Clinical Networks are complex interventions that enable healthcare professionals from various disciplines to work in a coordinated manner in the context of multiple care settings, to provide a high quality response to a specific disease. The aim of this study was to evaluate if clinical networks are able to improve effectiveness, efficiency, patients’ satisfaction and professionals’ behavior in the health care settings, namely the “quadruple aim” quality goals.
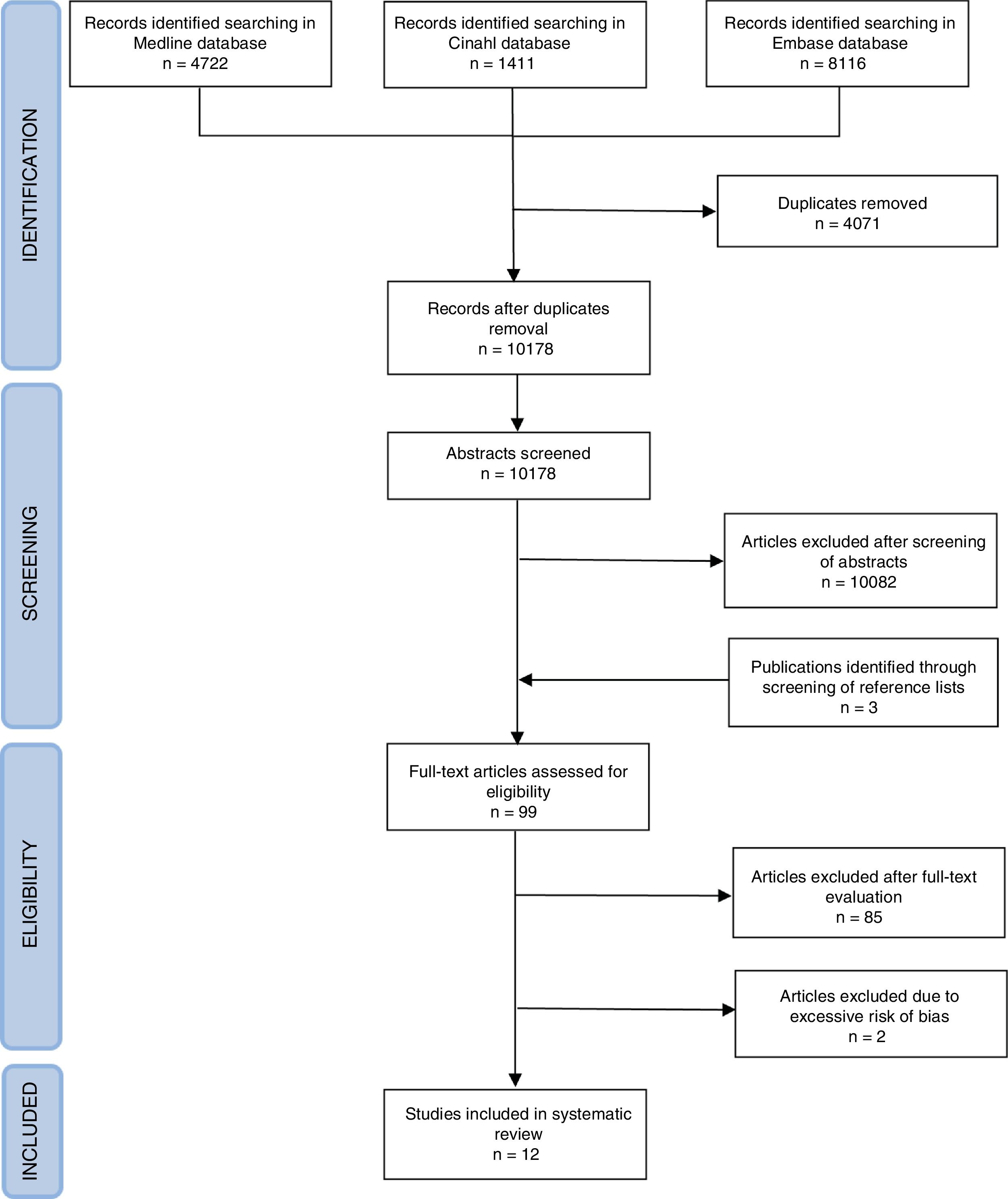
Materials and methodsA systematic review of documents published until February 28, 2018, in Medline, Embase and CINAHL was performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses approach. A specific research strategy was created to identify studies evaluating effectiveness, efficiency, patient satisfaction and professionals well-being obtained through clinical networks implementation.
Results14249 studies were identified; 12 of these were eligible to the evaluation of “Quadruple Aim” outcomes. 9 studies focused on patients’ outcomes improvement and 4 on network efficiency. Professionals’ and patients’ experience were not considered in any study.
ConclusionsThere are some evidences that clinical network can improve patients’ outcomes and health funds allocation in a small number of moderate-low quality studies. Further rigorous studies are needed to confirm these findings and to evaluate patients’ and professionals’ experience, taking into account also networks’ structural features that could influence outcomes achievement.
Las redes clínicas son intervenciones complejas que permiten a los profesionales de la salud de diversas disciplinas trabajar de manera coordinada en el contexto de entornos de atención múltiple, para brindar una respuesta de alta calidad a una enfermedad específica. El objetivo de este estudio fue evaluar si las redes clínicas pueden mejorar la efectividad, la eficiencia, la satisfacción de los pacientes y el comportamiento de los profesionales en el ámbito de la atención médica, es decir, el denominado cuádruple objetivo de calidad.
Materiales y métodosSe realizó una revisión sistemática de los documentos publicados hasta el 28 de febrero de 2018 en Medline, Embase y CINAHL mediante el uso de los elementos de informe preferidos para revisiones sistemáticas y metaanálisis. Se creó una estrategia de investigación específica para identificar estudios que evalúen la efectividad, la eficiencia, la satisfacción del paciente y el bienestar de los profesionales obtenidos a través de la implementación de redes clínicas.
ResultadosSe identificaron 14.249 estudios; 12 de ellos fueron elegibles para la evaluación de los resultados de cuádruple objetivo. Nueve estudios se centraron en la mejora de los resultados de los pacientes y 4 en la eficiencia de la red. La experiencia de los profesionales y los pacientes no se consideró en ningún estudio.
ConclusionesExisten algunas evidencias de que las redes clínicas pueden mejorar los resultados de los pacientes y la asignación de fondos de salud en un pequeño número de estudios de calidad moderada a baja. Se necesitan más estudios rigurosos para confirmar estos hallazgos, y evaluar la experiencia de los pacientes y profesionales, teniendo en cuenta también las características estructurales de las redes que podrían influir en el logro de los resultados.
Clinical Networks are complex organizational systems that enable healthcare professionals from various disciplines to work in a coordinated manner in the context of multiple care settings, unconstrained by existing professional and organizational boundaries.1,2
Clinical networks are expected to provide a continuous and high quality response to a specific disease (for example cancer, stroke, respiratory diseases),3 taking into account clinical outcomes and satisfaction of all stakeholders.4–7 Networks should therefore be able to optimizing health system performance.
Actually, the most challenging framework to evaluate quality produced by health care systems is the Quadruple Aim approach.8 Dimensions of performance that must be evaluated according to this framework are: improving the health of populations, reducing the per capita cost, enhancing the patient experience of care, and improving the work life of health care clinicians and staff.
Since 1999, several forms of clinical networks,9 with different formalization levels, governance methods and strength of linking between member centers, have been established in Europe,10–13 Australia,6 America.14,15 Due to huge financial investments required to implement this organizational model,16 an evaluation of quality outcomes is needed to a proper allocation of resources.
The aim of this systematic review is to evaluate the quality of care produced by the more structured network models according to the Quadruple Aim framework,8 evaluating clinical outcomes (effectiveness), financial aspects (efficiency), and the experience of patients and professionals.
Materials and methodsThe review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) approach, to ensure transparency of methods and completeness of results reporting.17 A specific P.I.C.O.S. was created to direct the bibliographic research and properly identify the eligibility criteria to satisfy the research question.18
Eligibility criteria- -
Population: all patient with acute or chronic condition that can be treated by health care system.
- -
Intervention: implementation of one of the following types of clinical network: “Managed Clinical Network (MCN)” (groups of healthcare professional working in multi-professional and multidisciplinary teams organized by clinical discipline, with formal membership, hierarchical organization and mixed approach bottom-up/top-down), or “Integrated Service Delivery (ISD)” (networks made up of healthcare organizations with an overarching administrative structure aimed at integration and coordination of services, organized by geographical regions, with contractual arrangements about service delivery, hierarchical structure and top-down approach).9
- -
Comparison of quality outcomes before and after the network implementation or between comparable geographical areas with different network implementation degrees.
- -
Outcomes and proxy indicators of effectiveness, efficiency, patient satisfaction and healthcare professionals well-being as a result of clinical network implementation.
- -
Study design: quantitative studies were evaluated eligible for inclusion in the systematic review, such as experimental (Randomized Controlled Trials – RCT), quasi-experimental (Interrupted Time Series – ITS), and observational studies (before–after, with or without control group, cross-sectional, case-control, cohort studies).
Identification of articles was conducted in two stages by searching in electronic databases Medline, Embase and CINAHL, using a specific research strategy (Appendix A. Supplementary data [Attachment A. Research strategy]), and by snowballing, without restriction of language nor of publication date. A first research was conducted until February 06, 2017, and an update was performed to identify articles published until February 28, 2018. Unpublished articles were not searched.
After duplicates removal, articles were divided equally between the three reviewers and a first screening was conducted by title and abstract reading to assess the compliance with P.I.C.O.S. criteria. In case of doubt of a reviewer, the other two reviewers were asked to reach a shared decision. Studies evaluated as eligible were read entirely and independently by two reviewers to establish if they can be included in the qualitative analysis. To be included in the analysis, studies had to quantitatively compare the Quadruple Aim's outcomes obtained with and without the implementation of a MCN or an ISD. The choice of include studies in the qualitative analysis and the infeasibility of a meta-analysis was established in agreement by the reviewers. An ad hoc table was built to collect data, and the compilation method was initially tested in a coordinated manner by the reviewers, in order to obtain a standardized compilation procedure.
Quality assessmentStudies were included in the qualitative analysis after methodological quality evaluation. The evaluation was carried out through the application of the Newcastle-Ottawa Scale (NOS)19 for cohort studies, CASP (Critical Appraisal Skills Program) scale20 for case-control studies, Cochrane EPOC (Effective Practice and Organization of Care) criteria21 for Controlled Before–After studies (CBA), ITS and RCT, and the scales developed by the National Institutes of Health (NIH)22 for before–after studies without control group and for cross-sectional studies. Case-control, cross-sectional and before–after studies without control group were evaluated having a moderate or low quality depending on the satisfaction of more or less than the 50% of the checklist's items. Only for CBA, ITS and RCT, it was considered the possibility to reach a good quality degree if all the requested items were satisfied; quality was considered moderate if were met more than 50% of the criteria, or low if the study was missing more than 50% of the requested items. Cohort studies’ quality degree were evaluated according to NOS guidelines (the good quality degree could be assigned if were satisfied at least three requirements of the “selection” domain, one in the “comparison” domain and two in the “outcome/exposure” domain) (Appendix A. Supplementary data [Attachment B. Methodological quality assessment of the included studies]).
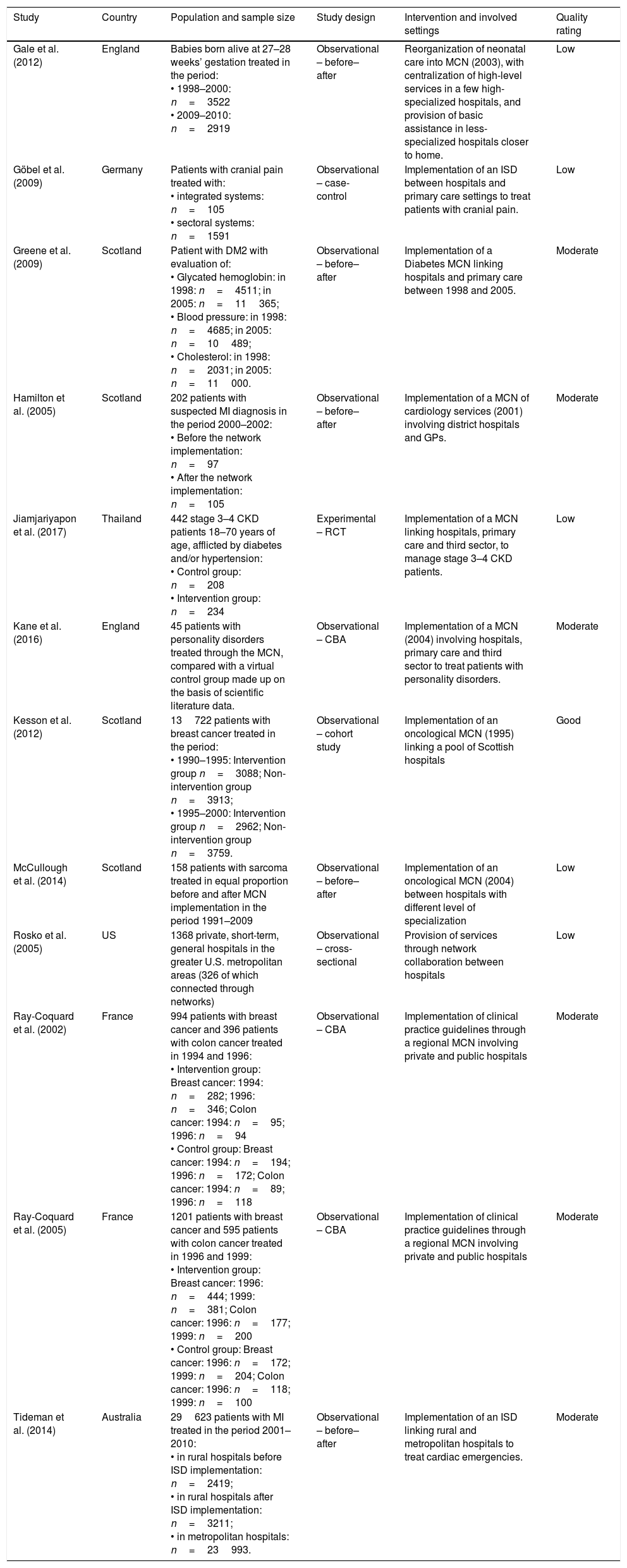
Results12090 studies were identified in the first search, and 2159 additional articles during the search update. After duplicates removal, 10178 studies were screened for eligibility. The research strategy of this review was created to maximize the sensitivity of the research, so most of the studies were excluded in the screening phase after abstracts reading, because of no adherence of the studies with the P.I.C.O.S. criteria. The main reasons for excluding studies were the following: qualitative studies, studies that analyzed typologies of networks less structured of MCN and ISD, studies that were not focused on clinical networks but rather on multidisciplinary teams or clinical pathway. After the screening of abstracts, 99 studies were selected and analyzed in full. Bibliography evaluation led to the inclusion of 3 further studies, also analyzed in full. Only 12 of these studies were eligible to the “Quadruple Aim” outcomes evaluation (Fig. 1). The remaining articles were excluded due to impossibility to retrieve full text (some of the studies identified were abstracts presented at conference, which had not been followed by an in-extenso publication), absence of quantitative data, or no relevance with the aims of the study. Some studies were excluded because they were conducted on networks that did not have the features of MCN or ISD, or because they analyzed outcomes of interventions and projects in a network context and not the outcomes of the network implementation itself, or because they compared outcomes of health facilities organized in network against those of facilities without such organization despite the different severity of the treated patients or the differences between the institutions’ performances at the baseline. Furthermore, two quantitative studies were excluded due to their low quality which made unreliable their results. Characteristics and risk of bias of included studies are reported in Table 1.
Characteristics and risk of bias of included studies.
| Study | Country | Population and sample size | Study design | Intervention and involved settings | Quality rating |
|---|---|---|---|---|---|
| Gale et al. (2012) | England | Babies born alive at 27–28 weeks’ gestation treated in the period: • 1998–2000: n=3522 • 2009–2010: n=2919 | Observational – before–after | Reorganization of neonatal care into MCN (2003), with centralization of high-level services in a few high-specialized hospitals, and provision of basic assistance in less-specialized hospitals closer to home. | Low |
| Göbel et al. (2009) | Germany | Patients with cranial pain treated with: • integrated systems: n=105 • sectoral systems: n=1591 | Observational – case-control | Implementation of an ISD between hospitals and primary care settings to treat patients with cranial pain. | Low |
| Greene et al. (2009) | Scotland | Patient with DM2 with evaluation of: • Glycated hemoglobin: in 1998: n=4511; in 2005: n=11365; • Blood pressure: in 1998: n=4685; in 2005: n=10489; • Cholesterol: in 1998: n=2031; in 2005: n=11000. | Observational – before–after | Implementation of a Diabetes MCN linking hospitals and primary care between 1998 and 2005. | Moderate |
| Hamilton et al. (2005) | Scotland | 202 patients with suspected MI diagnosis in the period 2000–2002: • Before the network implementation: n=97 • After the network implementation: n=105 | Observational – before–after | Implementation of a MCN of cardiology services (2001) involving district hospitals and GPs. | Moderate |
| Jiamjariyapon et al. (2017) | Thailand | 442 stage 3–4 CKD patients 18–70 years of age, afflicted by diabetes and/or hypertension: • Control group: n=208 • Intervention group: n=234 | Experimental – RCT | Implementation of a MCN linking hospitals, primary care and third sector, to manage stage 3–4 CKD patients. | Low |
| Kane et al. (2016) | England | 45 patients with personality disorders treated through the MCN, compared with a virtual control group made up on the basis of scientific literature data. | Observational – CBA | Implementation of a MCN (2004) involving hospitals, primary care and third sector to treat patients with personality disorders. | Moderate |
| Kesson et al. (2012) | Scotland | 13722 patients with breast cancer treated in the period: • 1990–1995: Intervention group n=3088; Non-intervention group n=3913; • 1995–2000: Intervention group n=2962; Non-intervention group n=3759. | Observational – cohort study | Implementation of an oncological MCN (1995) linking a pool of Scottish hospitals | Good |
| McCullough et al. (2014) | Scotland | 158 patients with sarcoma treated in equal proportion before and after MCN implementation in the period 1991–2009 | Observational – before–after | Implementation of an oncological MCN (2004) between hospitals with different level of specialization | Low |
| Rosko et al. (2005) | US | 1368 private, short-term, general hospitals in the greater U.S. metropolitan areas (326 of which connected through networks) | Observational – cross-sectional | Provision of services through network collaboration between hospitals | Low |
| Ray-Coquard et al. (2002) | France | 994 patients with breast cancer and 396 patients with colon cancer treated in 1994 and 1996: • Intervention group: Breast cancer: 1994: n=282; 1996: n=346; Colon cancer: 1994: n=95; 1996: n=94 • Control group: Breast cancer: 1994: n=194; 1996: n=172; Colon cancer: 1994: n=89; 1996: n=118 | Observational – CBA | Implementation of clinical practice guidelines through a regional MCN involving private and public hospitals | Moderate |
| Ray-Coquard et al. (2005) | France | 1201 patients with breast cancer and 595 patients with colon cancer treated in 1996 and 1999: • Intervention group: Breast cancer: 1996: n=444; 1999: n=381; Colon cancer: 1996: n=177; 1999: n=200 • Control group: Breast cancer: 1996: n=172; 1999: n=204; Colon cancer: 1996: n=118; 1999: n=100 | Observational – CBA | Implementation of clinical practice guidelines through a regional MCN involving private and public hospitals | Moderate |
| Tideman et al. (2014) | Australia | 29623 patients with MI treated in the period 2001–2010: • in rural hospitals before ISD implementation: n=2419; • in rural hospitals after ISD implementation: n=3211; • in metropolitan hospitals: n=23993. | Observational – before–after | Implementation of an ISD linking rural and metropolitan hospitals to treat cardiac emergencies. | Moderate |
Abbreviations: MCN: Managed Clinical Network; ISD: Integrated Service Delivery; DM2: Type 2 Diabetes Mellitus; MI: Myocardial Infarction; GPs: General Practioners; CKD: chronic kidney disease; RCT: Randomized Controlled Trial; CBA: controlled before–after.
Outcomes of a neonatal care network were evaluated in a before–after study conducted in England.11 The study is based on data collected from British hospitals before and after the reorganization of neonatal care into MCN, which took place in 2003. Hospitals were differentiated depending on complexity levels, with centralization of high-level services in a few high-specialized centers, and provision of basic assistance in less-specialized centers closer to home. Data of babies born alive at 27–28 weeks’ gestation over the two years period September 1998 to August 2000 were compared with data of patients of the same gestational age born in the two year period 2009–2010. In the period 2009–2010, the 28-day survival was 94%, compared to 88% in the period 1998–2000 (OR=2.00; 95%CI: 1.67–2.40; p<0.001).
Diabetes care networkOutcomes of a diabetes network were analyzed in a Scottish before–after study.23 Diabetes MCN was progressively implemented between 1998 and 2005. The study compared clinical data referring to 1998, before the establishment of the network, with those of 2005, when the process was completed. Data showed a better, statistically significant, disease control in patient afflicted by type 2 diabetes after the network implementation. Patients with glycated hemoglobin ≤7% increased from 42.9% to 48.5%, and cholesterol was more effectively maintained ≤5mmol/l after the network establishment (72.8% of patients, compared to 30.7% in 1998). There was also a better control of blood pressure (BP): systolic BP≤140mmHg in 57.7% and diastolic BP≤80mmHg in 68.8% of patients (versus 50.7% and 57.8%, respectively, before the network implementation).
Cancer care networkAssessment of outcomes achieved with implementation of networks for the management of cancer has been identified in two studies carried out in Scotland: a cohort study conducted on 13722 patients with breast cancer24 and a before–after study conducted on patients with sarcoma,25 and in two CBA studies conducted in France on patient with breast cancer and colon cancer.12,26
The first study24 examined outcomes of breast cancer patients in a pool of Scottish hospitals in the period 1990–2000. In 1995 a cancer MCN was set up linking some of these hospitals, while in another group of hospitals the program was not implemented. After the network implementation, breast cancer specific mortality in the intervention area decreased compared to that recorded in the non-intervention area (Adjusted Hazard Ratio 0.82; 95%CI: 0.74–0.91; p<0.001), although the situation was reversed in the two areas before 1995 (Adjusted Hazard Ratio 1.11; 95%CI: 1.00–1.20; p=0.04). All-cause mortality followed the same trend (Adjusted Hazard Ratio 0.89; 95%CI: 0.82–0.97; p=0.005).
The second study25 was conducted on 158 patients with sarcomas, treated, in equal proportions, before and after the network implementation, which took place in 2004. The MCN take advantage of few specialized centers providing a high level support to the other cancer centers in the area, also using telemedicine. Analyzed aspects were representative of the care process, rather than its outcome, so they can be considered proxy indicators of the network effectiveness. The study showed a reduction in the average time interval from receipt of a referral to initial assessment by the service (10 days after the network establishment, compared with 19.5 days before its institution, p=0.016). There was also a statistically significant greater appropriateness both in the diagnostic phase (86% of patients undergoing Magnetic Resonance scanning before resection and 79% of patients undergoing biopsy, compared respectively to 67% and 57% in the past) that in the therapeutic phase (adequacy of surgical margins in 81% of patients, instead of 48% as it was before the network establishment).
Proxy indicators of network effectiveness were analyzed in the two CBA studies carried out in France.12,26 A comparison of compliance with clinical practice guidelines was performed between oncological services offered in a region where hospitals were organized in MCN and in a region where clinical networks were not implemented. Where services were organized in clinical networks, an increasing adherence to clinical guidelines was detected (from 12% in 1994 to 36% in 1996 (p<0.001) in breast cancer care) and this virtuous behavior was also maintained some years later (14% in 1994, 46% in 1996, 73% in 1999 in colon cancer care). Furthermore, in the region where the clinical network was implemented, conformity to medical practice guidelines was better than that registered in the region without a network organization of cancer services (adherence to guidelines in breast cancer care: 36% and 7%, respectively).
Cardiovascular networkOutcomes obtained through the establishment of cardiac networks were analyzed in two observational studies carried out in Australia27 and in Scotland.10
The cardiovascular network implemented in the South of Australia between 2001 and 2008 connected rural hospitals and high-specialized metropolitan hospitals, adopting shared protocols to achieve a fast and accurate diagnosis of coronary events in rural centers and a rapid transfer to metropolitan hospitals if needed. The before–after study examined data referring to 29623 patients with Acute Myocardial Infarction (MI) diagnosis hospitalized between July 2001 and June 2010. 30-day mortality of patients admitted to rural hospitals was decreased from 13.93% to 11.46% after network implementation (p<0.001). Furthermore, 30-day mortality of patient treated in rural hospital belonging to the network was 22% lower than that of patients treated in rural hospital where network was not implemented (ORrisk-adj 0.78; 95%CI: 0.65–0.93; p=0.007).
Results achieved after the implementation of a MCN of cardiac services (made up connecting general practitioner and district hospitals) established in 2001 in Scotland were evaluated in a before–after study conducted on 202 patients with suspected MI diagnosis. The aim of the study was to identify differences in achieving process goals (proxy indicators) before and after the network implementation. Pain to needle target (≤90min) was fulfilled in 32.7% of the cases following the network formalization, against the 15% of the previous period (p=0.05). Furthermore, better results were obtained in secondary prevention after MI: the aim of having at least 70% of patients receiving beta-blockers and at least the 70% of patients with cholesterol >5mmol/l using statins after 6 months from the MI episode was reached, respectively, in 75% and 95.5% of cases, against a previous figure of 61.3% and 80.3% (p=0.05 and p=0.007, respectively).
Chronic kidney disease (CKD) networkEffectiveness of a network implemented to manage patients with stage 3–4 CKD was evaluated through an experimental study with high risk of bias carried out in Thailand between June 2011 and July 2013.28 The intervention group was composed by patients treated within a MCN made up of hospitals and primary health care professionals and of voluntary workers, providing additional services as home visits and training to patients to improve compliance with medications and dietary control. Patients in the control group received conventional treatment. Analysis showed a delay of CKD progression in the intervention group compared to the control group (lower mean difference of estimated Glomerular Filtration Rate (eGFR) over time and lower rate of eGFR decline) and a lower incidence of cardiovascular events, End-stage renal disease and 50% increase in serum creatinine from baseline (HR=0.59, 95%CI: 0.4–0.9, p=0.03).
Reducing the per capita cost of health careHeadache treatment networkEconomic advantages achieved through the establishment of an ISD in Germany were evaluated in a case-control study.29 A reorganization process of health services provision was started in 2007 in a state of the German Federal Republic. The project provided for the stipulation of integration contracts between various care settings and the identification of clinical pathways to take care of eligible patients through settings, with a contextual identification of the most appropriate centers for the treatment of each kind of cranial pain. Patients admitted to the hospitals due to cranial pain were followed for the next two years, and data referred to the two previous years were collected, to allow a comparison before and after the introduction of the new organizational modality. A control group was also set up consisting of patients with comparable clinical and demographic features treated by sectoral modalities. Costs of hospital admission, outpatient services, rehabilitation, pharmaceuticals and social services were collected for each patient. Two years later network implementation, a reduction in direct costs in all the analyzed settings could be observed: 21.5% reduction in the hospital setting and 50.6% reduction in the rehabilitation setting (versus 19.9% and 34.6% rise, respectively, with sectoral organization). Costs of outpatient services were reduced in both organizational models, but the reduction achieved through integrated services was greater (−31.5%) compared with that obtained with sectoral organization (−6.4%).
Personality disorders networkThe personality disorders MCN was established in Leeds, England, in 2004, linking hospitals, primary health care and services offered by the voluntary sector. Economic savings were evaluated through a CBA study.30 Data collected on a sample of patients treated before and after the network implementation were used. Observed differences were compared against a control group trend, constructed using findings in the scientific literature for patients with comparable features, in order to estimate the benefits attributable to the network implementation. The analysis revealed a reduction in total per-capita expenditure for the treated patients (£ 7560 after the implementation of the network, compared to £ 14860 in the previous period) due to a reduction of per-capita costs in all the expenditure items considered: medication, general practitioner, secondary care and mental health services costs. Comparing total costs recorded after network implementation with the estimated costs that could be expected in the control group, there was a 31.9% potential per-capita saving, although costs of network implementation were not considered in the analysis.
Cardiovascular networkCosts of health care services needed to treat patients afflicted by cardiovascular diseases in Scotland were evaluated before and after the network implementation occurred in 2001.10 The analysis of resources used to treat 202 patients with diagnosis of MI was performed, taking into account costs incurred since hospitalization up to 6 months after discharge, including costs of primary and secondary care. Costs of network organization were also considered, including both costs needed to start the project and time resource spent for multidisciplinary and multi-professional meetings. Regression analysis conducted to eliminate confounders showed no statistically significant differences in the average costs per patient before and after the network implementation.
Inter-hospital networksIn a U.S. (United States) study,31 an economic evaluation was conducted to find out if the organization of hospitals who collaborated in a network, determines an efficiency advantage. The study was conducted on 1368 private, short-term, general hospitals in the greater U.S. metropolitan areas. Based on the proportion of services offered through a network participation by each hospital, two thresholds were identified (33.3° and 66.7° percentile of the distribution) to distinguish three levels of network arrangements: low (if less than 2.2% of the services were offered through network), medium (if services offered through network were from 2.2% to 9.4%) or high (if more than 9.4% of services were offered through network), and the X-inefficiency (difference between optimal and current performance) was calculated. Analysis showed that it was the entity of collaboration between members of the network that determined the extent of costs benefits, and not the mere belonging to a network. Medium and high level network collaboration, in fact, was inversely associated with X-inefficiency (respectively, t-ratio −2.05 and −2.17, p<0.05), while these differences disappeared in low-level collaboration.
Enhancing the patient experience of carePatient satisfaction was not investigated in any study through focused surveys. Patient satisfaction was assessed only in a study29 performed in Germany to evaluate outcomes obtained through the establishment of a network for cranial pain treatment, obtaining excellent results (85.4% of patient totally satisfied and 13.4% very satisfied), but comparable data of patients treated with sectoral organization are not available.
Improving the work life of health care clinicians and staffNo studies analyzing health workers’ well-being changes following network implementation have been identified.
Since the studies heterogeneity (different study designs, typologies of network, treated pathologies and outcomes evaluated in each study) a meta-analysis was not performed. Description of studies results was carried out through a qualitative comparative synthesis.
DiscussionThe aim of this systematic review was to evaluate results of clinical networks implementation analyzing the achievement of the Quadruple Aim outcomes.8
Lack of studies with rigorous design limits the ability to draw robust conclusion. Within the twelve studies included in this review, effectiveness and efficiency of clinical networks were reported in 9 and 4 studies, respectively, while patient satisfaction and professionals well-being were neglected.
Different types of clinical network were identified: networks made up of only hospitals with different specialization level, and networks linking hospitals of different levels with general practitioners and, sometimes, with territorial services and voluntary sector involvement. The most suitable type of clinical network often depends on the pathology to treat: acute pathologies are more appropriately treated in networks made up of hospitals, where the centralization of complex procedures into high volume hospitals makes it possible to improve patient outcomes32; chronic pathologies are more properly managed through networks involving more care settings.
Improving the health of populationsAvailable evidences, albeit limited in number and methodological quality, seem to highlight the ability of clinical networks to cause improvements in treated patients’ outcomes. Inter-hospitals networks have showed their effectiveness in improving survival of preterm infants, in reducing all-cause mortality, breast cancer mortality and 30-day mortality for MI, and in improving the process of care (timeliness and diagnostic and therapeutic appropriateness). Timeliness and appropriateness of patients’ care, that correspond with adherence to evidence based guidelines, are significant proxy indicators, because of their association with short- and long-term outcomes improvement.33,34 Furthermore, clinical network has proven effective in improving the secondary prevention of patients with previous MI. This is important because adherence to guidelines is often high in the acute phase of MI (84.2% of patients treated according to evidence based guidelines)35 but is drastically reduced in the next phase (adherence to the main evidence based practices only in 3.5% of cases),36 which is however critical for mortality and recurrence reduction.37 Hematochemical parameters of diabetic patients treated through clinical network testify a better control of the pathology, fundamental for obtaining more favorable long-term outcomes.38
Reducing the per capita cost of health careThree studies showed an improvement of services’ efficiency achieved through network organization, while in one study no differences were founded in sustained expenses before and after the network implementation. It must be taken into account that in two studies showing an increase in efficiency, costs of network's activation and support were not considered. In a study in which these costs were evaluated, no direct economic benefit was shown adopting network organization. However, costs to achieve a network could be huge in a first phase of implementation, and decrease gradually when the new organizational model has entered at operating speed. Furthermore, it must be considered the possible long-term savings due to the diseases treatment through an integrated system, attributable to the improved effectiveness of integrated care in preventing medium and long-term complications. Other sources of savings that could be considered, from a broader perspective, are the reduction of social costs due to less absenteeism and greater work productivity.
Enhancing the patient experience of careIn the analyzed studies, no improvement in patient satisfaction attributable to organizational changes was assessed, although this is relevant for planning services more suitable for users’ needs,39 and for the correlation existing between patient satisfaction and care effectiveness. In fact, patient satisfaction increases adherence to treatments, reduces unhealthy lifestyles and improves the proper utilization of health services.40
Improving the work life of health care clinicians and staffHealth professionals’ well-being has never been evaluated in the analyzed study, although burnout is a very common problem among healthcare workers,41 that can harm professionals, patients and the whole healthcare system. Physicians’ dissatisfaction can contribute to inappropriate prescriptions, with consequent increase in complications’ occurrence possibility and costs, and is associated with a reduction in patient satisfaction and therefore outcomes worsening.42,43 Health professionals’ burnout is also associated with their involvement in patient safety incident, in which they resulted second victims of their errors.44 Health care professionals who feel responsible for a serious medical error may enter a vicious cycle by experiencing negative consequences that often result in defensive medicine, suboptimal patient care and higher odds of future errors.45,46 Burnout limits providers’ engagement and empathy, a crucial component of person-centered care, makes the staff unable to give patients hope, confidence and safety, and makes worse the experience of patients.47 Therefore, joy in work is an essential resource to change patients’ care experience through small acts during the daily care activities, and these little gestures can improve trust between staff and patient, creating a positive care experience that can also make clinicians more resilient to stressful circumstances.48 In a network contest, impact of professionals’ well-being on teamwork (working climate, collaboration willingness) should also be considered, because it could result in a different level of functionality of the whole healthcare system.
More quality perspectives were assessed together in a single study that showed an improvement in pathology control indicators without costs variation. Simultaneous assessment of multiple quality perspectives is essential to provide an indication of the network's global outcomes. A healthcare costs reduction cannot be achieved to the detriment of the effectiveness of the provided care, the patient satisfaction or the professionals’ well-being; nor improvement of these outcomes can be pursue without thinking about their financial sustainability, risking to undermine the whole welfare system or to create gaps in patient's care based on their resources.
In evaluating the results highlighted by this review, some limitations must be taken into consideration. Firstly, the lack of studies with rigorous designs and with low risk of bias does not allow monitoring of an important confounder in the evaluation of the effectiveness of an organizational change, as the time factor, which can influence outcomes by reason of the rapid improvement of care techniques and the possible variation in the people's sensitivity toward benefits of adopting healthier lifestyles.
Implemented clinical networks differs from each other not only for the adopted model (MCN or ISD), or for the involved care settings, but also for some structural elements, such as governance,4,7,9 leadership,4 operational and informative integration methods,3,4,23 that could have enormous implications in the organization of healthcare services in networks and their outcomes, but that often are not deductible from the studies. Furthermore, factors related to the interaction between people operating in the network (influenced by the job satisfaction and the ability of team-working), that could have repercussions on outcomes of the whole system, are not considered.
In addition, it must be considered that the definition of clinical network used in this study was born in nations with a public healthcare system, interested in the identification of organizational methods aimed at coordinating services offered to patients, in order to guarantee them the best quality of their entire care pathway without unnecessary replications of exams and performances, obtaining a more efficient use of resources. This definition is extremely restrictive and does not allow considering other forms of network organization of health services, such as the phenomenon of “consolidation”49 developed within the U.S. private health service in order to reduce competition between healthcare companies, or forms of collaboration in flexible and voluntary network of professionals such as the “communities of practice”. Therefore, it is desirable to take into account, in future studies, also outcomes obtained through the application of alternative forms of network.
Although the quality of the analyzed studies is not optimal, there are some evidences of improvement in effectiveness and efficiency of the care provided through healthcare organization in clinical networks. The result of this review confirm those obtained by Brown et al.,9 and expand them taking into account also the efficiency outcome. Organization in clinical networks was proved to be effective in improving health outcomes, adherence to therapy and efficiency in care provision in medium-low quality studies. These are preliminary results, which should encourage the development of stricter research strategies (ITS, CBA or RCT studies) in order to increase knowledge in this development field, obviating the problem of the multitude of interfering and non-eliminable factors that make complex the evaluation of organizational interventions. In addition, greater attention must be paid, in the next studies, to the evaluation of patient satisfaction, of professionals’ well-being and of outcomes with important repercussions on quality of life and on costs of healthcare system (relapses, re-hospitalizations, patient's general condition deterioration). Furthermore, it must be considered that outcomes produced by a network organization are probably influenced by the typologies of network and by their structural features (governance, leadership, operational and information integration systems, effectiveness of interaction between network operators and their professional fulfillment). Therefore, further studies are needed to evaluate other types of networks, in order to define which is the form of connection between health settings able to produce the best outcomes.
Funding sourceThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations of interestNone.
Authors would like to acknowledge Federico Tirabassi (Polytechnic University of Marche, Italy) and Deborah Seys (University of Leuven, Belgium) for their contribution to the realization of the present review.