Background/Objective: Several diagnostic criteria of Post-traumatic Stress Disorder (PTSD) are remarkably similar to symptoms reported by individuals with depression, particularly as they manifest as cognitive processing deficits in children. Because of this overlap in profile and the high rate of comorbidity of PTSD and depression (48% to 69%), pinpointing similarities/differences in cognitive processes related to each of these disorders is essential to accurate diagnosis. This study aims to examine cognitive performance profiles of 23 children who have been victims of PTSD and to compare their results with 23 children with depression and 24 controls. Method: Empirical study, observational and descriptive methodologies were performed using several neuropsychological tests to assess IQ, attention, memory and executive function. Statistical comparisons between groups were made using the non-parametric Kruskall-Wallis test and post-hoc analyses were conducted using a Mann Whitney U test, as well as Quade's co-variance analysis. Results: Data show different profiles of cognitive performance in those with PTSD compared to those with depression and controls. Conclusions: The findings suggests that PTSD and depressed children differ somewhat in their cognitive profiles, and the differences in IQ found between those with PTSD and those without are not necessarily a confounding variable, but may rather be a consequence of their traumatic experience.
Antecedentes/Objetivo: Varios criterios diagnósticos del trastorno de estrés post-traumático (PTSD, por sus siglas en inglés) son similares a los síntomas de la depresión, particularmente relacionados con aspectos cognitivos de niños afectados por estas condiciones. Debido a esta superposición del perfil cognitivo y dada la alta comorbilidad entre PTSD y depresión (48% y 69%), identificar las características en los perfiles cognitivos de cada trastorno pudiera ser útil para hacer diagnósticos más precisos. El objetivo fue examinar el rendimiento cognitivo en 23 niños con PTSD y comparar sus resultados con 23 niños con depresión y 24 controles. Método: Estudio empírico, observacional y descriptivo mediante aplicación de una batería neuropsicológica que evaluó inteligencia, atención, memoria y función ejecutiva. Las comparaciones estadísticas se realizaron mediante la prueba no paramétrica Kruskal-Wallis. Los análisis post-hoc se realizaron utilizando U de Mann Whitney y el análisis de covarianza de Quade. Resultados: Los datos muestran diferentes perfiles cognitivos del grupo con PTSD en comparación con los grupos de depresión y controles. Conclusiones: Los hallazgos sugieren que el grupo de PTSD y el grupo de depresión difieren en sus perfiles cognitivos y que las diferencias en el nivel intelectual encontradas en los niños con PTSD pudieran no ser una variable de confusión sino una consecuencia de la experiencia traumática.
The latest version of the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013) includes a new type of trauma and stress related disorder, namely Post Traumatic Stress Disorder (PTSD). The latter is a specific classification derived from traumatic experiences in which four distinct factors converge: 1) re-experiencing of the trauma, 2) effortful avoidance of trauma reminders, 3) negative alteration in mood and cognition and 4) alterations in arousal and reactivity (Danzi & La-Greca, 2016; Van Dusen, Tiamiyu, Kashdan, & Elhai, 2015). While PTSD is a common diagnosis associated with trauma, in the clinical context, some similar symptoms typically associated with depression are increasingly being reported following traumatic experiences, particularly in children and adolescents (Calderón-Delgado & Barrera-Valencia, 2013; Itzhaky, Levin, Fingerhut, & Solomon, 2014; Thabet, Thabet, & Vostanis, 2016). In fact, PTSD and depression are frequently comorbid with 48%-69% of individuals diagnosed with PTSD also showing clinical evidence of depression (Elhai, Grubaugh, Kashdan, & Frueh, 2008).
The rates of early traumatic experiences related to maltreatment, abuse and neglect against children and adolescents are increasing worldwide. For example, in the United States during 2014 about 6.6 million children were reported to have experienced some form of maltreatment with 1,580 of them dying from abuse and neglect (U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, & Children's Bureau, 2016). In Colombia, during the same year 10,402 children and adolescents were victims of intra-familial violence along with 15,807 reported cases of rape and sexual abuse. Tragically 1,064 individuals died from these situations of violence and abuse. Perhaps more alarmingly 2,931 children and adolescents have simply disappeared as a result of armed conflicts in Colombia (Instituto Nacional de Medicina Legal y Ciencias Forenses, 2015). These large numbers highlight the importance of gaining a deeper understanding of the consequences of early traumatic experiences on several aspects of brain development and potential changes in cognitive functioning.
Child maltreatment is known to have a significant negative impact on the developing nervous system, which in turn interferes with the achievement of numerous developmental/cognitive milestones (Davis, Moss, & Nogin, 2015) as well as increasing the incidence of some somatic diseases related to PTSD (Britvić et al., 2015). Some of the cognitive deficits are related to under-development of the prefrontal cortex (and thus executive functions) which does not fully reach maturity until early adulthood, and is particularly sensitive to maltreatment and abuse during the early years (Holmes, Kim-Spoon, & Deater-Deckard, 2016). In light of this fact, a better understanding of the association between early traumatic experiences and cognition would contribute greatly to the accurate diagnosis of PTSD and depression.
One major complication to the process of diagnosing these conditions is the fact that children with depression often exhibit a similar alteration of their cognitive performance profiles as those with PTSD. For example, previous studies have suggested that children with PTSD have lower intelligence quotient (IQ) scores, deficits in verbal memory, attention, and learning, as well as impairments in a variety of higher-order executive functions, for example difficulties in pre-planning purposeful action and lower inhibitory control (De Bellis, Hooper, & Spratt, 2009; Fry, Langley, & Shelton, 2016). Similarly, children diagnosed with major depression also show alterations/deficits in several of these same cognitive domains. In that regard, Wagner, Müller, Helmreich, and Huss (2015) conducted a meta-analysis of 17 studies with samples of depressed participants 4 to 18 years old and found deficits in verbal memory, sustained attention, phonemic verbal fluency and inhibitory capacity–a profile very similar to that reported for those with PTSD (see Barrera, Calderón, & Bell, 2013). Because of this apparent overlap in cognitive profile and the high rate of comorbidity between PTSD and depression (48% to 69%) (Flory & Yehuda, 2015), pinpointing similarities/differences in cognitive processes induced by each disorder is essential to understanding the relationships among traumatic experience, cognition and emotion, with the latter knowledge contributing to more accurate diagnoses.
Since IQ represents a global cognitive skill, which has a strong impact on the daily life of children and adolescents, there is particular interest in describing the connection between IQ and psychopathology, thus improving our understanding of the relationship between cognition and mental disorders. Unfortunately, the relations among PTSD, depression and low IQ as reported in the current literature are often conflicting or ambiguous. For example, regarding the connection between depression and IQ, Koenen et al. (2009) assessed 1,037 males and females (New Zealand) who were followed-up to age 32. WISC-R IQ was assessed at ages 7, 9, and 11. Diagnoses of DSM mental disorders were subsequently made at ages 18, 21, 26, and 32. Their results showed a relation between lower childhood IQ and depression in adulthood. And a similar result was reported by Zammit et al. (2004), who found lower IQ was reliably related to severe depression. Moreover, Morsy and Rothstein (2015), found a link between depression and lower IQ, but only for those with accompanying (and significant) social disadvantages.
Similar to the relationship between IQ and depression, the association between PTSD and IQ also remains unclear. Saltzman, Weems and Carrion (2006), in a sample of 59 adolescents, reported a correlation between PTSD symptoms and IQ, particularly verbal IQ, with greater symptom severity predictive of lower IQ scores. De Bellis et al. (2009), also reported lower IQ in a PTSD group compared to a control group, but as pointed out by the authors, there was no clear understanding if lower IQ was a predisposing factor or a consequence of their traumatic experiences.
Note that previous studies investigating the above relationships have often been confounded by pharmacological interventions, as well as an overly broad age range of study participants (Fry et al., 2016; Itzhaky et al., 2014) and these factors make it difficult to determine the relative impact of PTSD and depression on cognitive functioning. Furthermore, the routine use of different batteries of neuropsychological tests to evaluate each of the disorders has contributed to the difficulty in comparing the specific impact of PTSD versus depression on various cognitive processes. Thus, the present study includes samples of traumatized, depressed, and control Colombian children/adolescents (all within the same age range and using an identical assessment test battery) aiming to identify potential similarities/differences across cognitive profiles of participants diagnosed with PTSD and participants reporting depression.
MethodAn empirical study with descriptive and quantitative methodologies was performed (Montero & León, 2002) using several neuropsychological instruments to assess the cognitive profiles of performance in PTSD, depressed and control participants.
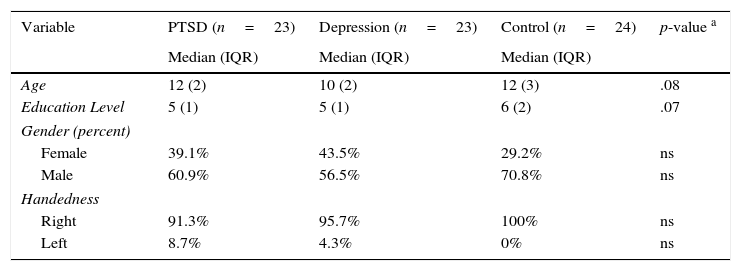
Participants and ProceduresThe study involved 70 children and adolescents recruited primarily from a semi-rural community in Colombia, South America. The distribution by gender was 37.1% for girls and 62.9% for boys; participants had a median age of 11 (interquartile range=3) and 5 years of schooling (interquartile range=2). From this sample 23 participants exhibited symptomatology associated with PTSD, while 23 participants had no history of trauma. However, a screening using the Children's Depression Inventory (CDI) and the Mini-International Neuropsychiatric Interview for Kids (MINI Kids) revealed some clinical depression symptomatology. Finally, for the control group, 24 participants without a history of trauma or neurological/psychiatric diagnoses were recruited. The groups were matched on age and education level (see Table 1).
Demographic characteristics.
| Variable | PTSD (n=23) | Depression (n=23) | Control (n=24) | p-value a |
|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | ||
| Age | 12 (2) | 10 (2) | 12 (3) | .08 |
| Education Level | 5 (1) | 5 (1) | 6 (2) | .07 |
| Gender (percent) | ||||
| Female | 39.1% | 43.5% | 29.2% | ns |
| Male | 60.9% | 56.5% | 70.8% | ns |
| Handedness | ||||
| Right | 91.3% | 95.7% | 100% | ns |
| Left | 8.7% | 4.3% | 0% | ns |
Note. IQR: interquartile range.
The PTSD sample was obtained from the Psychosocial Intervention Program for Socio-political Violence Victims and their Families, a non-governmental organization initiative in a semi-rural area west of Antioquia, Colombia (Antioquia is the Colombian state that includes the city of Medellin). Children and adolescents who had experienced trauma were evaluated using the MINI Kids to confirm the symptomatology associated with their PTSD. In addition to physical maltreatment, a common cause of PTSD in children, this sample included children who had lived in situations/conditions commonly associated with refugees (or displaced persons) and/or had experienced the death of one or both parents as a result of para-military or armed guerrilla conflict. Children and adolescents with PTSD symptomatology were interviewed to explore detailed aspects of their traumatic experiences. All participants met the following criteria: 1) they had personally experienced, witnessed, or been confronted by an event(s) involving actual or threatened death or serious injury, 2) their response to the situation involved intense fear, helplessness, horror, disorganized or agitated behavior, and 3) they exhibited at least one symptom associated with the re-experiencing of the traumatic event.
Depression and control group participants were recruited from local public schools via authorization of the school system's chief administrator. The CDI was used to assess 437 children and adolescents during a classroom session lasting about 25minutes, resulting in 51 participants selected for the study: 25 with clinical-level depressive symptoms and 26 without any depressive symptomatology. All participants were interviewed by a clinical psychologist, who extracted a complete written history of any learning difficulties or psychiatric/neurological conditions. For the depression group the MINI Kids was used to confirm the symptomatology associated with their depression, and for the control group it was used to rule out any diagnosis of PTSD, depression, or any other mental health problems. Two of the depressed individuals were excluded from the study due to comorbid symptomatology associated with PTSD and attention deficit hyperactivity disorder (ADHD), and 2 of the 26 controls elected not to participate for personal reasons. Thus, 47 participants in total comprised the final sample of the depression (23) and control (24) groups. The study was carried out according to the latest version of the Declaration of Helsinki, and the Ethics Committee of University of Antioquia gave its approval for the study. Based on the protocol of the Institutional Human Subjects Review Board of the University of Antioquia, all 70 participants signed an assent form and their parents/guardians signed consent forms. Each individual underwent neuropsychological testing during a 90-minute session with a clinical psychologist and neuropsychologist who interviewed the participants individually.
MaterialsMini-International Neuropsychiatric Interview for Kids (MINI Kids; see Sheehan et al., 1998). This is a structured diagnostic interview that provides for the reliable diagnosis of DSM-IV-TR psychiatric disorders. In the present study a validated Spanish translation of this instrument was employed (Ferrando, Bobes, Gibert, Soto, & Soto, 2000). Performance on the MINI Kids was used to exclude children or adolescents with comorbid cognitive/psychiatric problems (e.g., ADHD, substance abuse, anxiety and developmental disorders).
Children's Depression Inventory (CDI). A validated Spanish translation (Figueras-Masip, Amador-Campos, Gómez-Benito, & del Barrio-Gándara, 2010) of this test was used to evaluate depressive symptomatology in participants. The test consists of a 27-item, self-rated, symptom-oriented scale suitable for assessment of youth aged 7 to 17. The CDI includes five scales (negative mood, interpersonal problems, ineffectiveness, anhedonia and negative self-esteem) as well as a total scale score. Following the recommendation of Kovacs (1992), a cutoff score of 19 for severe depression was set to identify depressed participants.
Neuropsychological testing: Neuropsychological assessment was conducted using subtests from the Child Neuropsychological Assessment battery (Matute, Rosselli, Ardila, & Ostrosky-Solís, 2007) to evaluate attentional and memory processes. This battery has been validated for use in the aforementioned Colombian population, and is broadly used by clinicians and researchers alike. From this battery four subtests were used.
Visual attention. This test assesses sustained visual attention and includes two cancellation tasks. First—drawing cancellation— where the child is asked to cross out the larger rabbit on a sheet of rabbits of two different sizes. He/she completes as many as possible in 1min. The second test is a 1min letter cancellation task that requires the child to cross out the letter X but only if it is preceded by an A in a set of six different letters. The Cronbach's alpha for this subtest is .83.
Auditory attention. The test assesses auditory attention, via a digits forward and a digits backward task. In this test the examiner verbally presents digits at a rate of 1/sec. The forward test requires the participant to repeat the digits verbatim. The backward test requires the participant to repeat the digits in reverse order. The number of digits increases by one until the participant fails on two consecutive trials of the same digit span. The Cronbach's alpha for this test is .79.
Word memory: This task consists of a list of 12 words from 3 categories (animals, fruits, body parts). The whole list is read 4 times, testing recall after each reading. Then, 20minutes later, a delayed recall test is conducted. Next, cues (categories) are given, and finally a more extensive list with additional words is given and the participants are asked to recognize which of the words were on the original list. The Cronbach's alpha for this test is .88.
Narrative memory: This subtest assesses story recall skill. Participants listen to a story with 15 main ideas and then are asked to provide as many of the ideas conveyed as possible. Twenty minutes later, the idea recall portion of the task is repeated.
Stroop Test: This test is made up of three parts: the first one, contained the words ‘RED’, ‘GREEN’, ‘BLUE,’ and ‘YELLOW’ printed in black; the second part contained groups of X's (XXXX) printed in red, green, blue, or yellow; and finally, for the incongruent conditions, the color name word was printed in an incongruent color (e.g., the word “green” printed in red). In this test, the participant is required to name aloud the color of the ink in which the stimulus item is presented and is thus designed to measure cognitive flexibility and response inhibition (Lezak, Howieson, Bigler, & Tranel, 2012).
Wisconsin Card Sorting Test (WCST). This test was conducted in order to assess abstract reasoning and cognitive flexibility (Axelrod, 2002), using the procedure outlined by Heaton, Chelune, Talley, Kay, and Curtis (2001). The participants were given a deck of cards and instructed to match the top card to 1 of 4 target cards. Matching occurs on the basis of one to three categories and the potential sorting criteria change throughout the test. This study employed the 64 card hand-administered version. The variables of interest were number of categories completed as well as the responses that were correct and/or perseverative.
Data analysisThis study was conducted using a small sample size where extreme data could affect statistical analysis. Because of this and in light of the fact that the scale for the majority of neuropsychological test employed were ordinal, all analyses were run using non-parametric statistics (Zhang & Zhang, 2009). Specifically, for each cognitive domain of IQ (Table 2), Attention (Table 3), Memory (Table 4) and Executive Function (Table 5), descriptive statistics (median and interquartile range-IQR) were computed and statistical comparisons between groups were made using a non-parametric Kruskall-Wallis test for independent samples (SPSSTR version 22). Following the recommendations of Ruxton and Beauchamp (2008) for a small set of comparisons, post- hoc analyses were conducted using a Mann Whitney U test (p<.05).
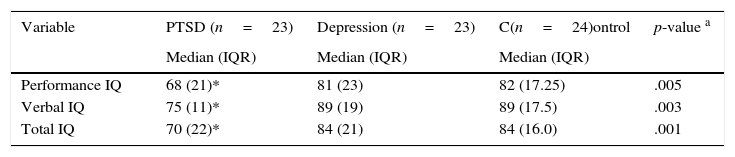
IQ descriptive statistics.
| Variable | PTSD (n=23) | Depression (n=23) | C(n=24)ontrol | p-value a |
|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | ||
| Performance IQ | 68 (21)* | 81 (23) | 82 (17.25) | .005 |
| Verbal IQ | 75 (11)* | 89 (19) | 89 (17.5) | .003 |
| Total IQ | 70 (22)* | 84 (21) | 84 (16.0) | .001 |
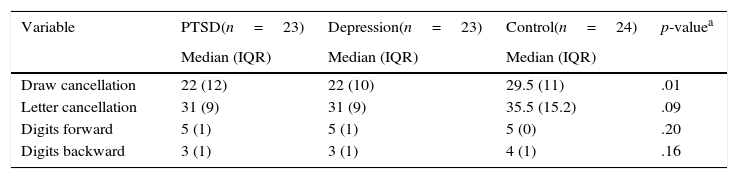
Attention descriptive statistics.
| Variable | PTSD(n=23) | Depression(n=23) | Control(n=24) | p-valuea |
|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | ||
| Draw cancellation | 22 (12) | 22 (10) | 29.5 (11) | .01 |
| Letter cancellation | 31 (9) | 31 (9) | 35.5 (15.2) | .09 |
| Digits forward | 5 (1) | 5 (1) | 5 (0) | .20 |
| Digits backward | 3 (1) | 3 (1) | 4 (1) | .16 |
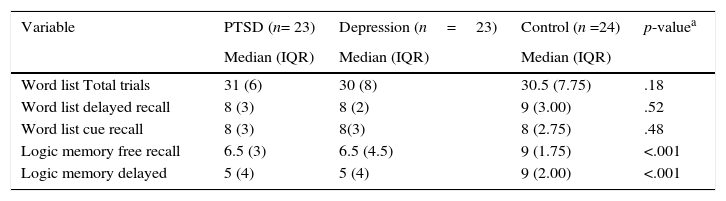
Memory descriptive statistics.
| Variable | PTSD (n= 23) | Depression (n=23) | Control (n =24) | p-valuea |
|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | ||
| Word list Total trials | 31 (6) | 30 (8) | 30.5 (7.75) | .18 |
| Word list delayed recall | 8 (3) | 8 (2) | 9 (3.00) | .52 |
| Word list cue recall | 8 (3) | 8(3) | 8 (2.75) | .48 |
| Logic memory free recall | 6.5 (3) | 6.5 (4.5) | 9 (1.75) | <.001 |
| Logic memory delayed | 5 (4) | 5 (4) | 9 (2.00) | <.001 |
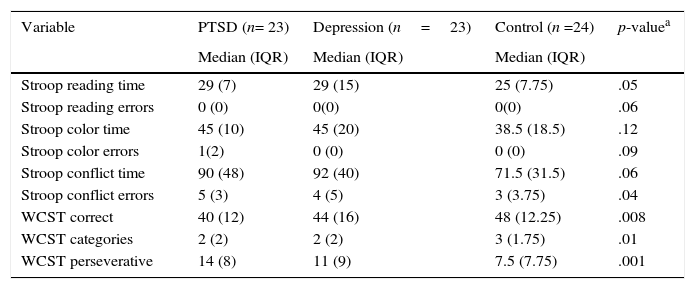
Executive function descriptive statistics.
| Variable | PTSD (n= 23) | Depression (n=23) | Control (n =24) | p-valuea |
|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | ||
| Stroop reading time | 29 (7) | 29 (15) | 25 (7.75) | .05 |
| Stroop reading errors | 0 (0) | 0(0) | 0(0) | .06 |
| Stroop color time | 45 (10) | 45 (20) | 38.5 (18.5) | .12 |
| Stroop color errors | 1(2) | 0 (0) | 0 (0) | .09 |
| Stroop conflict time | 90 (48) | 92 (40) | 71.5 (31.5) | .06 |
| Stroop conflict errors | 5 (3) | 4 (5) | 3 (3.75) | .04 |
| WCST correct | 40 (12) | 44 (16) | 48 (12.25) | .008 |
| WCST categories | 2 (2) | 2 (2) | 3 (1.75) | .01 |
| WCST perseverative | 14 (8) | 11 (9) | 7.5 (7.75) | .001 |
As can be seen in Table 2, PTSD participants had significantly lower Performance IQ, Verbal IQ and Total IQ scores compared to the depressed and control groups, with the latter two groups not significantly different from one another.
As shown in Table 3, the control group was significantly more accurate in draw cancellation compared to the PTSD and depressed groups, which did not differ from each other.
Inspection of Table 4 reveals that the PTSD and depressed groups were significantly less accurate in both free and delayed recall of logic memory (story ideas) compared to controls, while the PTSD and depressed groups did not differ from each other.
Related to Executive Function, Table 5 reveals that the PTSD and depressed groups, while not differing from one another on most measures, were significantly impaired relative to controls in several aspects of Executive Functioning—including Stroop reading time as well as conflict errors, WCST correct, WCST categories and WCST perseveration scores.
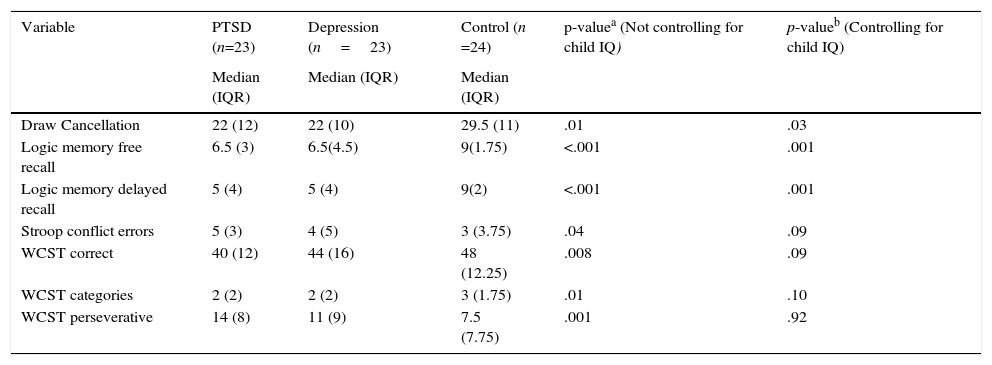
Due to the possible impact of overall IQ on the reported differences between groups, a rank Analysis of Covariance (Quade, 1967) for non-parametric data was also conducted to control for the potential impact of IQ on cognitive abilities. As seen in Table 6, when controlling for IQ, the differences in performance in the attention and memory domains remained statistically significant; however, differences in executive function were no longer statistically reliable.
Main Findings Controlling (not) for IQ.
| Variable | PTSD (n=23) | Depression (n=23) | Control (n =24) | p-valuea (Not controlling for child IQ) | p-valueb (Controlling for child IQ) |
|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | |||
| Draw Cancellation | 22 (12) | 22 (10) | 29.5 (11) | .01 | .03 |
| Logic memory free recall | 6.5 (3) | 6.5(4.5) | 9(1.75) | <.001 | .001 |
| Logic memory delayed recall | 5 (4) | 5 (4) | 9(2) | <.001 | .001 |
| Stroop conflict errors | 5 (3) | 4 (5) | 3 (3.75) | .04 | .09 |
| WCST correct | 40 (12) | 44 (16) | 48 (12.25) | .008 | .09 |
| WCST categories | 2 (2) | 2 (2) | 3 (1.75) | .01 | .10 |
| WCST perseverative | 14 (8) | 11 (9) | 7.5 (7.75) | .001 | .92 |
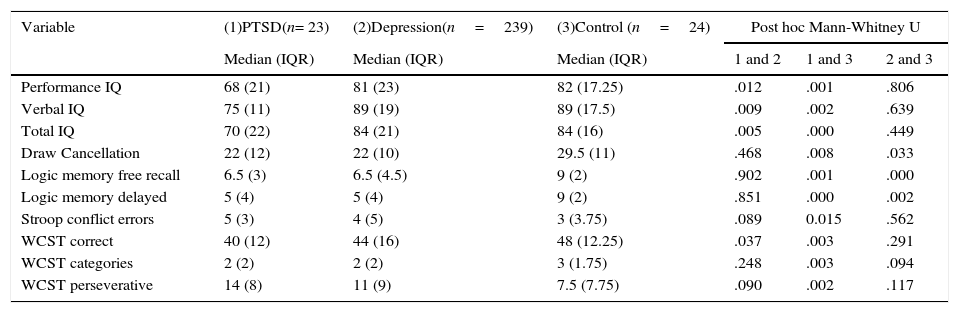
Post-hoc comparisons of the PTSD versus the depressed groups appear in Table 7 and show significant differences in IQ and number correct in WCST. However, no differences between the PTSD and depressed groups were found in the subtests comprising the domains of attention and memory, nor in the majority of subtests of executive function. It is interesting to note, however, that although not statistically reliable, the PTSD group tended to exhibit poorer performance in all cognitive domains/measures compared to the depressed and control groups.
Post-hoc Mann Whitney U analysis.
| Variable | (1)PTSD(n= 23) | (2)Depression(n=239) | (3)Control (n=24) | Post hoc Mann-Whitney U | ||
|---|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | 1 and 2 | 1 and 3 | 2 and 3 | |
| Performance IQ | 68 (21) | 81 (23) | 82 (17.25) | .012 | .001 | .806 |
| Verbal IQ | 75 (11) | 89 (19) | 89 (17.5) | .009 | .002 | .639 |
| Total IQ | 70 (22) | 84 (21) | 84 (16) | .005 | .000 | .449 |
| Draw Cancellation | 22 (12) | 22 (10) | 29.5 (11) | .468 | .008 | .033 |
| Logic memory free recall | 6.5 (3) | 6.5 (4.5) | 9 (2) | .902 | .001 | .000 |
| Logic memory delayed | 5 (4) | 5 (4) | 9 (2) | .851 | .000 | .002 |
| Stroop conflict errors | 5 (3) | 4 (5) | 3 (3.75) | .089 | 0.015 | .562 |
| WCST correct | 40 (12) | 44 (16) | 48 (12.25) | .037 | .003 | .291 |
| WCST categories | 2 (2) | 2 (2) | 3 (1.75) | .248 | .003 | .094 |
| WCST perseverative | 14 (8) | 11 (9) | 7.5 (7.75) | .090 | .002 | .117 |
The current study aimed to identify similarities and differences in the cognitive performance profiles of Colombian children and adolescents diagnosed with PTSD as compared to those with depression. The results revealed several interesting findings.
Regarding IQ, the present results are in agreement with previous studies suggesting that a measureable by-product of traumatic experience is a subsequent lowering of IQ (De Bellis et al., 2009). Saltzman et al. (2006) found an association between IQ and the number of real and re-experienced trauma episodes, suggesting that early traumatic experiences negatively impact on the development of cognitive abilities (and underlying IQ) in children and adolescents. Thus, the present difference in IQ between those with PTSD and those without suggests that rather than being a confounding factor, lower IQ is a consequence of (and not necessarily a predisposing factor for) childhood/adolescent trauma. Note that the present study analyzed data controlling for IQ differences between groups and still found differences between the PTSD and depressed groups in the attention and logical memory domains.
Regarding attentional processes, poorer performance on the draw cancellation task compared to the letter cancellation task suggest an alteration of visuospatial processing in both the PTSD and depressed groups. Because emotional processing and visuospatial processing depend extensively on the specialized functioning of the right hemisphere, Liotti and Mayberg (2001) suggested a common pathway may be involved for attentional processing in both the PTSD and depressed groups. In the present study even after controlling for IQ, the PTSD and depressed groups maintained their differences from the control group in attentional performance (lower for both). Note that this pattern contrasts with the findings of De Bellis et al. (2009), who reported no differences between a neglect group and a PTSD group after controlling for IQ.
Regarding memory, PTSD and the depressed groups both had poorer performance compared to the control group in logical (story) memory but not word memory, which suggests a very specific alteration of verbal memory for each group. Further, after controlling for IQ, this difference persisted, with post-hoc analysis revealing no difference between the PTSD and depressed groups for word memory. Note that lists of words and logical memory are two distinct tests used to assess verbal memory (Lezak et al., 2012), with logical memory consisting of a story, which includes chains (or “links”) between multiple semantic units. These chains are important in understanding story meaning and appear to be adversely affected by both PTSD and depression. By way of speculation, the deficits in memory processes reported in other studies (Johnsen, Kanagaratnam, & Asbjørnsen, 2008; Vasterling et al., 2002; Wagner et al., 2015) may be due specifically to a failure in linking chains of verbal information, and not necessarily to the recovery of individual verbal materials (i.e., words) from memory per se.
Alterations of executive function were found mainly in the PTSD group. Functional neuroimaging studies have shown alterations of frontal lobe activation in those with PTSD and/or depression, which may affect aspects of executive function, including inhibitory control, cognitive flexibility and pre-planning of actions (Olff, Polak, Witteveen, & Denys, 2014; Patel, Spreng, Shin, & Girard, 2012; Rive et al., 2013). Note that in the present study, however, when controlling for IQ, the executive functioning differences obtained between the two groups were rendered non-significant. As previously mentioned, the relationship between IQ and executive function is complex. Some previous studies have suggested no relation between IQ and executive function (Eslinger & Damasio, 1985), while others report a reliable association between IQ and several specific executive processes. For example, Salthouse, Fristoe, McGuthry, and Hambrick (1998) found that inhibitory control is strongly correlated with fluid intelligence, while Friedman et al. (2006) report differential correlations among IQ, working memory and set shifting. Further research is required to provide insights into this discrepancy.
In summary, this study compared similarities/differences between PTSD and depression in the cognitive domains of IQ, attention, memory and executive function. The findings provide evidence for generally lower performance of the PTSD group on most of the tests for each domain. However, the PTSD and depressed groups did show similar deficits in attention and logical memory as compared to control group level performance. Deficits in executive functioning were mainly found in the PTSD group and less so in the depressed group. Regarding IQ, a strong correlation with PTSD was found, which may indicate that IQ is a consequence of traumatic experience, rather than a predisposing factor. Further research, however, is required to confirm this claim and future research efforts might be directed towards exploring this relationship in PTSD children and adolescents, for whom IQ deficits are known to have a negative impact on their academic achievement.
For clinical purposes, the present findings suggest a strong relationship between disorders in which the emotional component is the predominant characteristic, and the cognitive processes associated with executive function, particularly inhibitory control. By way of speculation, rehabilitation of this link could be made part of a therapy regimen, one which focuses on improving the ability to control or regulate the impact of the emotional aspects of traumatic experiences. Or, in cases of depressed children, a program might aim to improve their ability to control cognitive processes like rumination (the latter being one of the main symptoms associated with depression). Given that a sense of control of physiological responses (via relaxation) and/or thoughts (using thought-stopping techniques) are current techniques employed by a variety of therapy programs, the present findings provide empirical support for why these techniques have a positive impact on the mental health of individuals suffering from PTSD and/or depression.
Limitations: Given the small sample size of the current study, generalizations cannot be readily drawn to the whole of the Colombian population or be extended to other sources of PTSD inducement. Additionally, given the high prevalence of PTSD and depression, and the limited literature on its neurocognitive consequences, longitudinal neurobiological studies are warranted. It is particicualry important to clarify if lower IQ is a predisposing factor or a consequence of traumatic experience.