 |
| Yes (n=129) | 88 (68.2) | |
| Needed hospital admission | ||
| No (n=490) | 238 (48.8) | 0.114 |
| Yes (n=56) | 34 (60.7) | |
| Access by e-mail or telephone contact | ||
| Yes (n=413) | 206 (49.9) | 0.009 |
| No (n=75) | 46 (61.3) | |
| Not known (n=58) | 20 (34.5) | |
| Access to specialized nurse | ||
| Yes (n=250) | 123 (49.2) | 0.010 |
| No (n=149) | 88 (59.1) | |
| Not known (n=147) | 61 (41.5) | |
With regard to patients’ perception of disease activity, the frequency of self-medication with analgesics ranged from 39.2% in patients who considered their UC as mostly inactive during the past year, to 65.1% in those who described it as severe (p<0.001). Patients who had needed urgent telephone assistance or at least one emergency room visit due to UC activity, reported a higher frequency of self-medication (Table 1).
The frequency of self-medication was similar in patients followed-up in a general gastroenterology clinic or in an IBD unit (47.1% and 50.7% respectively, p=0.815). Those with four or more medical appointments per year, who did not have the option to contact their gastroenterology healthcare providers via e-mail or telephone, or who did not have follow-up by a specialized nurse at the clinic, reported higher frequency of self-medication (Table 1). Some 77 of 117 patients (65.8%) who were being treated with intravenous biological medications compared with 170 of 429 (39.6%) of those who were not (p<0.001) declared self-medication with analgesics. There were no differences with in self-medication in those being treated with subcutaneous biological drugs (50.9% versus 49.8% in those not treated with subcutaneous biologicals, p=0.976).
The most common reasons for self-medication were “the need for quick relief of symptoms” and “it had been agreed with or prescribed in the past by the treating physician” (Table 2).
Reasons for self-medication with analgesics.a
| Which were the reasons for initiating analgesics by your own initiative for treating the pain related with your ulcerative colitis? | n (%) |
|---|---|
| The need for quick relief of symptoms | 173 (63.6) |
| It had been agreed with my physicianb | 96 (35.3) |
| My doctor had prescribed analgesics in the past | 83 (30.5) |
| Difficulty obtaining an early appointment with my physician | 40 (14.7) |
| Fear that symptoms could worsen | 38 (13.9) |
| It is what I am used to doing, I do not need to ask my physician | 27 (9.9) |
| Being on vacation | 14 (5.1) |
| Lack of time to attend the clinic | 13 (4.7) |
| I read it on the Internet | 1 (0.4) |
The multivariable model included, as independent variables, age, gender, employment status, number of regular UC-related medical appointments per year, disease activity, need of telephone assistance, emergency room visit, access by e-mail or telephone contact, access to specialized nurse and treatment with intravenous biological therapies. Female sex (OR=1.9 [95% CI: 1.3–2.8], p<0.001), sick leave (OR=2.2 [1.1–4.6], p=0.031), treatment with intravenous drugs (OR=2.9 [1.8–4.6], p<0.001), and emergency room visit (OR=2.3 [1.5–3.6], p<0.001), were variables positively associated with self-medication with analgesics, whilst access to a specialized nurse vs no access was associated with less self-medication (OR=0.6 [0.4–0.9], p=0.022).
DiscussionThis study reaffirms the fact that, although guidelines do not recommend self-medication with analgesics in IBD patients, the use of these drugs without indication by the treating physician for treating UC-related pain is frequent in this population. In this anonymous survey, about half the patients declared that they had self-medicated with analgesics in the past year due to pain that they considered to be related to UC. The finding is worrisome for two reasons: (1) the potential for analgesics to partially mask UC flares, which can complicate the disease course and lead to complications, and (2) the use of drugs with relatively common adverse effects, or even some (e.g. several NSAIDs) could be contraindicated in some patients.
Paracetamol was the most common analgesic with which our cohort declared to have self-medicated (45.2%), consistent with the findings from other studies.8,18 Metamizole was the second most common drug (21.2%), probably related to its wide use in the Spanish population,2,22 and its better gastrointestinal toxicity profile compared with NSAIDs.23 Of note, although self-medication with drugs which possess the potential for more serious adverse events (opioid derivatives and NSAIDs) was much less frequent in our cohort, efforts are still needed to reduce self-medication with these analgesics.
As observed in the general Spanish population, the use of analgesics in our cohort was higher in women and in younger patients.1 Female sex was one of the factors associated with higher analgesic self-medication after multivariable analysis, in line with findings from other studies in IBD patients.19,21 This finding may be partially related to the higher prevalence of extra-intestinal manifestations, such as peripheral arthropathies and arthralgia, in women.12 However, we did not collect clinical data and cannot confirm this potential association.
Other variables associated with self-medication with analgesics (sick leave, emergency room visit, treatment with intravenous drugs) appear to be related to worse control or more severe UC course, suggesting that minimizing disease activity would lead to a lower requirement for analgesics. We should emphasize the importance of follow-up by a specialized nurse as one factor associated with less self-medication in this study. The availability of an IBD nurse is associated with a reduction in hospital admissions, and emergency unit and outpatient clinic visits,23 and is cost-effective for the management of IBD patients24; consequently, it is recommended in current guidelines.16
However, it should be noted that self-medication with analgesics in our cohort was high even in patients who considered their disease to be inactive (39.2%). This fact has also been reported in other studies,8,21 suggesting that analgesic consumption may be a marker of mild symptomatic disease that is not in complete remission, or that patients have normalized the presence of certain symptoms in their everyday life. Further investigation is needed to ascertain whether patients with presumable quiescent IBD and analgesic consumption definitely have no underlying active disease, or if pain is related to co-existing diseases.25 Nonetheless, this high prevalence of analgesic consumption highlights the burden of pain for UC patients, impacting their quality of life and their social and working habits.18,19
With regard to the reasons for self-medication, the main reason reported by patients in this survey was the need for quick symptom relief, but the percentage who declared that it had been agreed with or prescribed by their treating physician in the past was also significant. In these cases, better patient-physician communication is warranted; this has been highlighted by patients in a recent evaluation of quality of care standards,26 and they should inform physicians to avoid misbehaviors with regard to the intake of analgesics.
The main limitations of the study include the cross-sectional design with no follow-up and the survey format with no clinical data collection, which precludes the establishment of strong conclusions between self-medication and specific UC characteristics or outcomes. Moreover, the study is based exclusively on the statements of the sample of patients who voluntarily agreed to answer the survey. Therefore, the sample is selected, and may not reflect the habits of all patients. Although the frequency of self-medication with NSAIDs was ∼5% in our survey, patients tend to underestimate their NSAID use27; consequently, if NSAID use had been sought objectively, the actual frequency in our study may have been higher than reported. Nevertheless, the study provides relevant information on variables and reasons for self-medication which can help in establishing preventive and corrective measures. The inclusion of a large number of patients, and the anonymous nature of the survey, avoiding potential bias related to the presence of the treating physician, gives strength to the study results.
ConclusionThe frequency of self-medication with analgesics due to UC-related pain is high and appears to be related to variables suggesting persistent symptoms or worse disease control. As a striking finding, those who described their disease as mostly inactive also described a high frequency of self-medication, suggesting that these patients could not be truly in remission and might be normalizing the presence of pain. Efforts to achieve better close monitoring and lower pain perception in this population are needed. In this regard, the survey also suggests a benefit from multidisciplinary teams with nurse follow-up for patients with UC.
Sources of funding/supportThe study was funded by MSD Spain.
Conflicts of interestIago Rodríguez-Lago: board membership (Tillots Pharma, Pfizer, Ferring, Adacyte), payment for lectures including service on speakers’ bureaus (Tillots Pharma, Pfizer, MSD, AbbVie, Takeda, Dr. Falk Pharma, Ferring, Adacyte, and Roche).
Francisco Mesonero: payment from MSD Spain for the development of educational presentations, research funding from MSD, AbbVie, Takeda, Janssen, Ferring, Kern-Pharma, and Dr. Falk Pharma.
Gonzalo Hijos-Mallada: the author declares no conflicts of interest.
Mercedes Cañas: payment for consultancy from MSD Spain.
Roberto Saldaña: the author declares no conflicts of interest.
Claudia Savini: the author declares no conflicts of interest.
Sabela Fernández: full-time employee, Medical Affairs, MSD Spain.
Berta Juliá: full-time employee, Medical Affairs, MSD Spain.
Luis Cea-Calvo: full-time employee, Medical Affairs, MSD Spain.
The current study was funded by MSD Spain, a subsidiary of Merck & Co. Inc, Kenilworth, New Jersey, USA, and was endorsed by the Spanish Confederation of Associations of Patients with Crohn's Disease and Ulcerative Colitis (ACCU), the Spanish Working Group on Crohn's Disease and Ulcerative Colitis (GETECCU) and the Spanish Nurses Working Group on Inflammatory Bowel Disease (GETEII). The authors thank David P. Figgitt PhD, ISMPP CMPP™, Content Ed Net, for providing editorial support, with funding from MSD Spain.