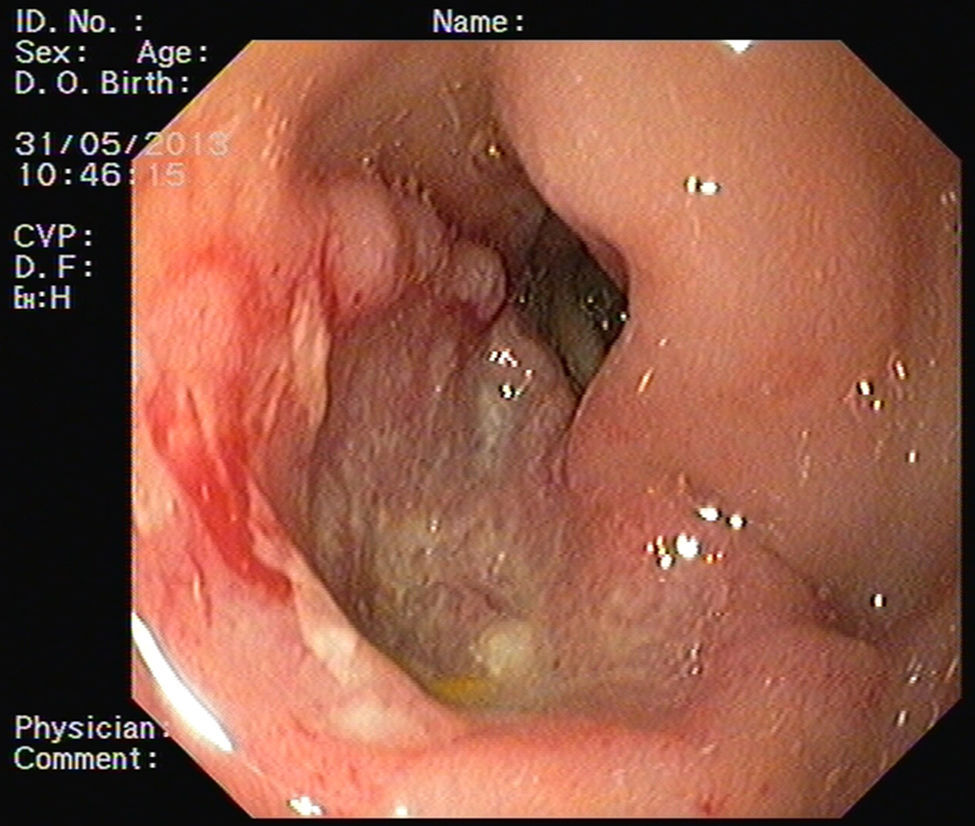
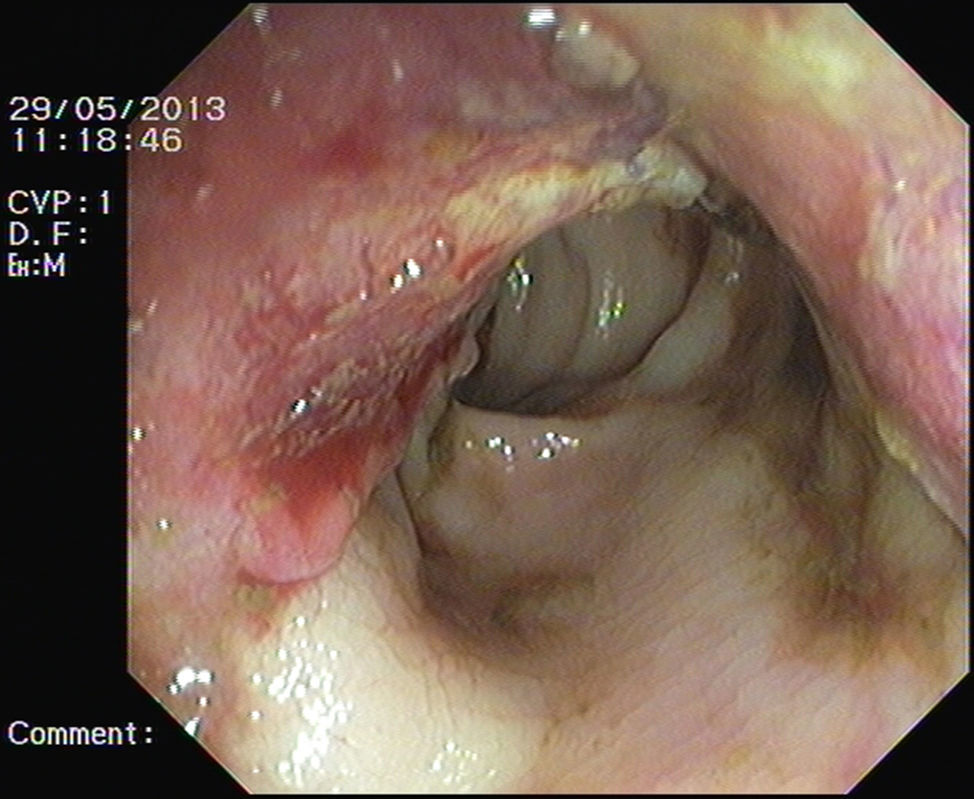
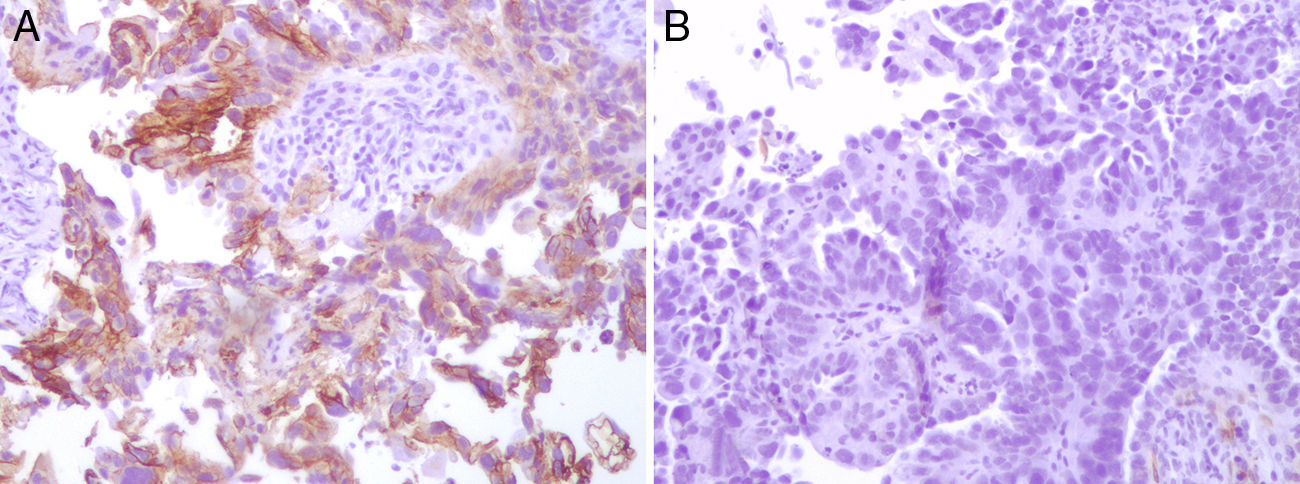
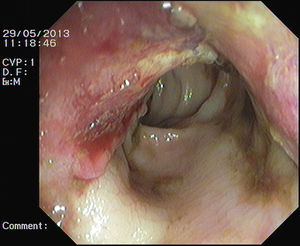
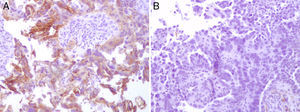
A 75-year-old female presented with asthenia and melena. Her past medical history included Alzheimer's disease, laparotomy in childhood due to unknown reason and an advanced ovarian neoplasm with peritoneal carcinomatosis in palliative treatment during the last year. Two years before, the patient was submitted to gastrointestinal endoscopic examination (endoscopy and colonoscopy) that were normal. She was pale and her vital signs were stable. The abdomen was distended and asymmetric, with an abdominal surgical scar in midline and multiple visible and palpable masses in all quadrants (Fig. 1). Laboratory tests showed hemoglobin of 8.3g/dL. Endoscopy demonstrated an excavated ulcer with elevated irregular borders, in the antero-inferior wall of duodenal first portion with no major bleeding stigmata (Fig. 2) and endoscopic biopsies were performed. Blood transfusion and medical treatment were started and clinical improvement was observed. However, on the third day after admission she had haematochezia. A colonoscopy was performed and showed two ulcerated masses in the sigmoid colon with active bleeding (Fig. 3). Endoscopic hemostasis with argon plasma coagulation was attempted without success. Biopsies were done. Histopathological examination confirmed metastatic malignant ovarian neoplasm in duodenum and colon (Fig. 4).
Duodenal and colonic metastases are a very rare cause of gastrointestinal bleeding.1,2 However, they should be considered in a patient presenting with gastrointestinal bleeding and a previous history of malignancy.1 The main dissemination pattern in epithelial ovarian neoplasm is the transcoelomic route. Metastasis to the intestinal mucosa can occur as a result of transmural involvement by invasion from the serosal surface. Lymphatic and hematogenous dissemination may also occur in the case of advanced peritoneal disease.1 Symptoms are nonspecific and similar to those caused by other gastrointestinal tumors: abdominal pain, altered bowel habits, tenesmus, small bowel obstruction or perforation, hematemesis, melena and anemia. Imaging and endoscopic findings are unspecific and histopathological examination allowed definitive diagnosis. Special immunohistochemical staining, including cytokeratin-7 and 20, Ber-EP4 and the anti-calretinin antibody, is important to confirm diagnosis.1,3–5 Prognosis is poor and treatment is mainly palliative. Endoscopic treatment is hardly effective. In some cases surgical resection and chemotherapy may be considered.2
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.