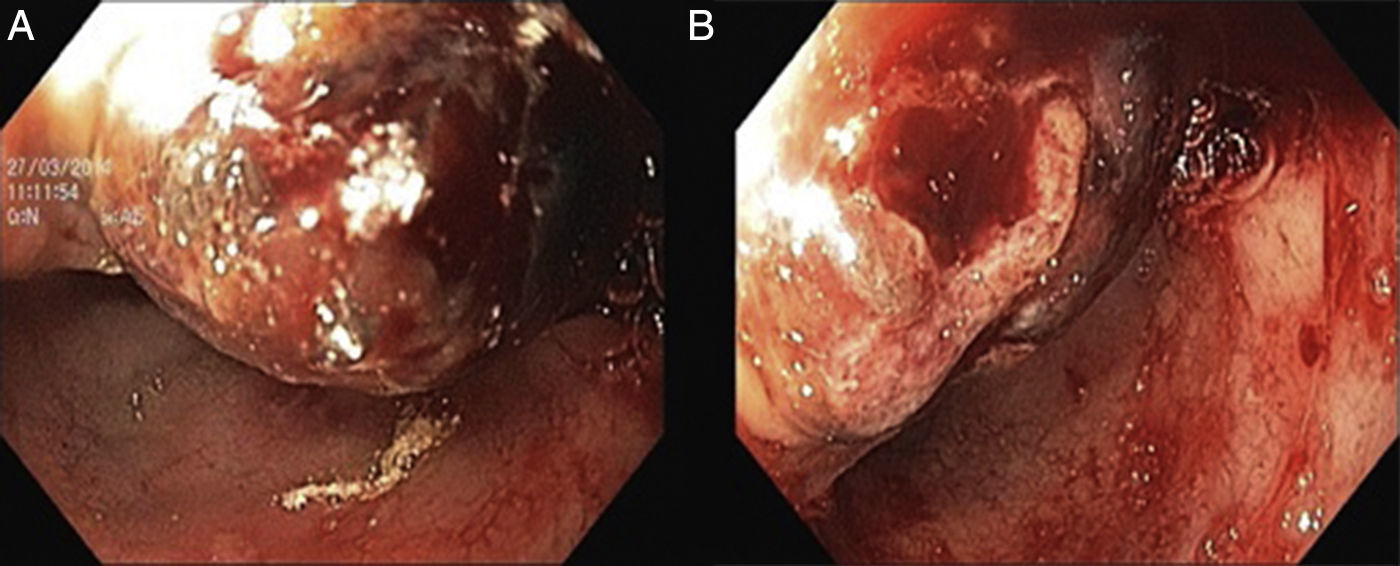
The authors describe a 63 year old male patient with a previous diagnosis of hereditary hemochromatosis (HH) performed an abdominal computed tomography (CT) that confirmed 2 liver masses compatible with hepatocellular carcinoma (HCC). He was proposed to chemoembolization treatment however he refused it. He presented in Emergency Department, nine months after, with melenic stool and epigastric pain, the laboratory work-up revealed hemoglobin 6.5g/dL with MCV of 72.3fl. Esophagogastroduodenoscopy was performed and revealed in the anterior and superior bulb wall, protruding into the duodenal lumen, a dark reddish polypoid lesion with 30mm of maximum diameter that occluded half of the lumen (Fig. 1).
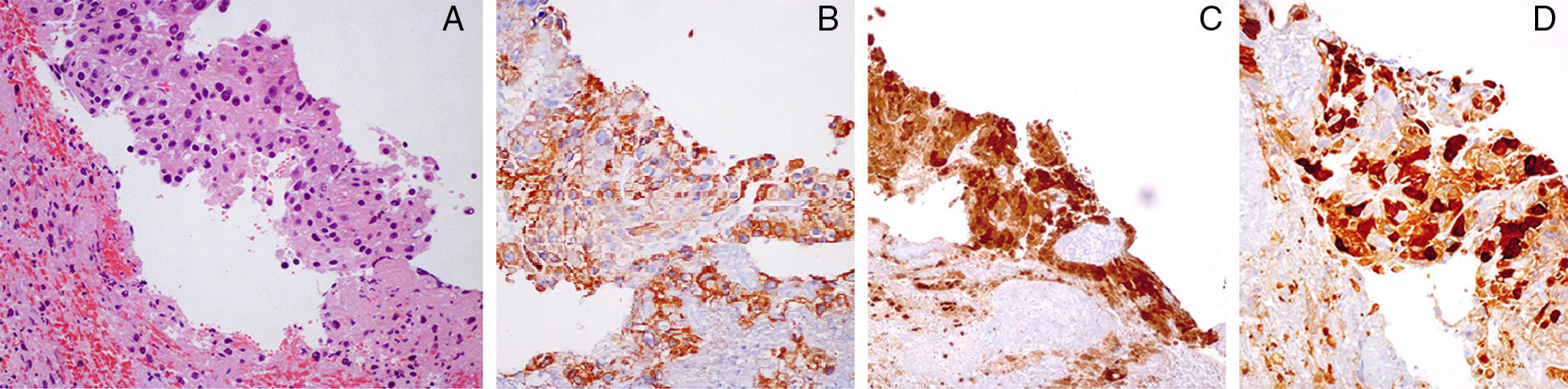
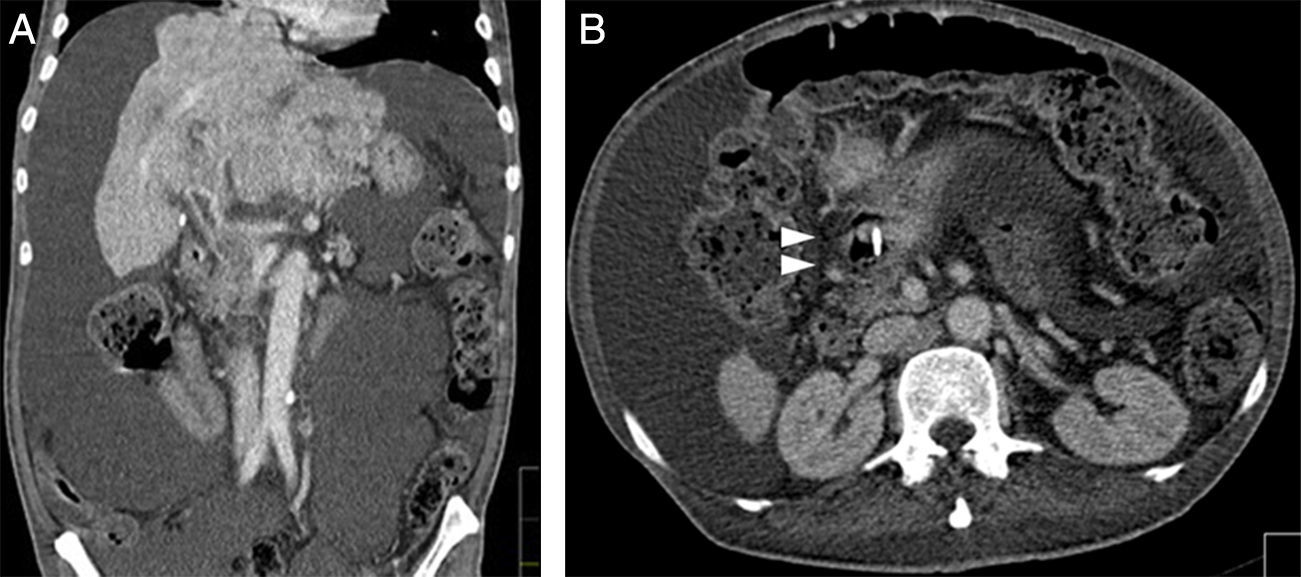
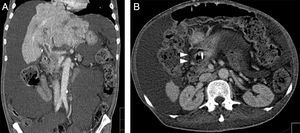
Biopsies were taken as it was not actively bleeding at the time of endoscopy. Histological analysis showed a fibrin clot with hepatic phenotype cells in the peripheral area. These cells showed cytological atypia and were disaggregated (Fig. 2A). Immunohistochemical studies revealed positive tumor cells staining for Heppar-1 (Fig. 2B), HSP-70 (Fig. 2C) and glutamine synthetize (Fig. 2D). Immunostaining showed negative results for CDX-2 and glipican-3, confirming the diagnosis of locally advanced HCC. Abdominopelvic CT was performed and showed multiple liver masses located in the left hepatic lobe, with the confluent lesions measuring 19.9cm of maximum diameter, some of them occupied the right lobe (Fig. 3A). It was also possible to recognize evidence of local invasion of the first part of the duodenum (Fig. 3B). Supportive treatment was given and the patient died of hepatic coma three weeks after the episode of gastrointestinal bleeding.
The authors describe a case of a duodenal invasion due to an HCC with upper digestive hemorrhage. In fact, the upper gastrointestinal bleeding is one of the most common complications in patients with HCC. Common etiologies include peptic ulcer disease, variceal bleeding due to portal hypertension from underlying cirrhosis, tumor invasion of portal vein causing thrombosis and portal hypertensive gastropathy.1–4 The direct invasion of tumor to gut is considered a rare cause among patients with a non-variceal source of upper digestive hemorrhage with an estimated incidence of 0.05–2%.5–7 The authors describe a 63 year-old male patient with a diagnosis of HCC who presented with melenic stool and epigastric pain. Esophagogastroduodenoscopy revealed in the anterior and superior bulb wall, a dark reddish polypoid lesion with 30mm that occluded half of the lumen. Histological analysis confirmed the diagnosis of HCC with locally advanced disease.
Metastatic spread of HCC can be hematogenous, lymphatic or by direct invasion of the tumor into adjacent organs.4 In our case the abdominopelvic CT performed showed local invasion of the first part of the duodenum (Fig. 3B and C) making the direct tumor invasion of the gastrointestinal tract the most likely process. In conclusion, despite being a rare situation, gastrointestinal bleeding in advanced HCC should raise suspicions of duodenal involvement.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.