Accreditation programs have a crucial role in improving the safety and effectiveness of hospital services. Many factors contribute to achieve accreditation goals. This study evaluated the national Iranian hospital accreditation program from the view of hospital managers in Iran.
MethodsThe study was conducted in 2015 using a validated questionnaire designed to collect feedback concerning accreditation processes and impacts. In total, 547 managers were surveyed using a stratified random sampling method. A 5-degree scale Likert from totally disagree=1 to totally agree=5 has been used for the evaluation. Descriptive and inferential statistics were used to analyze the data.
ResultsApproximately half of hospital managers were satisfied with the accreditation standards and surveying methods. The reason for their dissatisfaction was the high number of measures (2.38). The main challenges to the accreditation method were reported inadequate surveyor training (2.94) their satisfaction with the infrastructure was low because of a lack of hospital resources. Nonetheless, the accreditation program was perceived as being successful in improving patient safety (3.80), patient compliance (3.72), and error reduction (3.53).
ConclusionAn effective accreditation program requires reducing the number of standards and making them clearer as well as the infrastructure for the implementation of accreditation such as sufficient and sustainable funds, enough human resources and equipment should be provided. Appropriate surveyors should be selected and trained professionally to ensure inter-rater reliability among them.
Los programas de acreditación juegan un papel esencial para mejorar la seguridad y la efectividad de los servicios hospitalarios. Son muchos los factores que contribuyen al logro de los objetivos de acreditación. Este estudio evaluó el programa nacional de acreditación hospitalaria de Irán desde la perspectiva de los directores de hospitales iranís.
MétodosEste estudio fue realizado en 2015, utilizando un cuestionario validado, diseñado para recabar comentarios con relación a los procesos de acreditación y su impacto. En total, se encuestó a 547 directores, utilizando un método de muestreo aleatorio estratificado. Para la evaluación se utilizó una escala Likert de 5 grados para el total de desacuerdos =1 con respecto al total de acuerdos =5. También se utilizaron estadísticas descriptivas e inferenciales para analizar los datos.
ResultadosAproximadamente la mitad de los directores hospitalarios estaban satisfechos con los estándares de acreditación y los métodos de inspección. El motivo de su insatisfacción fue el alto número de medidas (2,38). Las principales dificultades con respecto al método de acreditación fueron la formación inadecuada del inspector (2,94). Su satisfacción con la infraestructura fue baja debido a la falta de recursos hospitalarios. Sin embargo, el programa de acreditación se percibió satisfactorio para la mejora de la seguridad del paciente (3,8), cumplimiento del paciente (3,72) y reducción de errores (3,53).
ConclusiónUn programa de acreditación efectivo requiere la reducción de los estándares, que estos sean más claros, y la aportación de infraestructuras para la implementación de la acreditación con fondos suficientes y sostenibles, así como de recursos humanos y equipamientos suficientes. Deberán seleccionarse supervisores adecuados, formados profesionalmente, para garantizar la fiabilidad inter-evaluador entre los mismos.
Hospitals are complex, bureaucratic and multi-specialized social organizations that comprise a significant part of health system budgets. Accessibility, quality, safety and cost are consistent foci for health system policymakers and service managers. Failure to pay attention to efficacy and the mere consideration of effectiveness can result in the provision of health services at very high prices, limiting access.1 Control plays a vital role in the productivity of health organizations, which aims to ensure the achievement of the goals of the organization. The control process is carried out through various mechanisms such as inspection, monitoring, assessment, audit, evaluation and accreditation.2
Accreditation is the process of evaluating the performance of healthcare organizations through initial self-assessment, followed by assessment by an external agency, based on established quality and safety standards.3 Accreditation surveyors collect and record data and information based on hospital accreditation standards, through observation, interview and reviewing documentation. As a result, considering the compliance of hospital services with the clearly defined standards, granting or not granting the certificate to the hospital will be decided on.4
The history of using standards for the external evaluation of healthcare organizations dates back to 1917 by American College of Surgeons in the US.5 Today, most health and medical organizations, especially in developed countries, use accreditation standards.6 In the last 50 years, accreditation has played a significant role in evaluating health organizations throughout the world.7 Focusing on increasing the efficiency and effectiveness of services will reduce unnecessary costs and increase the productivity of medical institutions.
Accreditation standards are far better than the general standards of other quality management models leading to improvements in work processes in hospitals.8 Moreover, accreditation of medical institutions has a significant role in increasing people's confidence in the quality of services provided to these organizations. As a result, medical institutions will be more responsive to the health needs of the people by improving the services provided. Accreditation can also enhance the satisfaction of physicians, nurses and other health care providers,9,10 organizational and individual learning11,12 and facilitate intra-organizational and non-organizational communication.13
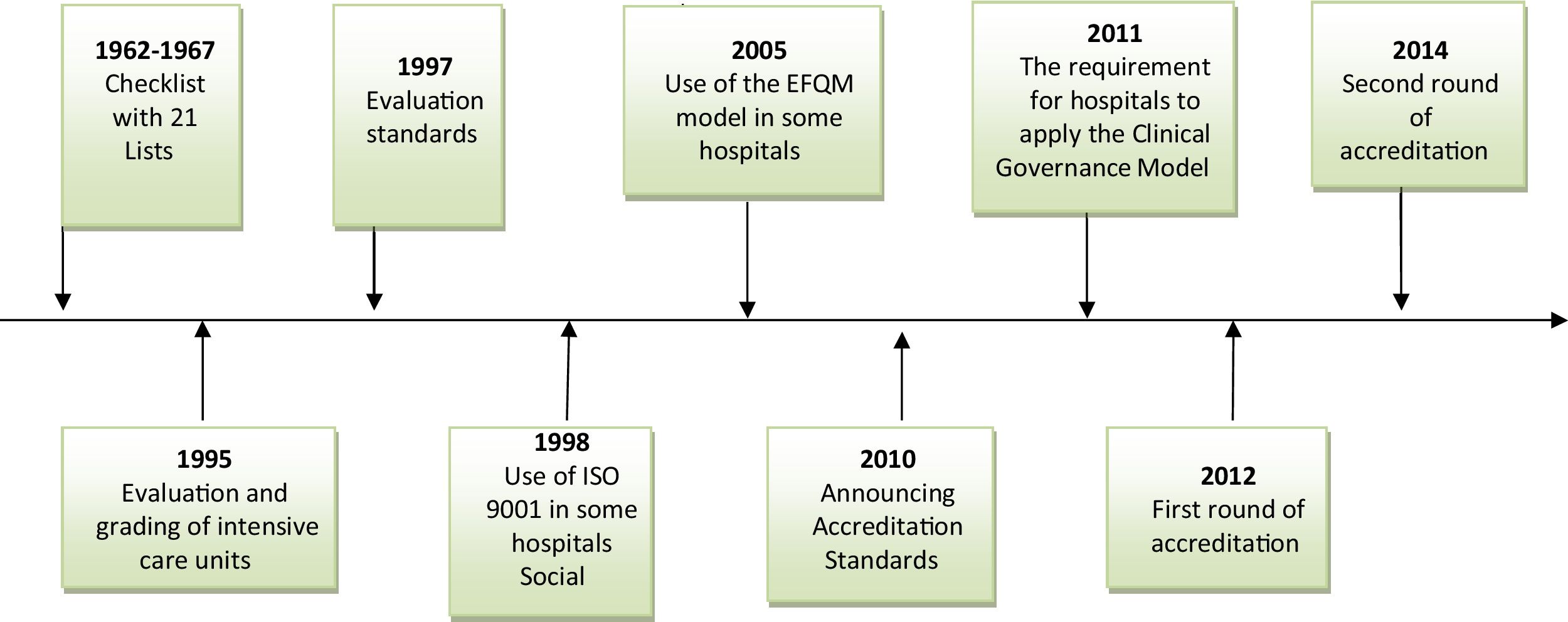
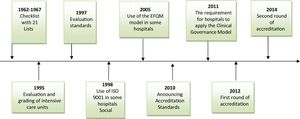
In Iran, Ministry of Health is responsible for hospital quality assurance and in recent years; various methods have been used to ensure the quality of hospital services such as some checklist and evaluation standards. During these years some hospitals also voluntarily used the ISO 9001 (International Organization for Standardization), EFQM (the European Foundation for Quality Management) models or clinical governance for self-assessment and even applied for their certifications (Fig. 1).
The national hospital accreditation system in Iran started in 2012. The accreditation program was a decision made at the Ministry of Health. All types of hospitals including public, private, social security, armed forced, charity and some other hospitals which owned by different organizations should be participate in the accreditation program and The Ministry of Health is currently compulsorily evaluating hospitals only based on this model and all the hospitals perform the accreditation. The hospital tariff is based on its accreditation grade. The higher the hospital grade, the higher the tariffs it charges patients. Hospital grades were Excellent, One positive, One, Two, And Three and non-accredited.14
To develop accreditation standards for hospitals in the country, a review study was conducted on the standards of US, France, Egypt, and Lebanon.15 These standards were localized and national laws and regulations were added. The standards were expressed in 37 sections of the hospital and 8104 measures. The standards were more based on the structure and process standards and the number of outcome standards was very limited. An on-site survey team were composed about 20–25 surveyors who were chosen from university of medical sciences staff in some different fields (e.g. medicine, nursing, pharmacy, health management, etc.). The first accreditation survey was done in 2012. In this round 7.9%, 36.8%, 27%, 18.6% and 4.4% obtained one excellent, one positive, one, two and three respectively. Also 7 Hospitals were evaluated as non-accredited. So almost 71.4 percent of hospitals achieved grade one and over.15
The feedback received from hospitals has been indicative of a large number of standards and measures. Therefore, in 2014 the standards were expressed in 36 sections and 2157 measures. In the second edition, the measures that were taken only with rating documentation were removed and merged with observation and interviews to reduce the amount of documentation.16 Also hospital grades changed to one excellent, one, two, three and non-accredited respectively, so the one positive grade removed.
The accreditation system includes standards, accreditation methods, and accreditation surveyors. To achieve the goals of accreditation, which includes improving the quality and safety, all three components of the program must be coordinated together.2 Some studies have shown that the implementation of accreditation in Iranian hospitals has had many challenges. The lack of necessary infrastructure, lack of human resources in hospitals, lack of cooperation of physicians, high cost of accreditation implementation, increased workload of manpower and time consuming implementation of standards.17–20 Therefore, this study was conducted with the aim of evaluating the accreditation program of hospitals from the view of hospital managers in Iran to identify opportunities for enhancement.
MethodsThis study was conducted in 2015 using a validated questionnaire. The questionnaire was compiled using the data obtained from the comprehensive review done by the authors, which had 50 questions in 5 scales. It was divided into two sections: 1-hospital Profile including type of hospital, number of approved and active beds, use of quality management models, degree of hospital accreditation, the use of the accreditation consultant, the number of staffs in the quality improvement unit and 2-questions related to various aspects of accreditation, including the accreditation evaluation method (8 items), the content of accreditation standards (7 items), the infrastructure of implementation (7 items), the effects of accreditation (24 items) including effects on patients, staffs, hospital and community and the expectations (4 items) that were developed through the 5-degree scale Likert from totally disagree=1 to totally agree=5. There were two open-ended questions about the challenges of the hospital accreditation system in the questionnaire.
The validity of the questionnaire was evaluated based on the ratio of content validity coefficient and expert opinion. All questions had a coefficient of over 90%. Reliability of the questionnaire was also tested through test-retest (Cronbach's alpha coefficient 92%).
Selected study sampleThe included population of this study was managers of hospitals throughout the country (914 people). Using the sample size formula, the total number of samples was 600. A stratified random sampling method was used for sampling. The strata included 57 medical universities in the country. The list of hospitals covered by each university was prepared and from each university a number of hospitals were selected randomly. In each hospital, a questionnaire was completed by the most senior manager within a hospital. A total of 547 completed questionnaires were received. So, about 60% of the hospital managers in the country completed the questionnaire. This study was approved by the institutional review board (IRB) and Code of Ethics Committee is 9121557014.
Statistical analysisData were analyzed using SPSS software version 18 and descriptive and inferential statistical methods. In addition, we investigated the open questions of the questionnaire were also examined using an inductive thematic content analysis approach (Eloo 2007) for data analysis and categorized the themes using MAXQDA.11 software.
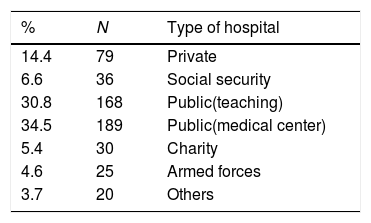
ResultsMost of the hospitals were public teaching hospitals or medical centers (Table 1). Out of 570 public hospitals, 357 hospitals (62%) were surveyed. Out of 337 private hospitals, 79 hospitals were (23%) were surveyed in this study.
The average number of beds approved 172 and the average number of active beds were 145 beds.
Thirty-one hospitals used the ISO model, 32 hospitals used the EFQM model, and 69 hospitals were using the clinical governance model. Based on the results of the second round of the accreditation program, 43 hospitals reported first excellent degree, 197 hospitals reported the first degree, 102 hospitals reported a secondary degree, 24 hospitals reported third degree, and 8 hospitals were rated as non-accredited. Also 85% of the hospitals did not have a consultant. In 85% of hospitals, 1–3 people were engaged in quality improvement units.
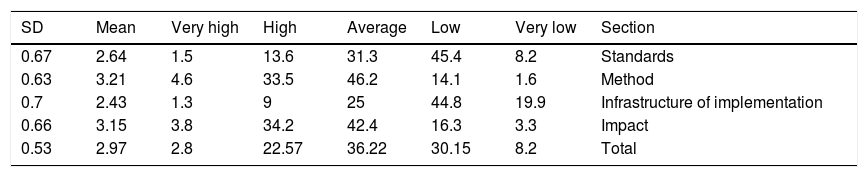
The average satisfaction of Iranian hospital managers from the hospital accreditation system was 2.97 out of 5 points (moderate). About 25% of hospital managers were satisfied with the accreditation system while the satisfaction of 36% of managers was almost average. The highest satisfaction was related to the method (21.3%) and the lowest satisfaction with the implementation of standards (2.43) (Table 2).
Frequency distribution and the mean score of satisfaction of hospital managers in Iran from the dimensions of the accreditation system.
| SD | Mean | Very high | High | Average | Low | Very low | Section |
|---|---|---|---|---|---|---|---|
| 0.67 | 2.64 | 1.5 | 13.6 | 31.3 | 45.4 | 8.2 | Standards |
| 0.63 | 3.21 | 4.6 | 33.5 | 46.2 | 14.1 | 1.6 | Method |
| 0.7 | 2.43 | 1.3 | 9 | 25 | 44.8 | 19.9 | Infrastructure of implementation |
| 0.66 | 3.15 | 3.8 | 34.2 | 42.4 | 16.3 | 3.3 | Impact |
| 0.53 | 2.97 | 2.8 | 22.57 | 36.22 | 30.15 | 8.2 | Total |
SD, standard deviation.
The average satisfaction of Iranian hospital managers with the content of accreditation standards was 2.64 out of 5 points (moderate). Approximately 15.1% of managers were satisfied with the content of the accreditation standards. Most satisfaction of hospital managers was due to attention given to national laws and regulations in developing accreditation standards (3.13) and they’re most dissatisfied with the same weight of different accreditation measures (22.2), non-transparency of measures (2.27) and a large number of standards and measures (2.38).
The average satisfaction rate of hospital managers with the method of accreditation was 3.21 out of five points (average). Approximately 38% of the managers were satisfied with the hospital accreditation method. The most satisfaction of managers was related to the surveyor's behavior (3.75) and the number of evaluation days (3.60). Managers were dissatisfied with the lack of inter-rater reliability between surveyors (2.26) and their low experience and skill (2.94).
The average satisfaction of Iranian hospital managers with infrastructure of implementation in their hospitals was 2.43 out of five (low). Only about 10 percent of hospital managers were satisfied with the infrastructure of implementation at their hospital. Hospital managers were most dissatisfied with lack of human resources (1.78), lack of financial resources (1.99) and the shortage of hospital resources (2.19), and their greatest satisfaction was related to the cooperation of the staff of different departments of the hospital (2.99) in the implementation of accreditation standards.
The average satisfaction rate of Iranian hospital managers from the impacts of implementing accreditation standards in their hospitals was 3.51 out of 5 points (moderate). In general, 38% of hospital managers were satisfied with the impacts of the accreditation program. The greatest impact of accreditation was on the patient (3.36) and its least effect was on the hospital staff (3.03). The accreditation program has been successful in improving patient safety (3.80), patient compliance (3.72), employee safety (3.56), information management (3.69), and reduction of errors and risks in the hospital (3.53). However, the accreditation program has been very weak in areas such as employee satisfaction (98/1), the involvement of physicians in improving work processes (2.2), the use of evidence-based care and medical care (2.51), patient admission (2.60), and the increase in hospital income (2.60).
In the expectations section, most managers would prefer accreditation to be implemented every two years. Approximately 53 percent of hospital managers believed that accreditation had better be done by the Ministry of Health and about 57 percent of managers maintained that it would be better to be done on a compulsory basis. About 95% of hospital managers considered self-assessment before validation necessary.
Inferential analysis of the study showed that there was a significant negative correlation between the number of hospital beds and the impacts of accreditation (r=−0 .90, p=0.038). There was a significant negative correlation between the number of active hospital beds and the impacts of accreditation on the patients (r=−0.95 and p=0.30). There was a statistically significant relationship between the number of staff in the quality improvement unit of hospitals and the degree of accreditation (r=−0.93 and p=0.036). However, there was no statistically significant relationship between the accreditation effects and the degree of accreditation of the first round (p=0.186) and second (p=0.152) in hospitals.
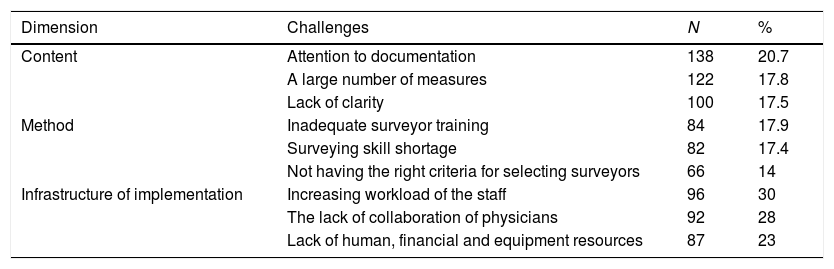
In the open questions of the questionnaire, managers were asked about the challenges of the implementation of the accreditation. These challenges included a total of 2262 cases, some of which were repeated by respondents. Further details are provided in Table 3.
Frequency distribution of Iran accreditation system challenges.
| Dimension | Challenges | N | % |
|---|---|---|---|
| Content | Attention to documentation | 138 | 20.7 |
| A large number of measures | 122 | 17.8 | |
| Lack of clarity | 100 | 17.5 | |
| Method | Inadequate surveyor training | 84 | 17.9 |
| Surveying skill shortage | 82 | 17.4 | |
| Not having the right criteria for selecting surveyors | 66 | 14 | |
| Infrastructure of implementation | Increasing workload of the staff | 96 | 30 |
| The lack of collaboration of physicians | 92 | 28 | |
| Lack of human, financial and equipment resources | 87 | 23 |
This study was conducted with the aim of evaluating the hospital accreditation program from the view of hospital managers in Iran. The results showed that the satisfaction of hospital managers with the content of the standards of accreditation and its method was moderate, but their satisfaction with the infrastructure of implementation was low. Managers also believed that the implementation of accreditation has positive impacts.
Research results that address the challenges of implementation of accreditation standards have shown that, from the perspective of nursing staffs and physicians, the high number of standards and measures is one of the main challenges in hospitals.21 Inappropriate scoring methodology, copying the accreditation standards of other countries, lack of regulatory initiatives, encouraging tools and professional prerequisites were other challenges.22,23
The lack of Inter-rater reliability between surveyors and the low level of expertise of surveyors was a challenge to the accreditation method. The results of some studies which performed in Iran 24,25 also confirm the present study. Those who are selected to evaluate the accreditation of hospitals should have the necessary academic qualifications (level of education and field of study) and have sufficient work experience in the clinical and non-clinical areas. The selection and recruitment of surveyor's team should be based on the Personality-behavioral characteristics and Staffing procedures. The accreditation process and strengthening of the credibility of these processes need surveyors training.26
The result of a research has shown that, low- and middle-income countries are more likely to need to certification processes for trainee surveyors and are more likely to make decisions on the status of accreditation based on a mathematically oriented approach and are less likely than higher income countries to include an evaluation component to programs.27
Lack of human resources, financial resources, and hospital resources were also challenges to the implementation of accreditation from the view of hospital managers in the present study. The results of some other studies which were performed in Iran showed that organizational culture and financial sources are inadequate for accreditation28 and also the most important obstacles to the implementation of accreditation include lack of required knowledge, lack of resources, inadequate manager's commitment and staff skills.29,30
Regarding the impacts of accreditation, the greatest impact of the use of accreditation has been on improving patient safety and the least has been on the involvement of physicians in improving work processes in the present study. The results of a study which aimed at examining the impact of accreditation on providing services from the viewpoint of the Iranian experts, showed that the experts believed that accreditation through continuous monitoring, the establishment of appropriate information systems, transparency of information, and the overall change in the organization's attitude can make a positive impact on achieving goals and improving the quality of services.31
The results of this study were similar to the review of Brazilian nurses’ viewpoints on the impact of hospital accreditation using the results scorecard approach. Nurses believed that some of the items, such as strategic quality planning, quality management, use of data on patients’ satisfaction and participation of hospital staff have improved in quality improvement processes.32 The results of this research are aimed at improving patients’ satisfaction in line with the current research. Also, there is a lack of desirable results in human resources strategies, especially the participation of physicians in Iran's accreditation system.
The results of studies that have examined the impacts of accreditation have shown that accreditation is a good strategy for improving the quality of health services and reducing medical errors.33–35 In addition, accreditation leads to enhanced staff training.36 Hospital managers clearly identify laws, regulations, policies, and procedures for the implementation of accreditation standards and encourage staff to apply protocols and clinical guidelines.37 The implementation of accreditation standards improves the satisfaction of physicians, nurses and other health care providers.38 Accreditation expands organizational and individual learning39 and facilitates intra-organizational and outsourced communication.40
The results of a research have shown that increasing the attractiveness of the accredited organization for customers/purchasers and boosted morale of their staff are other potential advantages.41 The result of a case study has shown that the implementation of accreditation during these 4 years reduced the return to the intensive care unit within 24h of ICU discharge and the staff turnover and also associated with the completion of medical records. These changes translated into total savings of US$ 593000 in Jordan's health-care system.42
Inferential analysis showed that there was a significant negative correlation between the number of hospital beds and the impacts of accreditation. This means that the lower the number of hospital beds, the greater the impact of accreditation. The reason could be that the implementation of accreditation in smaller hospitals has a faster impact. Also there was a significant relationship between the number of staff in the quality improvement unit and the degree of accreditation. Quality improvement unit plays an important role in the implementation of accreditation in Iranian hospitals. Personnel in this department make an important and sustained connection between different departments and staff of the hospital that can affect the accreditation result.16
The results of this research should be interpreted with caution because only the opinions of hospital managers were use. It is suggested that other stakeholders, such as hospital staffs and surveyors, be included in future research. In addition, the study of key performance indicators of hospitals can also indicate the credibility of the accreditation system. Performance indicators are expected to be better in first degree hospitals than second- and third-degree hospitals.
In conclusion, an effective accreditation program requires reducing the number of standards and making them clearer as well as the infrastructure for the implementation of accreditation such as sufficient and sustainable funds, enough human resources and equipment should be provided. Appropriate surveyors should be selected and trained professionally to ensure inter-rater reliability among them.
Source of fundingNo source/authors.
Author contributionsTaraneh Yousefinezhadi performed the data analysis and interpretation and supervised the development of work.
Ali Mohammad Mosadeghrad: helped in data interpretation and manuscript evaluation.
Reece Hinchcliff: helped to evaluate and edit the manuscript.
Ali Akbari Sari: wrote the manuscript and acted as corresponding author.
Conflict of interestsThe authors declare that there is no conflict of interest.
We thank the experts of the evaluation and accreditation department of the Ministry of Health and Medical Education as well as all the heads, managers and authorities responsible for improving the quality of the hospitals who collaborated on the data collection of this study.