Background/Objective: Depression is a common mental health disorder and an emerging public health concern. Few studies have investigated prevalence and predictors of depression severity in the Irish context. To investigate the relative contribution of known risk factors that predicts depression severity in a treatment-seeking sample of adults in Ireland. Method: As part of a randomised controlled trial of an internet-delivered intervention for depression participants (N=641) completed online screening questionnaires including BDI-II and information associated with common predictors of depression. Results: The mean score on the BDI-II was 24.13 (SD=11.20). Several factors were shown to predict greater severity of depression in the sample including female gender, younger age, unemployment, being single or partnered as opposed to married, previous diagnosis of depression, recent experience of life stressors. Alcohol use, recent losses, knowing a suicide completer, education level, type of employment and income level were not found to be significant. Conclusions: The study contributes to the profiling of the incidence and predictors of severity of depression in an Irish context. The results confirm some of the known risk factors and highlight the need for further research to be carried out on screening for depression and increasing access to interventions.
Antecedentes/Objetivo:La depresión es uno de los trastornos de salud mental más comunes y un incipiente problema de salud pública. Pocos estudios han investigado la prevalencia y factores predictivos de su gravedad en el contexto irlandés. El objetivo del estudio fue investigar los factores de riesgo que predicen la gravedad de la depresión en una muestra de adultos en Irlanda en búsqueda de tratamiento. Método: Los participantes auto-referidos accedieron a una intervención en línea para la depresión. Los participantes (N=641) completaron cuestionarios, incluyendo el BDI-II e información asociada con predictores comunes de la depresión. Resultados: Se encontraron varios factores que predijeron la gravedad de la depresión: ser mujer, ser joven, estar desempleado, estar soltero o con pareja pero no casado, tener diagnóstico previo de depresión y experiencia reciente con factores vitales estresantes. Conclusiones: El estudio contribuye a la elaboración de perfiles de incidencia y factores predictivos en la gravedad de la depresión. Los resultados confirman algunos de los factores de riesgo conocidos y ponen de relieve la necesidad de nuevas investigaciones que lleven a cabo la detección de la depresión así como un mayor acceso a las intervenciones.
Depression is considered to be one of the primary causes of disease rates worldwide. It has shown high rates of lifetime prevalence and high chronicity, as well as early age onset and role impairment (Richards, 2011). Depression accounts for 4.5% of total disability adjusted life years; it is reported to be on the increase in the general population and is considered a major concern for public health (World Health Organization [WHO], 2008). The WHO has projected depression to be the number one cause of chronic illness in high-income countries by 2030 (WHO, 2008). Twelve month prevalence rates have been estimated at 5%-8% in Europe and 6% in Ireland based on DSM-IV criteria and as high as 12.8% for all depressive disorders in urban Ireland.
International epidemiological studies have identified several important factors that significantly predict depression severity; these include age, marital status, any previous episodes of depression, any recent significant losses, relationship difficulties, unemployment, and lifestyle stresses (Richards, 2011; Richards & Salamanca-Sanabria, 2014). Prevalence rates and gender differences are reported to be somewhat constant across the adult lifespan (Richards, 2011). In Ireland for example, the Central Statistics Office (Central Statistics Office [CSO], 2008) has reported that 68% of those reporting emotional, psychological and mental health illness were between the ages of 18 to 64 years (working age). This report also highlighted some gender difference in depression prevalence: 53% female and 47% male although reports are generally higher for females (CSO, 2008).
Depression is associated with losses in quality of life and increased mortality rates. In spite of this, access to evidence–based psychological and psychiatric diagnosis and treatments are severely limited throughout the world, including Ireland. On a global scale many affected individuals receive no medical diagnosis nor seek treatment (Andrews, Sanderson, Slade, & Issakidis, 2000). The worldwide treatment gap in depression has been estimated at 56.3% (Kohn, Saxena, Levav, & Saraceno, 2004). Several barriers to accessing treatment exist, such as waiting lists, lack of motivation for change, negative perception of psychological and (or) drug treatments, costs, and personal difficulty such as stigma; each can play an important role in choosing to seek diagnosis and treatment (Kohn et al., 2004; Mohr et al., 2010).
The context: IrelandStudies on the prevalence of depression in Ireland are far fewer in comparison to other high-income countries; however those in existence have established similar rates to the reports found in the worldwide prevalence literature (CSO, 2008; Richards, 2011). The point prevalence figures taken from the Health Research Board's findings indicate that nationally 12 in every 100 people aged 18 years and over experience mild to severe mental illness (Tedstone-Doherty, Moran, & Kartalova-O’Doherty, 2008). Recent government policies such as Healthy Ireland Framework 2013–2025 (Health Service Executive, 2013) acknowledge the need to develop appropriate mental health services across the whole community so that individuals with mental illness can achieve a good quality of life through accessing community-based, specialist services. However, the reality of bridging the gap between policy and practice is far from resolved. In a survey carried out by the Health Research Board, only 10% of respondents had accessed treatment from a GP in the previous year for mental health issues, and service use at secondary level was lower still than primary care level (Tedstone-Doherty et al., 2008).
Aims and hypothesisOther studies that have examined risk factors associated with depression have some data from Ireland but generally the data has been only one part of a larger sample, for instance a European sample (Ayuso-Mateos et al., 2001). It is therefore the case that sampling in many studies has only been partial, for instance in Ayuso-Mateos et al. (2001), the samples were taken from one part of an urban region and a small rural region, and the authors have detailed the methodological problems they encountered with this study. Additionally the literature exposes numerous risk factors, but together in an Irish sample they have not been examined in detail. This study aimed to include as many of the well-know factors and examine them in a more complete state in a national sample. As such, we used multiple regression to assess the relative contribution of predictors of depression severity in a treatment-seeking sample of adults in Ireland. We hypothesised that many of the know predictors of depression would be positively associated with depression severity in the sample.
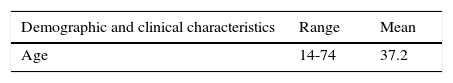
MethodParticipantsIreland has a population of 4,609,600 people, composed of 51% women and 49% men. Fifty-six percent of the population is between 15 and 55 years of age. As part of the screening procedure for a randomized controlled trial offering an online intervention for depression (Richards et al., 2014, 2015), six-hundred and forty-one participants (N=641) completed the screening questionnaires and were included in this analysis. The sample was composed of 27% men and 73% women. The age range was 14-74 (M=37.2, SD=10.62). To exclude multiple instances/visits to the website and consequently to the screening the sample only included unique participants who were identified through a unique and who thereafter engaged in the supported online intervention. The study protocol (Richards et al., 2014) had outlined that all participants who were screened irrespective of severity were able to avail of supported treatment.
MeasuresParticipants provided information on personal demographic factors such as age and gender. In addition, participants provided information regarding common predictors of depression including: employment and marital status (partnered, married, separated, divorced, single, other), number of dependents, previous diagnosis of depression, recent loss and difficulties in different life areas (work, financial, partner, family, or other). Participants answered questions relating to current suicidal ideation or intent, knowing anyone who completed suicide, and family history of depression. Lastly, participants provided an evaluation of the frequency of their personal alcohol consumption (once a week, twice a week, three times a week).
The Beck Depression Inventory (BDI-II; Beck, Steer, & Brown, 1996). The 21-item Beck Depression Inventory-Second Edition (BDI-II) is a widely used questionnaire developed for the assessment of depressive symptoms that correspond to the criteria for depressive disorder diagnosis as outlined in The American Psychiatric Associations Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (American Psychiatric Association, 2000). Each item includes four self-report statements scored on a scale from 0 to 3. The BDI-II manual states that a cutoff score of 17 has yielded a 93% specificity and 18% sensitivity for the presence of major depression (Beck et al., 1996). The scale designates levels of severity, Minimal (0–13); Mild (14–19); Moderate (20–28); and Severe (29–63) (Beck et al., 1996).
ProcedureBetween January 2014 and March 2014 participants were invited to participate in an online intervention for depression (Richards et al., 2015). The intervention and study were advertised through social media and radio adverts. Access to the study was made available through the Aware website. Aware is a national charity for depression in Ireland. Participants completed online information including baseline screening questionnaires, the BDI-II, demographic and clinical characteristics, and information on predictors for depression. The per protocol screening did include other measures of comorbidity (e.g. Generalized Anxiety Disorder [GAD-7]), and those with self-reported depression as the principal diagnosis were included even with comorbidity. After 3 months a total of 641 unique responses were received. The study protocol, information on the study, informed consent and related materials were submitted and approved by the School of Psychology, Trinity College Dublin ethics committee (22/11/2013). Informed consent was obtained from all participants in the study.
Data analysisAll 641 participants provided complete data and were included in the analysis. Descriptive statistics established mean and point prevalence of depression in the sample and also the percentages across the levels of severity of symptom presentation, as defined by their BDI-II scores (Beck et al., 1996). Linear hierarchical multiple regression was used to determine predictors of scores on the BDI-II. The most common response was used for the dummy/reference variable.
ResultsThe characteristics for the sample are presented in Table 1. In terms of scores on the BDI-II, total scores ranged from 0-57 out of 63. The mean depression in the sample was 24.13 (SD=11.20), which is within the moderate symptom severity according to the BDI-II manual (Beck et al., 1996). In terms of severity of symptom presentation, 17.8% (n=114) were minimal, 18.4% (n=118) mild, 31% (n=199) moderate and 32.8% (n=210) severe. While previous diagnosis of depression has been noted we did not collect further information on the nature of any past diagnosis, such as treatment resistant depression (Pérez-Wehbe, Perestelo-Pérez, Bethencourt-Pérez, Cuéllar-Pompa, & Peñate-Castro, 2014).
Characteristics of the current sample (N=641).
| Demographic and clinical characteristics | Range | Mean |
|---|---|---|
| Age | 14-74 | 37.2 |
| % | n | |
|---|---|---|
| Gender | ||
| Female | 73 | 468 |
| Male | 27 | 173 |
| Education Level | ||
| None | 1.6 | 10 |
| High School | 19 | 122 |
| Undergraduate Degree | 30.1 | 193 |
| Postgraduate Degree | 26.7 | 171 |
| Other Certificate | 22.6 | 145 |
| Current Work | ||
| Working | 63.3 | 406 |
| Not working | 36.7 | 235 |
| Employment Status | ||
| Unemployed | 16.2 | 104 |
| Full time employed | 44 | 282 |
| Part time employed or student | 24.5 | 157 |
| Disabled | 1.2 | 8 |
| At home parent | 11.4 | 73 |
| Retired | 2.7 | 17 |
| Civil Status | ||
| Married | 39.3 | 252 |
| Divorced | 1.9 | 12 |
| Have a partner | 18.7 | 120 |
| Other | 2.3 | 15 |
| Separated | 2.8 | 18 |
| Single | 34.9 | 224 |
| Number of Dependents | ||
| None | 55.4 | 355 |
| 1-2 | 29.6 | 190 |
| 3+ | 15 | 96 |
| Previous Diagnosis of Depression | ||
| None | 43.1 | 276 |
| Previous diagnosis | 56.9 | 365 |
| Experienced Recent Loss | ||
| Yes | 76.9 | 493 |
| No | 23.1 | 148 |
| Knew Suicide Completer | ||
| Yes | 18.9 | 121 |
| No | 81.1 | 519 |
| Family History of Depression | ||
| Yes | 51 | 327 |
| No | 49 | 314 |
| Frequency of Alcohol Consumption | ||
| Never or infrequently | 43.2 | 277 |
| Once or twice per week | 44.3 | 284 |
| 3+ times per week | 12.5 | 80 |
| Annual Income | ||
| <€11k | 28.2 | 181 |
| €11-22k | 18.9 | 121 |
| €22-44k | 34 | 218 |
| €44k+ | 18.9 | 121 |
| Recent Life Stresses | ||
| Family | 15 | 96 |
| Financial | 15.1 | 97 |
| Work | 22.6 | 145 |
| Partner | 4.4 | 28 |
| Other | 18.4 | 118 |
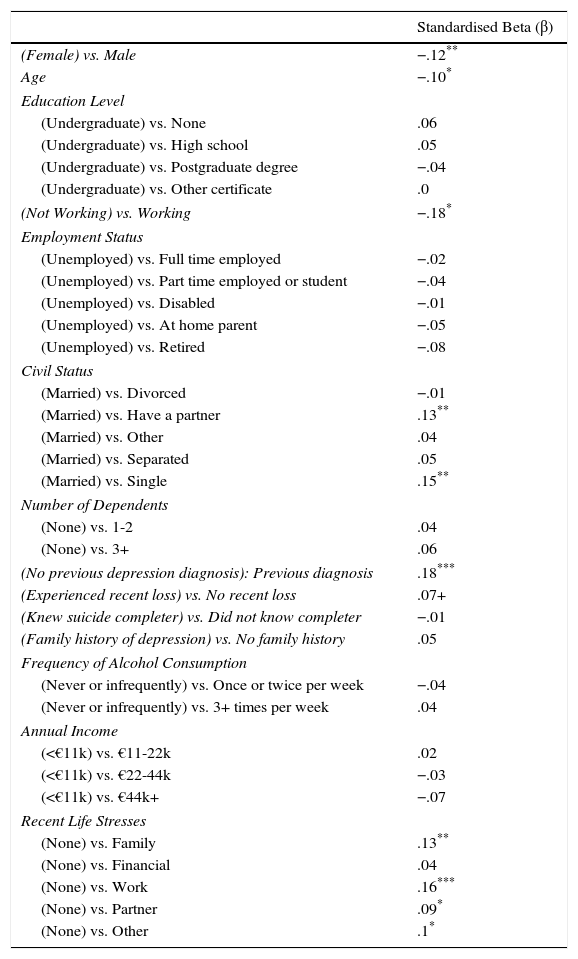
The final linear regression model including all demographic variables significantly predicted BDI-II total scores: F(33, 606)=4.93, p<.001, adjusted R2=.17. Table 2 displays the significance of individual predictors in the model. Greater depression severity was significantly predicted by female gender, younger age, unemployment, being single or having a partner compared to those who were married. Scores were also higher for those who reported having a previous diagnosis of depression, those who had recently experienced family, work, partner or other life stressors. There was no significant impact of educational level, type of employment, number of dependent children, knowing someone who had completed suicide, family history of depression, and frequency of alcohol consumption or annual income.
Significance of individual predictors in final regression model.
| Standardised Beta (β) | |
|---|---|
| (Female) vs. Male | −.12** |
| Age | −.10* |
| Education Level | |
| (Undergraduate) vs. None | .06 |
| (Undergraduate) vs. High school | .05 |
| (Undergraduate) vs. Postgraduate degree | −.04 |
| (Undergraduate) vs. Other certificate | .0 |
| (Not Working) vs. Working | −.18* |
| Employment Status | |
| (Unemployed) vs. Full time employed | −.02 |
| (Unemployed) vs. Part time employed or student | −.04 |
| (Unemployed) vs. Disabled | −.01 |
| (Unemployed) vs. At home parent | −.05 |
| (Unemployed) vs. Retired | −.08 |
| Civil Status | |
| (Married) vs. Divorced | −.01 |
| (Married) vs. Have a partner | .13** |
| (Married) vs. Other | .04 |
| (Married) vs. Separated | .05 |
| (Married) vs. Single | .15** |
| Number of Dependents | |
| (None) vs. 1-2 | .04 |
| (None) vs. 3+ | .06 |
| (No previous depression diagnosis): Previous diagnosis | .18*** |
| (Experienced recent loss) vs. No recent loss | .07+ |
| (Knew suicide completer) vs. Did not know completer | −.01 |
| (Family history of depression) vs. No family history | .05 |
| Frequency of Alcohol Consumption | |
| (Never or infrequently) vs. Once or twice per week | −.04 |
| (Never or infrequently) vs. 3+ times per week | .04 |
| Annual Income | |
| (<€11k) vs. €11-22k | .02 |
| (<€11k) vs. €22-44k | −.03 |
| (<€11k) vs. €44k+ | −.07 |
| Recent Life Stresses | |
| (None) vs. Family | .13** |
| (None) vs. Financial | .04 |
| (None) vs. Work | .16*** |
| (None) vs. Partner | .09* |
| (None) vs. Other | .1* |
Note: Dummy/reference variables are in brackets. If β is + the comparison variable is associated with a higher BDI score, if β is -, the dummy variable is associated with a higher BDI score.
+ p=.052,
The study examined several factors associated with severity of depression and revealed that female gender, younger age, unemployment, unmarried, a previous diagnosis of depression, and some recent life stressors were positively associated with depression severity in the sample. The influence of these factors is consistent with previous literature on factors associated with depression in the general adult population in Ireland and in general adult populations worldwide. In contrast, there was no significant association with factors including educational level, employment status, number of dependents, knowing someone who had completed suicide, family history of depression, drinking frequency and income, although other studies have shown these to be determinants of depression severity (Hölzel, Härter, Reese, & Kriston, 2011).
GenderThe current study is supportive of the general literature regarding the prevalence of depression in an adult population and gender being a significant predictor of depression severity (Richards, 2011). Community studies carried out over the last four decades have consistently reported higher rates of depression in women (Brossart et al., 2013; Romans, Cohen, & Forte, 2011). The results of a European study carried out in 23 countries, including Ireland, found that in a population aged 18-75, women reported higher levels of depression than men in all countries (Van de Velde, Bracke, & Levecqe, 2010).
Various speculations have been made with regard to this disparity between genders. In general, women are reported to be twice as likely to experience depression as men for reasons such as gender related stressors, low self-esteem and differences in coping styles (Kessler, 2005). Most current research acknowledges that gender differences in depression are a consequence of the interaction between biological, psychological and social factors (Van de Velde et al., 2010). Some theories have focused on social factors relating to women's role and status in society and particular biological differences, although the explanation remains unclear (Nolen-Hoeksema, 2001). Additionally, it has been speculated that females are more likely to seek help and acknowledge symptoms whereas males have the tendency to under report experiences of depressive symptoms (Nolen-Hoeksema, 2001). A review of a number of studies by Piccinelli and Wilkison (2000) revealed that several correlates of depression such as sleep disturbance and somatic anxiety were over-represented as depressive symptoms in women rather than mood-specific features. Future research should examine the possibility of measurement response bias in relation to gender differences and depression.
AgeThe onset of depressive disorders is reported to start at any age and prevalence patterns of each age group for men and women are often inconsistent. In the current sample, younger age was significantly associated with depression. Although there is consistency across previous studies regarding the age of onset, these results support emerging evidence of a decrease in age over the last half-century (Hirschfeld & Weisman, 2002). Recent trends suggest that depression is becoming more common (or at least being diagnosed more commonly) in younger age groups. In Ireland 68% of those reporting emotional, psychological and mental health disabilities are of working age (18-64 years age group; CSO Ireland, 2008). The indication for earlier age onset of symptoms would have consequences for services provision and preventative efforts.
Employment statusThe results of this study support previous research that suggests that unemployment is consistently associated with high rates of depression among adults. For instance, in a meta-analysis carried out by Paul and Moser (2009) on the effects of unemployment on mental health variables, including depression, the results showed a significant difference in depression between individuals who were not working and those who were employed. Emerging research from the U.S. on unemployment and depression rates in young adults gathered from the 2010 Behavioral Risk Factor Surveillance System (BRFSS) (Centers for Disease Control and Prevention, 2010) has found similar results which suggest that individuals who are unemployed are three times more likely to report symptoms of depression compared to their employed counterparts (McGee & Thompson, 2015). Several theories have offered to explain the link between unemployment and depression, which speculates that mental distress is a consequence of an individual being deprived of time structure, social contact, collective purpose, status and activity which are all associated with important psychological needs (Paul & Moser, 2009).
Civil statusThe results of the current study suggest that being single or having a partner rather than being married is predictive of depression. These results are consistent with previous studies regarding depression and marital status (Bulloch, Williams, Lavorato, & Patten, 2009). Previous research on marital status and mental health has consistently shown that married people have a lower prevalence of depression than those who are nonmarried (Bulloch et al., 2009). Married people have better mental health than both unmarried people who live alone and those that live with others, such as a partner. The results of a study carried out on 23 European countries on factors relating to depression indicated that married individuals reported lower levels of depression than those who were divorced, separated, widowed and single. Additionally, this study also showed that there was a strong association recorded between depression and the absence of a partner for both genders with no significant variation among the 23 countries (Van de Velde et al., 2010). With the recent legalisation on same-sex marriage in Ireland it will be interesting to explore this aspect into the future, and also this study did not examine the impact of sexual orientation on depression symptoms.
Previous diagnosis of depressionThe results show that a previous episode of depression was significantly associated with severity of depression. This supports the literature on recurrence after recovery and relapses during a time of recovery for individuals with depression (Solomon et al., 2000; Stegenga et al., 2013). It has become widely accepted that depression is a highly recurrent disorder with reports estimating that at least 50% of those who recover from an initial episode of depression go on to have one or more additional episodes in their lifetime (Judd et al., 2000; Solomon et al., 2008). Similarly, several studies have reported relapse rates of between 30%–50% (Judd et al., 2000; Solomon et al., 2008). The possibility of future episodes of depression seems to increase with subsequent episodes (Richards, 2011) with reports of approximately 80% of those with a history of two episodes having another recurrence. Factors shown to increase an individual's vulnerability for relapse and recurrence include a history of depression, psychiatric illness, the quality of any recovery from a previous episode, is a woman, a history of family depression, and any recent loss (Judd et al., 2000; Richards, 2011; Solomon et al., 2000, 2008). In addition research has shown how factors such as depressed patients with comorbid anxiety and not taking medication are at risk of dropping out from treatments (Lopes, Gonçalves, Sinai, & Machado, 2015).
Recent life stresses (family, work, partner or other)This study found that recent life stresses relating to work and relationship difficulties with family and partner were significantly predictive of depression severity. The association between depression and stressful life events has been demonstrated extensively (Mazure, 2006; Plieger, Melchers, Montag, Meermann, & Reuter, 2015). Individuals with depression are often found to be living in highly stressful family environments that include marital discord and at times family members with mental illness (Hammen, 2003). In a review of the literature Burcusa and Iacono (2007) concluded that there was considerable evidence to support that stressful life events in adulthood such as demands and conflicts with children, and negative interactions with spouses are notable risk factors for recurrent depression. Also depressive symptoms that develop in adolescence have been shown to have a considerable impact on health outcomes into adulthood (Cumsille, Martínez, Rodríguez, & Darling, 2015).
Work stress was also found to be an independent risk factor for depression as detailed in a large study by Wang, Simon and Kessler (2003) among 6,663 Canadian workers aged 18 to 64 years. A systematic review on workplace factors and risk of depression showed consistent findings that adverse factors in the workplace are associated with an elevated risk of depressive symptoms (Bonde, 2008). Another study carried out in Australia with disability support staff also found that workplace stress was associated with greater levels of depression (Mutkins, Brown, & Thorsteinsson, 2011). Stressors in life are multiple and more refined examination of variables that may occupy the categories described above might be required before definitive conclusions are drawn. The results of this research support the view that life stressors can have a deleterious effect on one's mental health.
Non-significant factorsEducational level, employment status, annual income, number of dependents, having experienced a recent loss, knowing someone who completed suicide, frequency of alcohol consumption, and family history of depression, were all non-significant in the current sample. This is inconsistent with some previous research, which has linked these variables to depression (Barry et al., 2009; Bjelland et al., 2008; Kessler & Bromet, 2013; Lorant et al., 2003).
The current results were inconsistent with those of a national report which reported findings consistent with worldwide literature regarding socio-economic status’ (SES), which includes education level, employment and income, being predictors for depression in Ireland (Barry et al., 2009). The finding in this study of no effect of financial difficulties is also inconsistent with research showing that those in debt are three times more likely to experience depression (Richardson, Elliott, & Roberts, 2013). It is possible that factors specific to the current sample, which was mainly composed of highly educated individuals in employment and under-represented individuals from lower SES, may have been captured. This may be indicative of a shift whereby traditionally protective factors linked to a higher SES, may no longer be serving such a function following the recent economic recession. A higher SES may no longer protect from economic hardship, which has consistently been reported as a predictor of depression (Bjelland et al., 2008; Chazelle et al., 2011); additionally individuals from higher SES backgrounds may not have the psychological resources to cope with economic adversity (Fitch, Mamo, & Campion, 2014; Mental Health Commission, 2011). Employment and high education levels may also be nesting new work-related or financial stressors, which were in fact the main stressors reported by the current sample. While this is speculative it may be an area future research may investigate further to develop a better picture of current factors mediating mental health difficulties and depression in Ireland.
Due to the fact that only the frequency of alcohol consumption was assessed, and not consumption levels, meant that the full picture of alcohol use was not captured. Alcohol use as well as family history of or suicide are also still taboo and subject to stigma in Ireland, which may have resulted in participants under-reporting or not being aware about such instances in their personal history.
Also, some other confounding variables which were not investigated in the current study, e.g. social support, may have played a role in buffering the impact of other stressful events such as losses.
Strengths and limitations of the studyThe current study had a good sample size and is the first to attempt to investigate factors of importance to people seeking treatment for depression in Ireland. Research on depression prevalence and risk factors in the Irish context has been sparse and the current research makes a contribution to build a national body of evidence. In particular it gives us some insight into the reasons why people might be seeking or needing treatment. Factors such as those identified are useful for clinicians to understand in building a profile of the patient and their needs. Such information is also useful to those responsible for wellbeing in various areas of a person's life such as work and family relationships. The knowledge can also help inform the development of interventions that addresses these significant factors for Irish people seeking treatment.
However caution should be taken in generalizing results concerning prevalence as the sample could have been affected by self-selection bias and the gender differences are not fully representative of the general Irish population. Also they are a treatment-seeking sample and therefore cannot be representative of the general population. In addition, some significant predictor variables for depression may also have not been captured; for instance, other studies have noted differences in prevalence rates across urban and rural communities, levels of social support and type of employment.
A limitation of this study is that it did not include an official diagnosis of participants; rather levels of depression and associated risk factors were self-reported by the participants, which may incur some recall and reporting bias in spite of participants having been asked to think carefully and answer as honestly as possible. Another limitation of this study is that it is a cross-sectional study design that limits the determination of the temporal relationship between the studied independent variables and depression to establish the cause-effect relationship.
ImplicationsThe current research data was collected as part of routine screening for recruitment into a Randomized Controlled Trial of an internet-delivered intervention for depression. The response to the invitation for an intervention was high and confirms the need and demand for services. Given the high levels of depressive symptoms in the community, the study has shown the potential for internet-delivered interventions to reach individuals and that they may have a considerable influence especially in areas where services are underdeveloped and where access is limited (Richards et al., 2015). Lastly, understanding factors that may increase people's vulnerability to depression can directly influence the development of psychological interventions to make them more targeted and effective.
ConclusionOur results demonstrate a high prevalence of depression in the particular sample investigated and significantly different for women compared to men. Several factors have been shown to be significantly associated with greater severity of depression in the sample, and these include being a woman, younger age, not working, single status or having a partner vs. married, a previous diagnosis of depression, and recent experience of family, work, partner or other life stresses.
Our research shows that severity of depression reported resemble those reported in other studies of general adult populations in Ireland and worldwide (Richards, 2011; Tedstone-Doherty et al., 2008). Our results highlight the extensive clinical need in a context where the majority of affected individuals have no medical diagnosis nor seeks treatment. In addition, a large percentage of individuals with mental health problems in Ireland do not access or cannot access the services they require (Health Service Executive, 2013).
In the context in which the data was collected there seems to be an opportunity to recognise both the need for help-seeking and treatment and the possibility of extending access through the use of internet-delivery, evidence-based and empirically supported interventions. Further such internet-delivered interventions can have a role at different stages of implementation form prevention to treatment to maintenance and across different target groups.