A significant number of psychotherapy clients remain untreated, and dropping out is one of the main reasons. Still, the literature around this subject is incoherent. The present study explores potential pre-treatment predictors of dropout in a sample of clients who took part in a clinical trial designed to test the efficacy of narrative therapy for major depressive disorder compared to cognitive-behavioral therapy. Logistic regression analysis showed that: (1) treatment assignment did not predict dropout, (2) clients taking psychiatric medication at intake were 80% less likely to drop out from therapy, compared to clients who were not taking medication, and (3) clients presenting anxious comorbidity at intake were 82% less likely to dropout compared to those clients not presenting anxious comorbidity. Results suggest that clinicians should pay attention to depressed clients who are not taking psychiatric medication or have no comorbid anxiety. More research is needed in order to understand this relationship.
Un número significativo de clientes de psicoterapia no recibe tratamiento adecuado y el abandono del mismo es una de las principales razones. La literatura existente al respecto es contradictoria. Este estudio explora potenciales predictores del abandono en una muestra de clientes que participaron de un ensayo clínico diseñado para demostrar la eficacia de la terapia narrativa en el trastorno depresivo mayor en comparación con la terapia cognitivo-conductual. Los resultados muestran que (1) la asignación del tratamiento no predecía el abandono, (2) los clientes que al comenzar el tratamiento estaban medicados tuvieron un 80% menos de probabilidad de abandonar la psicoterapia, comparado con los clientes no medicados y (3) los clientes que padecían de comorbilidad ansiosa tuvieron un 82% menos de probabilidad de abandonar la psicoterapia comparado con los clientes sin comorbilidad. Los clínicos deberían prestar especial atención a los clientes sin medicación o que no padezcan de comorbilidad ansiosa. Se requiere más investigación para comprender esta relación.
A high number of psychotherapy clients remain untreated and dropout is one of the main reasons, since rates are high (approx. 20%, up to 74%; Swift & Greenberg, 2012). Few predictors of dropout have emerged recurrently in research, such as low socio-economic status (Reis & Brown, 1999), being married or living with a partner, previous experience with psychotherapy (Werner-Wilson & Winter, 2010), low education (Swift & Greenberg, 2012), older age (Pomp, Fleig, Schwarzer, & Lippke, 2013), being African-American (Lester, Artz, Resick, & Young-Xu, 2010), being female (Shamir, Szor, & Melamed, 2010), suffering from low levels of anxiety and/or depression (Baekeland & Lundwall, 1975), less clinical experience of therapists (Roos & Werbart, 2013; Swift & Greenberg, 2012) and weaker alliance (Sharf, Primavera, & Diener, 2010). Still, most researchers who have investigated psychotherapy dropout agree that there is no clear evidence for a pattern of dropout predictors (Baekeland & Lundwall, 1975; Casares-López et al., 2011; Swift & Greenberg, 2012). The aim of this study is to explore the attrition data of a psychotherapy clinical trial by assessing potential pre-treatment predictors for dropping out of treatment.
MethodParticipants, therapists, procedures and treatment conditions are described in more details in the original report of the study (Lopes et al., 2014).
ParticipantsSixty-three clients diagnosed with moderate Major Depressive Disorder (MDD) according to the DSM-IV (American Psychiatric Association, 2000) were assigned to either narrative therapy (NT, n=34) or cognitive-behavioral therapy (CBT, n=29). No significant treatment group differences were found [i.e., 81% female, mean age of 35.44 years old (SD=11.51), 79.4% had comorbid anxiety and 60.3% entered treatment taking psychiatric medication]. Ten therapists, all psychologists, with an average of 1.9 years of clinical experience (SD=2.13) met clients individually.
Dropout rate was 36.50% [NT=41%, CBT=31%; χ2(1)=0.32, p=.568]. Dropout was defined as the unilateral termination by the client without the therapist's approval or knowledge (Jung, Serralta, Nunes, & Eizirik, 2013).
Treatment conditionsThe CBT (Beck, Rush, Shaw, & Emery, 1979) and NT (White, 2007) treatment manuals consisted of 20 sessions and made similar requirements on the clients (e.g., completion of forms, in- and out-of-session assignments).
Measures- -
Structured Clinical Interview for DSM-IV (First, Spitzer, Gibbons, & Williams, 2002) was used to gather clients’ demographic (i.e., age, gender, relationship status, professional status and education) and clinical information (i.e., global assessment of functioning [GAF], presence of anxious co-morbidity, medication at intake, previous hospitalizations, previous suicide attempts and previous psychotherapy).
- -
Graffar Index (Graffar, 1956) was used to measure socio-economic status (SES).
- -
Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) was used to measure baseline severity of depressive symptoms.
- -
Outcome Questionnaire (OQ45.2; Lambert et al., 1996) and its subscales were used to measure general psychological distress, interpersonal problems and social role.
- -
Working Alliance Inventory (WAI-C; Horvath & Greenberg, 1989) was used at session four to assess the quality of working alliance from the perspective of 40 completers and 15 dropout clients.
Of the 23 clients who eventually dropped out, 48% did so by the end of the fourth session, and 91% left treatment before the 11th session. Mean length of stay in treatment for the dropout group was 6.4 (SD=4.4).
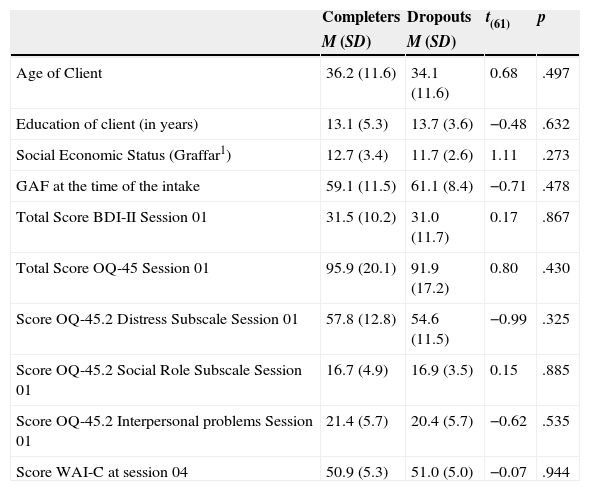
Prediction of dropoutAs shown on Table 1, t tests and chi-square tests were used to compare dropouts and completers on general characteristics (age, gender, years of education, socioeconomic status, marital status, and employment status), clinical characteristics at intake (GAF, anxious comorbidity, being medicated, previous hospitalization, previous suicide attempt, previous psychotherapy and pre-treatment scores on the BDI-II, OQ-45.2 and its subscales), process related variables (treatment assignment and WAI-C score) and a therapist variable (clinical experience). Those at least marginally significant entered a logistic regression model predicting dropout. Only consumption of medication [χ2(1)=6.79, p=.009] and anxious comorbidity at intake [χ2(1)=3.15, p=.076] met that criterion. When entered in the logistic regression model, these variables showed independent effects on the odds of dropping out of treatment. Medicated clients were 80% less likely to drop out, compared to non-medicated clients [OR=0.2 (95% CI=0.063-0.639), p=.007]. Clients presenting anxious comorbidity were 82% less likely to drop out compared to those not presenting anxious comorbidity [OR=0.182 (95% CI=0.033-1.016), p=.0520].
Comparison of completers and dropouts according to continuous and discrete pre-treatment variables.
| Completers | Dropouts | t(61) | p | |
|---|---|---|---|---|
| M (SD) | M (SD) | |||
| Age of Client | 36.2 (11.6) | 34.1 (11.6) | 0.68 | .497 |
| Education of client (in years) | 13.1 (5.3) | 13.7 (3.6) | −0.48 | .632 |
| Social Economic Status (Graffar1) | 12.7 (3.4) | 11.7 (2.6) | 1.11 | .273 |
| GAF at the time of the intake | 59.1 (11.5) | 61.1 (8.4) | −0.71 | .478 |
| Total Score BDI-II Session 01 | 31.5 (10.2) | 31.0 (11.7) | 0.17 | .867 |
| Total Score OQ-45 Session 01 | 95.9 (20.1) | 91.9 (17.2) | 0.80 | .430 |
| Score OQ-45.2 Distress Subscale Session 01 | 57.8 (12.8) | 54.6 (11.5) | −0.99 | .325 |
| Score OQ-45.2 Social Role Subscale Session 01 | 16.7 (4.9) | 16.9 (3.5) | 0.15 | .885 |
| Score OQ-45.2 Interpersonal problems Session 01 | 21.4 (5.7) | 20.4 (5.7) | −0.62 | .535 |
| Score WAI-C at session 04 | 50.9 (5.3) | 51.0 (5.0) | −0.07 | .944 |
| n (%) | n (%) | χ2(1,3) | p | |
|---|---|---|---|---|
| Treatment assignment | ||||
| Narrative Therapy | 14 (41.2%) | 20 (50%) | 0.70 | 0.404 |
| Cognitive Behavioural Therapy | 9 (31%) | 20 (50%) | ||
| Level of therapist experience | ||||
| Novice | 12 (30.0%) | 4 (17.4%) | 1.31 | .520 |
| Apprentice | 1 (2.5%) | 1 (4.3%) | ||
| Graduate | 27 (67.5%) | 18 (78.3%) | ||
| Gender of the client | ||||
| Female | 33 (82.5%) | 18 (78.3%) | 0.17 | .680 |
| Male | 7 (17.5%) | 5 (21.7%) | ||
| Relationship status | ||||
| Married | 15 (37.5%) | 6 (26.1%) | 3.41 | .333 |
| Single | 17 (42.5%) | 10 (43.5%) | ||
| Divorced | 6 (15.0%) | 7 (30.4%) | ||
| Widowed | 2 (5.0%) | 0 (0.0%) | ||
| Professional status | ||||
| Employed | 18 (45.0%) | 14 (60.9%) | 3.94 | .268 |
| Unemployed | 12 (30.0%) | 2 (8.7%) | ||
| Student | 9 (22.5%) | 6 (26.1%) | ||
| Retired | 1 (2.5%) | 1 (4.3%) | ||
| Previous psychotherapy | ||||
| No | 35 (87.5%) | 20 (87.0%) | 0.00 | .950 |
| Yes | 5 (12.5%) | 3 (13.0%) | ||
| Previous suicide attempts | ||||
| No | 35 (87.5%) | 18 (78.3%) | 0.93 | .334 |
| Yes | 5 (12.5%) | 5 (21.7%) | ||
| Previous hospitalizations | ||||
| No | 36 (90.0%) | 20 (87.0%) | χ2(1)= .14 | .711 |
| Yes | 4 (10.0%) | 3 (13.0%) | ||
| Psychiatric medication at intake | ||||
| No | 11 (27.5%) | 14 (60.9%) | χ2(1)=6.79 | .009 |
| Yes | 29 (72.5%) | 9 (39.1%) | ||
| Anxious comorbidity at intake | ||||
| No | 29 (72.5%) | 21 (91.3%) | χ2(1)= 3.15 | .076 |
| Yes | 11 (27.5%) | 2 (8.7%) | ||
1 Graffar is an international classification for socioeconomic status (SES; Graffar, 1956). The higher is the score, the lower the SES. This sample means indicate high SES.
Note. M=Mean; SD=Standard Deviation; GAF=Global Assessment of Functioning of the DSM-IV (First et al., 2002); BDI-II=Beck Depression Inventory II; OQ-45.2=Outcome Questionnaire 45.2; OQ-45.2 IR=Outcome Questionnaire 45.2 Interpersonal subscale; WAI-C=Working Alliance Inventory–client version.
Variables that are usually found to predict dropping out in the literature (e.g., low SES, low education, being female and therapeutic alliance) were not corroborated by our results. Assignment to treatment not predicting dropout is in line with findings in the literature (Swift & Greenberg, 2012), although it conflicts with the findings showing higher dropout rates in CBT therapies when compared to other therapies (e.g., Peñate Castro et al., 2014). These negative findings should be read with caution due to the small variance, restricting its generalization.
Consumption of medication at intake reduced the odds of dropping out from psychotherapy. Although clinicians and researchers agree that “the alleviation of symptoms with medication would reduce the motivation for gaining the understanding or making lifestyle changes needed to bring about a sustainable ‘cure”’ (Thase & Jindal, 2004, p. 743), they also recognize that pharmacotherapy is “a way to hasten recovery and to help patients make better use of psychotherapy” (p. 744). It appears that the alleviation of acute negative symptoms promoted by medication may have helped the clients adhering to psychotherapy and completing treatment. Also, the fact that medicated clients were assisted simultaneously by a psychiatrist and a psychologist may have decreased the odds of dropout.
The other prominent predictor for treatment dropout was not having a comorbid anxiety disorder or symptoms at intake. It can be suggested that anxiety symptoms would increase activity level and enhance motivation to complete the intervention. Since negative symptoms such as lack of activity and anhedonia characterize MDD, it is possible that depressed clients with no comorbid anxiety would have less motivation for completing treatment.
Results suggest that clinicians should pay extra attention to the clients not taking medication or with no comorbid anxiety, especially on the early stages of psychotherapy, when dropout is most likely to occur.
The Portuguese Foundation for Science and Technology (FCT) supported this paper through the Research Project “Ambivalence and Unsuccessful Psychotherapy” [PTDC/PSI-PCL/121525/2010], coordinated by M. Gonçalves, and a doctoral grant to R. Lopes [SFRH/BD/47343/2008]. The authors would like to thank the clients, therapists and staff at the Psychological Service at University of Minho, who have participated at the study in its diverse segments; Cátia Von Doellinger, who helped with data collection and with the statistical analysis; Dulce Pinto, who have reviewed the manuscript; Pablo Fernandez-Navarro for translating to Spanish; Maria Camera-Serrano and Paula Balbi for reviewing the Spanish version. An earlier version of this article was presented at the 42nd international meeting of the Society for Psychotherapy Research, held in Bern, Switzerland, in June 2011.
Available online 28 November 2014