Qualitative evidence points to the importance of both mental health-related barriers and benefits to exercise in chronic pain, yet this bidirectional relationship has not been established quantitatively.
Methods89 adults with chronic pain (75 female, Age: M = 34.7, SD=13.2), and 89 demographically-matched individuals without chronic pain (73 female, Age: M = 32.0, SD=13.3) self-reported demographic and health information, mental health-related barriers and benefits to exercise, and leisure-time exercise activity.
ResultsAdults with chronic pain had significantly higher scores on mental health-related barriers to exercise, and lower leisure-time exercise participation than adults without chronic pain. The groups did not differ on mental health-related benefits of exercise scores. Benefits scores positively predicted exercise, yet there was a significant negative interaction between pain and benefit scores, indicating a weaker positive relationship between benefits and exercise for adults with chronic pain than for those without chronic pain. Barrier scores significantly negatively predicted exercise engagement, but did not interact significantly with chronic pain.
ConclusionMental health-related barriers and benefits to exercise are important considerations when prescribing exercise for adults with chronic pain. Adults with chronic pain may require individualised support to address mental health-related barriers to leisure-time exercise.
Chronic pain disorders are highly common, affecting approximately 21 % of the population worldwide in any given year (Cieza et al., 2020). Chronic pain is defined as persistent pain lasting longer than 12 weeks, and can be due to specific pathophysiology (e.g., arthritic or rheumatic conditions, connective tissue disorders), or can be idiopathic, requiring patient report for diagnosis (e.g., fibromyalgia, chronic widespread pain, non-specific low back pain) (Ambrose & Golightly, 2015).
Exercise is the gold standard treatment for chronic pain, given its low cost, overall safety, and efficacy for treating pain (Geneen et al., 2017; Shipton, 2018). Exercise is here defined as effortful and planned movement or physical activity, completed in leisure-time, for either personal enjoyment or improved health outcomes (Caspersen et al., 1985). Despite the benefits of exercise for chronic pain, one large-scale study of 4839 individuals with chronic pain found that approximately 23 % of respondents felt unable to exercise, and a further 50 % felt less able to exercise since pain onset (Breivik et al., 2006). Thus, the uptake and adherence of exercise may prove difficult. But it is unclear whether it is solely pain which may inhibit exercise, or if co-occurring factors such as affective symptoms, including anxiety and depression also contribute.
Given the high comorbidity rates between chronic pain and depression and anxiety (Gureje et al., 2008a), treatment courses should address both physical and mental health presentations, including individual's perceived barriers and benefits to leisure time exercise. Mental health-related barriers and benefits to exercise are critical factors to evaluate, and are predictive of participation in leisure-time exercise activity (Connolly et al., 2023).
Evidence of mental health-related barriers and benefits to exercise in chronic pain is currently limited to qualitative research, where individuals with chronic pain have reported the mental health-specific benefits from leisure-time exercise of: improvements in self-confidence, overall motivation, enjoyment, improved sleep, and cognition, as well as decreases in exercise-related anxiety (Dnes et al., 2020; Joelsson et al., 2017; Vader et al., 2019). Mental health-related barriers reported by participants with chronic pain include low motivation, fear of injury or future pain (separate to current pain), low self-efficacy for exercise, fatigue, poor self-image, low mood, high anxiety, and perceived lack of exercise knowledge (Dnes et al., 2020; Joelsson et al., 2017; Vader et al., 2019). In the general population, scores of anxiety and depression-like symptoms positively predicted mental health-related barriers to exercise. Furthermore, leisure-time exercise participation was positively predicted by the benefits scores, and negatively predicted by the barriers scores [8]. However, the predictive patterns of mental health-related barriers and benefits to exercise for individuals with chronic pain are unclear.
We therefore aim to determine whether mental health-related barriers and benefits differentially predict leisure-time exercise participation between groups of individuals with chronic pain and those without. We hypothesise the following:
- 1.
Individuals with chronic pain will report higher levels of mental health-related barriers and lower levels of mental health-related benefits of exercise than those without chronic pain;
- 2.
The mental health-related barrier scores will negatively predict leisure-time exercise engagement more strongly for individuals with chronic pain than those without chronic pain;
- 3.
The mental health-related benefit scores will positively predict leisure-time exercise participation more strongly for individuals without chronic pain than for individuals with chronic pain.
The present dataset (total n = 178) comprises two groups: 1) a chronic pain group (n = 89), and 2) a demographically matched group of individuals without chronic pain (n = 89). The study was advertised via social media (Facebook, Twitter, Instagram and LinkedIn), online student noticeboards, and by email from physiotherapy and allied health clinics. The study was primarily advertised toward individuals residing in Australia, however, individuals residing overseas were also eligible. The recruitment of participants with chronic pain was completed first, allowing for follow-up advertisements to target particular age and gender demographics of individuals without chronic pain, for a balanced design. Overall sample size was determined by power analysis for a two-tailed student's t-tests with a conservative estimated effect size of d = 0.65, with p = .001 (see Giesecke et al., 2005 for comparison between chronic pain and healthy controls on depressive scores). The power analysis gave a minimum sample size of 85 participants per group. After the recruitment of 89 adults with chronic pain, a stopping point of 89 adults without chronic pain was implemented for recruitment.
Participants were eligible based on the following inclusion criteria: 1) aged 18–75; 2) no reported history of severe mental illness; 3) no physical disability that impacts > 50 % of daily function. The chronic pain sample had additional inclusion criteria of i) self-reported musculoskeletal pain lasting over 3 months. Individuals who reported pain for a period of less than 3 months were excluded. Demographic information is presented in Results.
ProcedureParticipants completed a short online questionnaire via the online survey management site Qualtrics to assess eligibility. Upon completion of the short survey, all participants were eligible to enter a draw for 1 of 5 gift card vouchers of $25AU. If eligible, participants were redirected to a second Qualtrics webpage, which contained a longer set of questionnaires to assess the psychological symptoms, pain, and exercise measures of interest. Upon completion of the total battery, participants were eligible to enter the draw for 1 of 10 gift card vouchers of $50AU.
MeasuresThe Mental health-related barriers and benefits to EXercise scale (MEX) (Connolly et al., 2023). The MEX is a 30-item scale (15 benefits of leisure-time exercise, 15 barriers to leisure-time exercise engagement) designed to assess the extent to which common transdiagnostic mental health symptoms can be alleviated with leisure-time exercise (benefits), and the extent to which such symptoms can hinder the practice of leisure-time exercise (barriers). A further two items were included in analysis: ‘benefit facilitation’ and ‘barrier interference’, in which participants were asked to rate the extent to which the benefits on the MEX scale facilitated exercise, and the barriers on the MEX scale interfered negatively with exercise.
Depression, Anxiety, and Stress Scales (DASS-42) (Lovibond & Lovibond, 1995). The DASS-42 is a 42-item scale designed to measure depression, anxiety and stress on a continuum (Lovibond & Lovibond, 1995). This measure was chosen due to its well-established psychometric properties (Page et al., 2007), and its utility in both research and clinical settings.
Subjective activity and fitness: Participants were presented with two questions regarding their evaluation of their current levels of physical activity (on a four-point scale of ‘I am very physically active’ to ‘I am not active at all’), and fitness (on a four-point scale of ‘I am very fit’ to ‘I am very unfit’). Participants were also asked a further two questions to ascertain an evaluation of self-comparisons with peers of their own age in terms of physical activity (on a five-point scale of ‘I am much more active than the average person’, to ‘I am much less active than the average person) and fitness (on a five-point scale of ‘I am much more fit than the average person’, to ‘I am much less fit than the average person). Questions on subjective activity and fitness were chosen as previous research indicates a negative association between mental health and subjective activity, where associations may not be present with mental health scores and recalled physical activity in metabolic equivalents (Baceviciene et al., 2019; Lang et al., 2019).
The McGill pain questionnaire - Short form (The MPQ-SF) (Melzack, 1975). The MPQ-SF is a 22-item questionnaire to assess the strength and type of pain. Perceptions of pain are described by 22 short descriptions (e.g., ‘throbbing pain’ or ‘aching pain’). The participant rates their current levels of each of the 22 pain types from 0 to 10, where 0 corresponds to no pain, and 10 corresponds to ‘worst possible pain’ (Melzack, 1975). This scale was selected due to its simplicity in administration, and its established psychometric properties.
The Habitual Physical Activity Questionnaire - Leisure-time Exercise Score (Baecke et al., 1982). The habitual physical activity questionnaire is a three-factor questionnaire designed to capture habitual physical activity across three domains: 1) activity at work, 2) sport and exercise activity in leisure time (referred to here as the Leisure-time Exercise Score), and 3) other leisure-time physical activity (e.g. incidental walking in leisure time, transport-related activity, and general inactivity). The present study uses only the second domain in analysis, deriving the leisure-time exercise score as an index of intentional leisure-time sport and exercise participation. Within the leisure-time sport and exercise component, the first question asked participants whether or not they participated in regular leisure-time sport or exercise. If ‘yes’, participants were then asked to list up to two activities which they participated in most frequently on a regular basis. The two activities could be either sports (e.g. tennis, football) and/or types of exercise (e.g. gym-based exercise, running, yoga). Participants were also asked for an estimation of their regular time spent participating in each activity, and the intensity of the activity. The resulting leisure-time sport and exercise index is scored from 0 to 4, where 0 corresponds to no leisure-time exercise participation, 1 corresponds to a low level of low-intensity activity in leisure time, and 4 corresponds to a high amount of high-intensity activity in leisure-time.
Pain Management and Exercise Prescription: Individuals with chronic pain were asked a single-item binary question of whether or not they take pharmaceutical medication for their pain. All participants were asked whether they had been prescribed exercise by a health professional in the previous three months; whether this prescription was specific or general, and which type of health professional prescribed their exercise(s) (e.g., physiotherapist, exercise physiologist, general practitioner). Examples of specific and general exercise prescriptions were given to participants. The examples of specific exercise prescriptions from healthcare providers were: "do 10 reps of squats for 3 sets, twice a week", "go for a walk for half an hour per day", or a full exercise routine to do a set number of times per week. The example given of a general exercise prescription from a healthcare provider was: "you should get some more exercise".
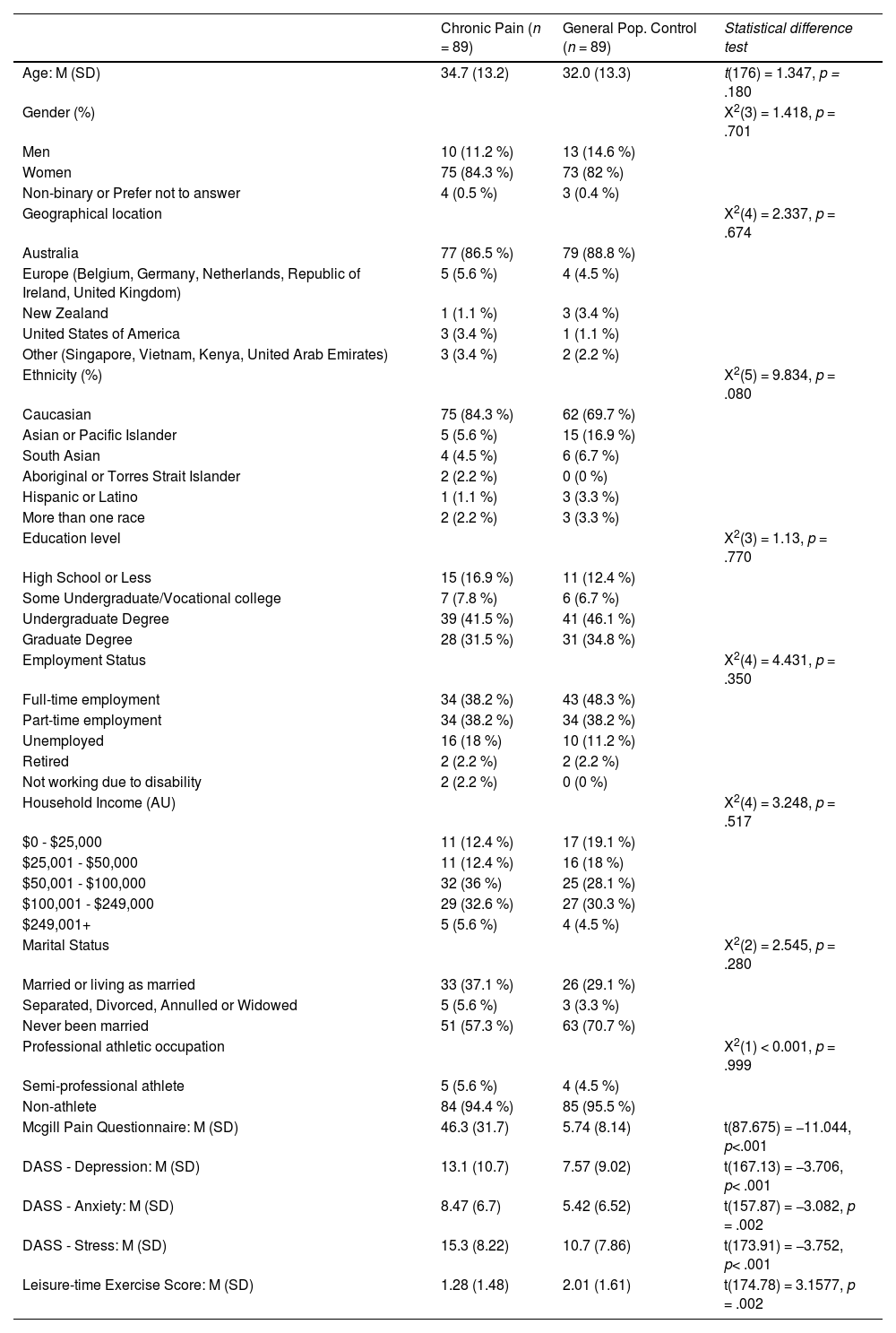
ResultsDemographicsThere were no significant differences between groups at the a = 0.05 level on any of the collected demographic information. All descriptive statistics and group difference calculations are shown below in Table 1.
Descriptive statistics for the chronic pain and general population control groups.
AU= Australian dollar; M = Mean; SD = Standard deviation; DASS = Depression, Anxiety and Stress Score.
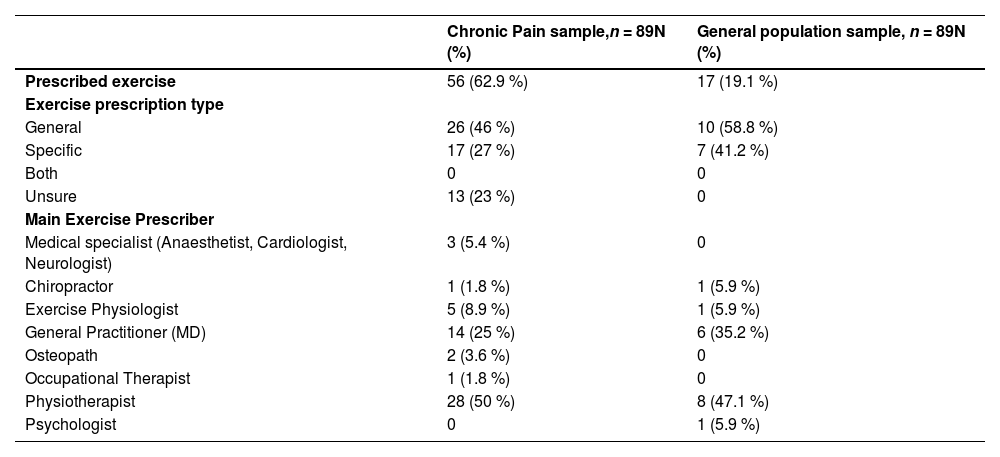
Additional information was collected regarding chronic pain characteristics for the chronic pain sample and are presented in Appendix A: Table A1, including self-reported diagnoses. Information about exercise prescriptions for both samples was also collected and presented in Appendix A: Table A2. Participants’ self-reported diagnoses were also recategorized by the authors in terms of the International Classification of Diseases - 11 (ICD-11) categories of chronic pain diagnoses (Treede et al., 2015), as reported in Appendix A: Table A1.
Group differences on affect, pain, exercise and activity levels, and mental health-related barriers and benefits to exerciseThe differences between the groups on all experimental measures can be seen below in Table 2. Significance was adjusted for multiple comparisons; the Bonferroni-corrected value of p = .005 was determined equivalent to nominal a = 0.05. Although some heterogeneity of variance was observed on MPQ scores, t-tests are typically robust to such assumption violations when sample sizes are equal between groups (Rasch, Teuscher & Guiard, 2007). Differences were observed between groups on mental health-related barriers to exercise, the amount to which endorsed mental health-related barriers interfered with exercise (barrier interference), pain, depression, anxiety, stress, and leisure-time exercise scores. However, there was no statistically significant difference between groups on subjective activity scores, mental health-related benefits to exercise, nor the amount to which the endorsed mental health-related benefits facilitated exercise (benefit facilitation).
Group differences between the chronic pain group and general population group on continuous variables.
Note. CP = chronic pain sample; GP = general population control sample; MEX = Mental health-related barriers and benefits to EXercise scale; MPQ = Mcgill Pain Questionnaire; DASS = Depression, Anxiety and Stress Scale.
Results significant to the Bonferroni-corrected p < 0.005 level are bolded.
Descriptive data showed the emergence of several subgroupings within the chronic pain sample: i) the number of sites of pain on the body (single-site: n = 21, two-site: n = 22, or 3+, n = 46); ii) whether or not participants were prescribed exercise by a health professional (yes: n = 56, no: n = 33); iii) the specificity of the exercise prescription (general: n = 26; specific: n = 17); iv) whether or not participants were prescribed pain management pharmaceuticals by a health professional (yes: n = 33; no: n = 56). Mean differences were compared between the binary subgroupings of the chronic pain sample, on the key variables of MEX - benefits, MEX - barriers, the MPQ, DASS - depression, DASS - anxiety, DASS - stress, leisure-time exercise scores, and subjective activity. Spearman's rank-ordered correlation was used to analyse the association between the number of pain sites and the key variables, due to the nature of the ordinal data. Per the large number of analyses, significance for each of the 24 t-tests was considered at the bonferroni-corrected value of p<.002.
The number of pain sites was not significantly correlated with any of MEX - benefits, MEX - barriers, the MPQ, DASS - depression, DASS - anxiety, DASS - stress, leisure-time exercise scores, and subjective activity. Further, there were no significant differences at the a = 0.01 level on any of the key variable outcomes between any of the three binary indicator groupings (1. Whether or not exercise was prescribed; 2. type of exercise prescription: general or specific; 3. Whether or not pain management pharmaceuticals were prescribed). A table of chronic pain-specific analysis results is presented in Appendix B, Table B1.
Additionally, participants with chronic pain were further grouped based on the International Classification of Diseases (ICD) of the World Health Organization (WHO), the ICD-11 chronic pain diagnostic nomenclature (Treede et al., 2015). Of the 89 total participants with chronic pain, 76 participants had chronic pain diagnoses which were categorised under only one of the following parent chronic pain entities: musculoskeletal (n = 36), neurological (n = 2), primary (n = 22), post-surgical or post-traumatic (n = 10), or visceral (n = 6). The other 13 participants had diagnoses with multiple parent entities: i) musculoskeletal and post-surgical or post-traumatic (n = 5), ii) musculoskeletal and neurological (n = 2), iii) musculoskeletal and head (n = 2), iv) musculoskeletal and visceral (n = 1), v) neurological and head (n = 1), vi) primary and head (n = 3), and vii) post-traumatic and visceral (n = 1). Eight separate One-way Analyses of Variance (ANOVAs) were performed using the ICD-11 based chronic pain groupings (excluding the neurological chronic pain group due to the small sample size of n = 2) on each of the key outcome variables of MEX - benefits, MEX - barriers, the MPQ, DASS - depression, DASS - anxiety, DASS - stress, leisure-time exercise scores, and subjective activity. No significant differences were found across ICD-11 chronic pain type groups on any of the eight variables. A table of ICD-11 chronic pain type ANOVA results, along with the means and standard deviations for each group on each key variable, is presented in Appendix B, Table B2.
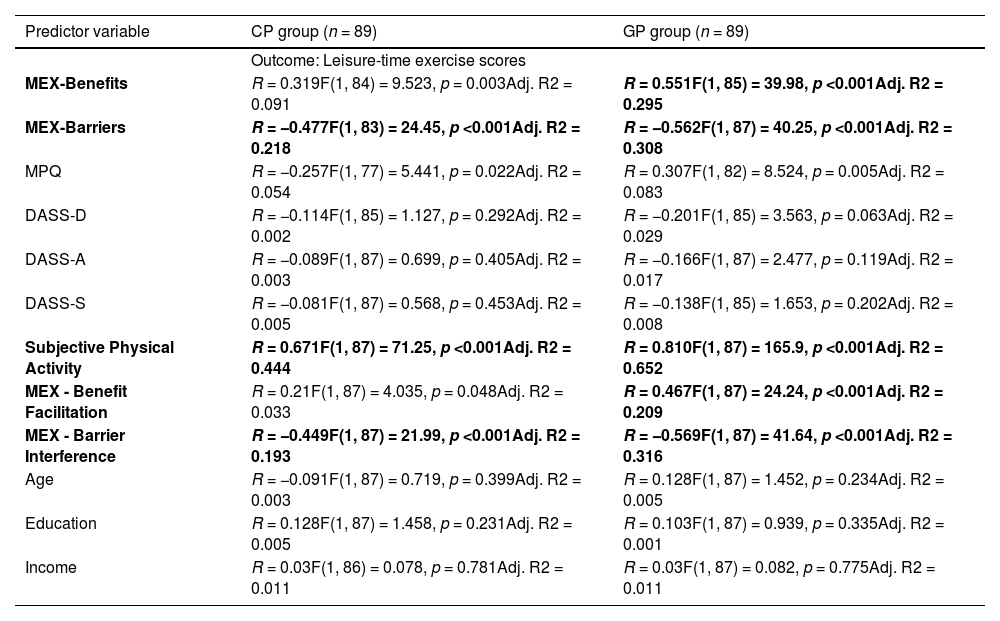
Linear regression models predicting reported leisure-time exercise participationTo specify which variables from the collected data were significant predictors of leisure-time exercise for each sample, simple regression analyses were conducted with each continuous variable as single predictors separately for the chronic pain and the general population group (see Table 3). Simple regression analyses were completed using variables theorised to either predict or be covariates of leisure-time exercise, in light of the significant difference in leisure-time exercise scores between groups. The simple regression analyses were conducted to allow for clearer comparison with multiple regression analyses to follow. Due to the large number of analyses, significance for each of the 24 simple regression models was considered at the bonferroni-corrected value of p< .002. Leisure-time exercise scores were significantly predicted by the following variables in both samples: MEX - mental health-related barriers to engagement, Subjective Activity and Fitness Scores, and MEX - interference of barriers on exercise. Although the variables MEX - benefits and MEX - facilitation of MEX benefits on exercise were both significant predictors of leisure-time exercise for the general population control sample, they were not significant predictors of leisure-time exercise for the chronic pain sample. The following variables were not significant predictors of leisure-time exercise scores in simple regression in neither the chronic pain nor the general population control samples: MPQ - total current pain scores, DASS - Depression, DASS - Anxiety, DASS - Stress, age, education levels, nor income levels.
Simple regression analyses, predicting leisure time exercise from relevant predictor variables, by chronic pain grouping.
Note. CP = chronic pain sample; GP = general population sample; MEX = Mental health-related barriers and benefits to EXercise scale; MPQ = Mcgill Pain Questionnaire; DASS = Depression, Anxiety and Stress Scale.
Results significant to the Bonferroni-corrected value of p < 0.002 level are bolded.
Forward entry stepwise multiple regression analyses were performed including the entire sample (n = 188), but using the chronic pain grouping as a secondary independent variable, to account for any interaction effects between the mental health-related benefits and experience of chronic pain in the prediction of leisure-time exercise scores in model 1, or between the mental health-related barriers and chronic pain in the prediction of leisure-time exercise scores in model 2. Results of the best fitting models for predicting leisure-time exercise scores from benefits, group, and the interaction of benefits and group are presented below in Table 4, as Model 1. Model 1 was significant overall, and included a significant negative interaction between the benefits score and group, with the benefits score as a significant positive predictor within the model. However, group alone was not statistically significant as a predictor of leisure-time exercise scores within the model. The results from the model predicting leisure-time exercise scores from barriers and chronic pain with an interaction term are presented below in Table 4, as Model 2. Model 2 was significant overall, however, only the barriers score was significant as a predictor of leisure-time exercise scores within this model. Group was not a significant predictor of leisure-time exercise scores within this model, nor was the interaction term between pain grouping and barrier scores. In both model 1 and model 2, backwards entry stepwise regression was also undertaken to ensure the models chosen were best fitting for the data. Both models 1 and 2 (as described in Table 4) had better fit and accounted for higher levels of overall model variance than the comparative alternate models without interaction effects and without pain grouping as a predictor.
Models of prediction of leisure-time exercise by mental health-related benefits, mental health-related barriers, and chronic pain vs. non-chronic pain sample.
Note: results and terms significant to the p < 0.05 level are bolded. Non-chronic pain group used as reference group for calculation.
Figs. 1a and b depict the benefits and barrier models with group respectively.
Panel A) Model 1: Linear trend lines of the effect of Mental health-related benefits to exercise on leisure-time exercise scores, with a significant group interaction. Panel B) Model 2: Linear trend lines of the effect of Mental health-related barriers to exercise on leisure-time exercise scores, with a non-significant group interaction.
The current study aimed to quantify differences between individuals reporting chronic pain to a demographically-matched sample of those without chronic pain on mental health-related barriers and benefits to leisure time exercise. Individuals with chronic pain reported significantly higher levels of perceived mental health-related barriers to leisure time exercise than those without chronic pain. Those with chronic pain also reported higher interference from the mental health-related barriers for leisure time exercise than those without chronic pain. There was, however, no significant difference between the groups on perceived mental health-related benefits to exercise or perceived facilitation of exercise from the mental health-related benefits to exercise. Additionally, and in line with previous quantitative evidence (Gureje et al., 2008b), the individuals with chronic pain reported higher anxiety-like, depression-like symptoms, and self reported stress levels, and lower scores on leisure-time exercise participation as well as subjective activity levels, compared to individuals without chronic pain.
Interestingly, individuals with chronic pain reported similarly high levels of mental health-related benefits to exercise as those without chronic pain. Yet, a multiple regression model showed that mental health-related benefits more strongly predicted exercise participation for those without chronic pain than for those with chronic pain. Thus, seemingly, unique aspects of the chronic pain experience may include barriers to exercise that may supersede the experience of mental health-related benefits to exercise. This finding corresponds to evidence from qualitative research, showing that although individuals with chronic pain may understand and recognize the benefits of exercise - both for their chronic pain condition and for their mental health - participating in exercise remains challenging due to barriers to exercise such as fear of pain with movement, lack of motivation and lack of support and access (Vader et al., 2019). Accordingly, in another multiple regression model from our dataset, there was no interaction between chronic pain and barriers to exercise in the prediction of exercise participation, with results for both groups indicating that the more mental health-related barriers reported by participants, the lower the rate of exercise participation. Yet, importantly, in this cross-sectional analysis the individuals with chronic pain had significantly higher levels of mental health-related barriers than those without chronic pain. Thus, the implications of both mental health-related benefits and mental health-related barriers to exercise for individuals with chronic pain may be essential to review clinically in the prescription of exercise treatment and rehabilitation.
For clinical settings, the findings of the current study suggest that psychoeducation surrounding the mental health-related benefits of exercise is valuable where appropriate to increase exercise motivation, and remains a viable option for individuals with and without chronic pain. Given the delicate interplay between chronic pain and mental health barriers and benefits to exercise, the results of the present study support the notion of a holistic approach to pain management. Present results indicate that physical therapists and exercise professionals involved in the rehabilitation of chronic pain should be psychologically informed of the increased level of mental health-related barriers to exercise in chronic pain, and the potentially decreased influence of mental health-related benefits to exercise in chronic pain. The contemporary pain clinic model, which includes pain and exercise specialists, as well as clinical psychologists (Bell, 2015), also has the possibility to provide holistic care with recognition of the mental health-related barriers to exercise for individuals with chronic pain, and to support clients individually to overcome such barriers, and identify meaningful and individualised benefits. Indeed, future clinical trials will be necessary for investigating the ongoing role of barriers and benefits to exercise in chronic pain rehabilitation.
The primary strength of this study is that this is the first study to quantitatively model the mental health-related barriers and benefits to exercise in individuals with chronic pain and compare these barriers and benefits to individuals without chronic pain. The present study adds to an existing body of qualitative research on barriers and benefits to exercise in chronic pain (Dnes et al., 2020; Joelsson et al., 2017; Vader et al., 2019) by using quantitative methods to predict exercise participation from mental health-related barriers and benefits to exercise in individuals with and without chronic pain. Furthermore, using a validated mental health-related barriers and benefits scale lends credence to the generalizability of results, and allows for further replicability (Connolly et al., 2023).
The present study has limitations which warrant consideration. Firstly and most importantly, the study focused solely on mental health-related barriers and benefits to leisure time exercise. Whilst the area of mental health-related barriers and benefits to exercise is particularly understudied, the narrowed scope of the present research may have missed quantifying other important benefits and barriers to exercise that may be unique to the experience of chronic pain, for example, lack of social support, or lack of access to facilities (Vader et al., 2019). Secondly, the sampling of two groups of only 89 participants each limited statistical power when modelling covariates in the prediction of leisure-time exercise participation. Further, the final two models chosen to represent the data were optimised to each only include two predictor variables (i. Group, and ii. either the mental health-related benefits or barriers to exercise) and an interaction term each, to allow for increased statistical power. Future research in this area with larger sample sizes may seek to increase explanatory power by using further predictor variables to account for the complexities of the pain-affect-exercise relationship. The small sample size also potentially limited statistical power in analysing differences in experimental outcomes by subgroups of chronic pain participants based on pain-specific characteristics (e.g., ICD-11 chronic pain subtypes, prescriptions of exercise or pain medication). It remains unclear from the present analysis whether null results found on all experimental outcomes by all chronic pain subgroups simply reflect overall commonalities across chronic pain characteristics, or if such results are due to the small sample sizes occurring as a function of subgrouping only 89 participants on various characteristics. The nature of the study design using convenience sampling does unfortunately limit interpretation of results also. Future research may benefit from clinical recruitment for adults with chronic pain. Finally, comparison was limited to a cross-sectional design of individuals with chronic pain diagnoses and to individuals without chronic pain in the general population, thus potential differential levels, effects, and determinants of mental health-related barriers and benefits to exercise between chronic pain and clinical anxiety or depression are yet to be established.
The present study has provided evidence of differences between individuals with chronic pain and those without in terms of their mental health-related barriers and benefits to leisure time exercise, and potential implications for leisure-time exercise participation. The relationship between benefits and exercise was stronger for the individuals without chronic pain than for those with chronic pain, and higher levels of barriers were reported by individuals with chronic pain compared to individuals without chronic pain. Identifying and addressing the mental health-related barriers and benefits to exercise in chronic pain may be critical in the successful prescription of exercise for individuals with chronic pain.
Pain and treatment information for participants with chronic pain.
Note. * 28 participants of 89 with chronic pain reported multiple chronic pain diagnoses.
Exercise prescription information for both groups.
Subgroups within the chronic pain sample (number of pain sites, and prescription of exercise and pain medication), compared on outcome scores of mental health-related benefits and barriers, pain, depression, anxiety, stress, exercise, and subjective activity.
Note. MEX = Mental health-related barriers and benefits to EXercise scale; MPQ = Mcgill Pain Questionnaire; DASS = Depression, Anxiety and Stress Scale. Significance considered at Bonferroni corrected value of p < .002. *Item not used in analysis.
Chronic pain subtypes per the ICD-11 pain categories within the Chronic Pain sample, compared on the outcome scores of mental health-related benefits and barriers, pain, depression, anxiety, stress, exercise, and subjective activity.
Note. MEX = Mental health-related barriers and benefits to EXercise scale; MPQ = Mcgill Pain Questionnaire; DASS = Depression, Anxiety and Stress Scale.
*Neuropathic chronic pain group not included in analyses due to small sample size.
Funding acknowledgment: This research was financially supported by the Melbourne School of Psychological Sciences at the University of Melbourne. We declare no conflicts of interest.