Healthcare staff behaviour can impact on the performance of hospitals. Staff involvement in clinical research can have a wider positive effect on patients and hospital performance. The aim of this study was to further assess the putative positive effect of clinical research activity on patient feedback with a more recent dataset, and if staff's motivational engagement levels may impact on aspects of in-patient feedback.
MethodsA retrospective cross-sectional study was conducted with (survey) data from 2019; the sample was 129 English National Health Service hospital Trusts. Sources were the national in-patient survey, national staff survey (for staff motivational engagement), and research activity (based on Trust size-corrected National Institute for Health Research records data). Spearman correlation analyses were conducted (minimum rho value 0.25, p-value<0.005), followed by principal component analysis (score cut-off 0.2).
ResultsInitial correlation analyses identified eleven in-patient survey questions where better in-patient feedback was associated with increased clinical research activity, and only three questions linked with higher degree of staff motivational engagement. Subsequent principal component analysis confirmed that increased staff engagement is mainly linked to overall Trust performance such as staff levels, whereas staff in research-active hospitals provided in-patients with sufficient information – including on medication – and did well answering patient questions.
ConclusionsStaff involvement in clinical research is associated with better patient feedback. Clear and thorough information provision to patients, may be a mechanism for improved patient outcomes including mortality.
El comportamiento del personal sanitario puede repercutir en el rendimiento de los hospitales. La implicación del personal en la investigación clínica puede tener un efecto positivo más amplio sobre los pacientes y los resultados del hospital. El objetivo de este estudio fue evaluar en mayor profundidad el efecto positivo putativo de la investigación clínica en las reacciones de los pacientes utilizando un conjunto de datos más reciente y si los niveles de implicación motivacional del personal pueden afectar a las cuestiones relativas a los comentarios de los pacientes ingresados.
MétodosSe llevó a cabo un estudio transversal retrospectivo utilizando datos (de encuestas) de 2019. La muestra se compuso de 129 «trust» pertenecientes al National Health Service (NHS) inglés. Las fuentes fueron la encuesta de pacientes hospitalizados nacionales, la encuesta nacional de personal (para evaluar la implicación motivacional del personal) y la actividad de investigación (basada en los datos corregidos de los registros de los trust del NHS). Se realizaron análisis de correlación de Spearman (valor mínimo rho de 0,25, valor p<0,005) y análisis del componente principal (punto de corte establecido en 0,2).
ResultadosLos análisis de correlación iniciales identificaron 11 preguntas de la encuesta a los pacientes hospitalizados en las que las mejores reacciones estuvieron asociadas al incremento de la actividad de investigación clínica y solo 3 preguntas estuvieron vinculadas a un mayor grado de compromiso motivacional del personal. El análisis posterior del componente principal confirmó que el incremento del compromiso del personal está vinculado principalmente a los resultados generales del trust, tales como el nivel del personal, mientras que el personal de los hospitales con actividad investigadora aportó a los pacientes ingresados información suficiente — incluyendo la relativa a la medicación — e hicieron bien en responder a las preguntas de los pacientes.
ConclusionesLa implicación del personal en la investigación clínica está asociada a una mejor respuesta de los pacientes. La aportación a los pacientes de información clara y profunda puede ser un mecanismo de mejora de los resultados de dichos pacientes, incluyendo la mortalidad.
The COVID-19 pandemic has placed clinical research firmly into the spotlight, with clinical trials improving treatment of infected patients.1 Beyond the direct benefit that trial participants may get from new and improved treatments, there is a growing body of evidence supporting the wider positive impact that clinical research may have. Lower mortality rates occur in hospitals where more research takes place, and this has been demonstrated at specialty and organisational level.2–5 Other qualitative outcomes are associated with research active hospitals too, and in England clinical research is now incorporated in reviews by the inspectorate for healthcare standards, the Care Quality Commission (CQC) which issues hospitals with a CQC rating for their overall performance.6 Furthermore, since 2019 as part of the national in-patient survey, hospital patients are now asked whether they have been approached for a research study whilst admitted.
A first glimpse into the mechanism underpinning improved wider outcomes for patients who attend a research-active hospital was gleaned recently by comparing activity levels and in-patient survey feedback for English National Health Service (NHS) hospitals. It appears that staff in more research active hospitals provide patients with more information, including about medication and at different stages such as discharge from hospital (reference).7 If we believe that conducting research creates a learning environment, then these observed associations in the NHS between conducting research and healthcare quality may be explained by Spreitzer's workforce “thriving”.8,9 Using factor analysis, Spreitzer found that thriving has two dimensions: (1) engagement (more specifically, vitality) and (2) ongoing learning or improvement. Spreitzer also found that thriving was associated negatively burnout and positively with job performance and extra-role behaviour, and explained variance beyond job satisfaction and organizational commitment.8
The aim of this present study was to compare again research activity and in-patient feedback for English hospitals, to determine if initial findings on research activity and patient feedback could be corroborated. Apart from research activity, other staff related variables may contribute to improved hospital performance and outcomes; one of those, staff motivational engagement, is linked to better CQC ratings and lower mortality.2,3,10 Since research activity (learning) and motivational engagement (vitality) can combined potentially be seen as a degree of staff thriving,3 both variables were included in the analyses.
MethodsFor this retrospective cross-sectional study, publicly available anonymous outcome data for 129 English NHS hospital Trusts was collated. For governance purposes this therefore is classed a service evaluation, rather than research requiring ethics approval. The sources for the majority of the data have been described previously,3 but are summarised in brief. CQC ratings, as of 2019 or as close to that year, were obtained from the CQC website.11 The ratings options are inadequate, requires improvement, good and outstanding and this ordinal ranking was used here. For hospital mortality rates, the Standardised Hospital Mortality Index (SHMI) was consulted.12 In the England, NHS clinical research activity is monitored by the National Institute for Health Research (NIHR) and data was obtained from an open source as previously.13 To make different hospital Trust sizes comparable, through use of a quotient, the total number of patients recruited into interventional trials in 2018–2019 was divided by the whole time equivalent workforce size in each NHS Trust as of January 2019.14 Staff motivational engagement was inputted by utilising the ‘motivation’ section of a validated survey measure (Utrecht Work Engagement Scale).3,15–17 As outlined previously, the mean scores for each member of staff across all three motivation questions is aggregated into a Trust level workforce ‘motivational engagement score’.16,17 Finally, the 2019 NHS in-patient survey was used for analyses, incorporating all the questions that were applicable to all in-patients and excluding specific locality questions such as experience in the emergency department.18 The methodologies underpinning scoring for the staff and in-patient survey respectively are outlined on the NHS digital web site.19
Data was collected in Excel and statistical tests run using SPSS v24. Spearman correlation analyses was performed to assess individual relationships between variables and a minimum rho value of 0.25 and p-value of 0.005 was applied to select candidate in-patient survey questions. Subsequently, using variables significantly associated with either research activity or motivational engagement, principal component analysis (PCA) was performed with a cut-off value of 0.2.
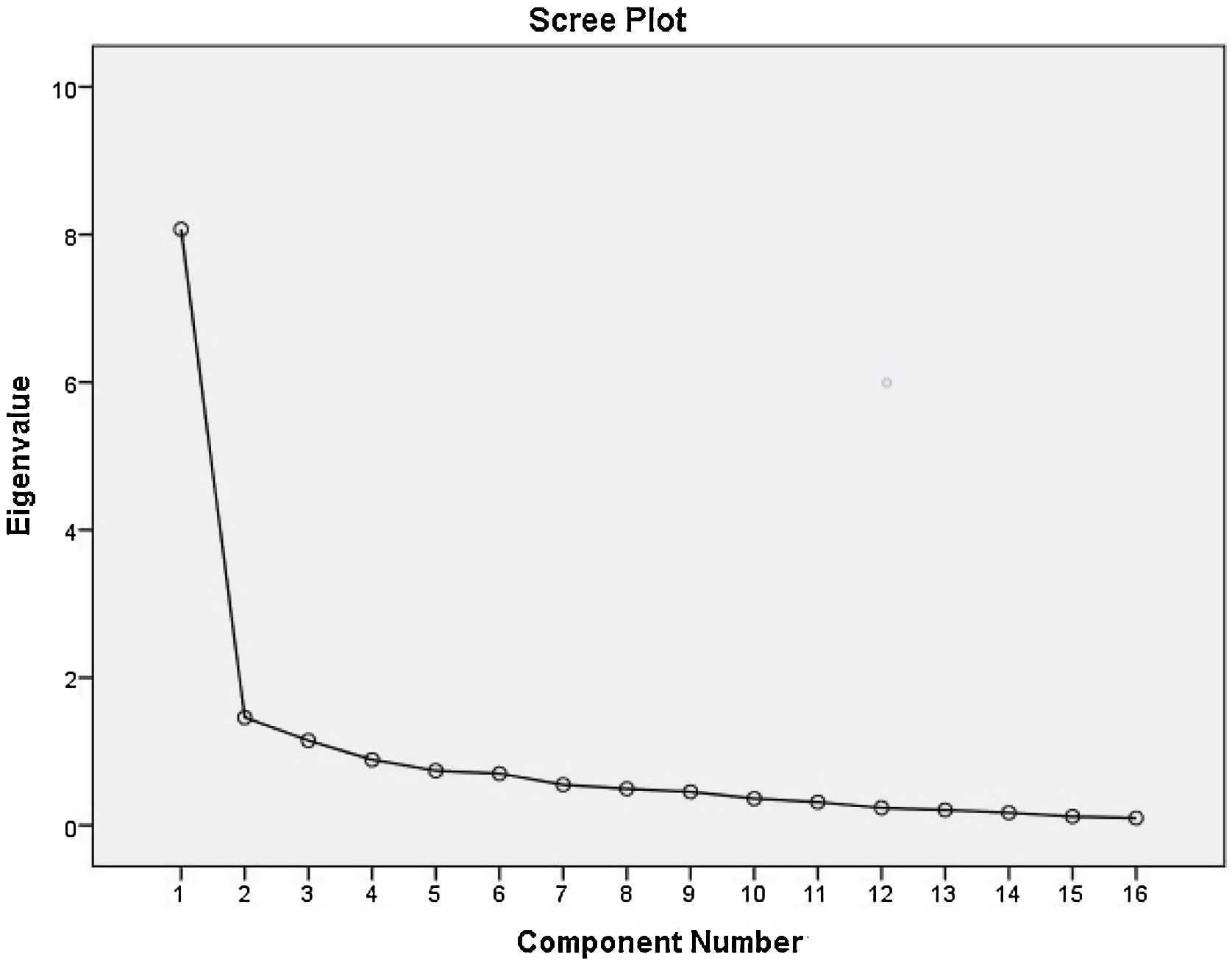
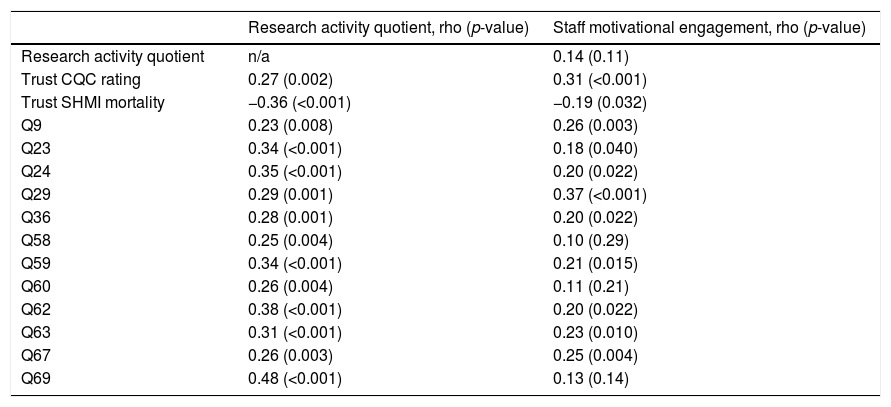
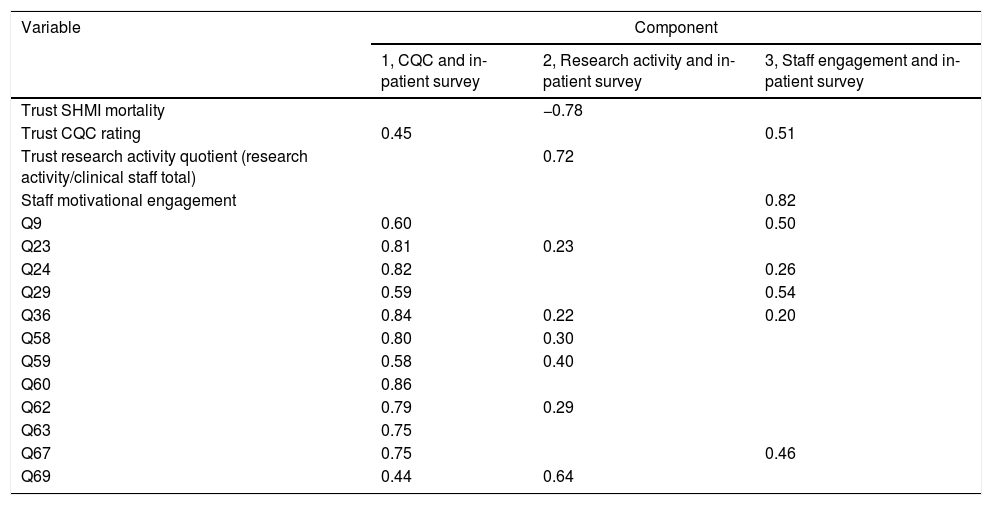
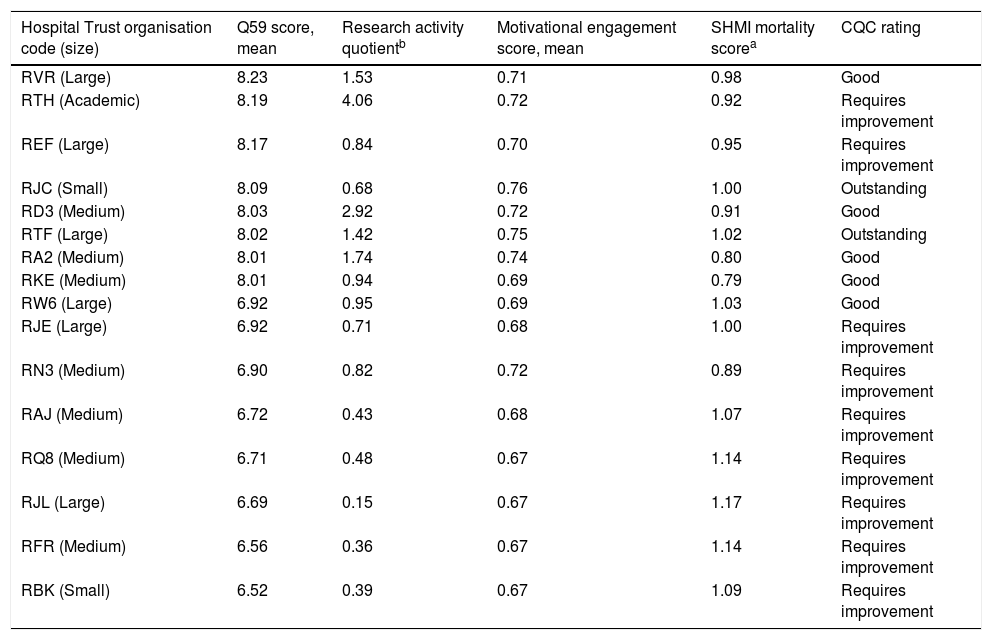
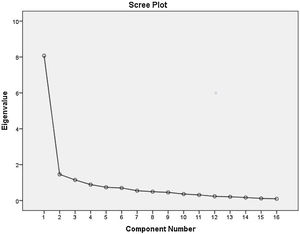
ResultsOf the 129 NHS hospital Trusts, 23 (18%) were classed as small, 42 (33%) medium, 35 (27%) large, and 29 (23%) were large academic Trusts. Table 1 shows the results for the Spearman correlation coefficients when research activity quotient and staff motivational engagement respectively were compared with the in-patient survey questions; only those questions that were significantly associated are listed since the initial list was over fifty questions long. The previously assessed hospital-related outcome measures CQC rating and SHMI mortality are included to allow seeing the relative strength of associated between research activity, motivational engagement and in-patient feedback. Where eleven in-patient survey questions are linked with research activity, with most following the theme of information provision, only three questions relate to staff motivational engagement. The theme for the latter is more overall hospital performance rather than staff performance. The questions identified by spearman analysis were then inputted for PCA assessment. The Kaiser–Meyer–Olkin measure of sampling adequacy was 0.91 for PCA, with a significance level of <0.001, which indicated that the test was valid. Table 2 shows that there are three components to the set of variables and how they interact. The first is the close relationship between all the selected in-patient survey questions, which is no surprise since a patient's response for questions will likely be driven by their overall experience. Fig. 1 shows the strong eigenvalue for the first component, which is the close interrelation between all the NHS in-patient survey questions. The second set of components, titled ‘2, Research activity and in-patient survey in Table 2, is an interaction between research activity quotient and six of the initial eleven in-patient questions identified as individually correlating with the research activity quotient (as shown in Table 1). The overriding theme associated with increased research activity continued to be improved information provision to patients. Question 69, ‘During this hospital stay, did anyone discuss with you whether you would like to take part in a research study?’, stands by itself and shows an expected strong association with research activity. Once again, mortality (SHMI) is joined up strongly with research activity with mortality going down as research activity goes up (PCA score for Trust research activity quotient of 0.72 and score for Trust SHMI mortality score of −0.78, see Table 2) as shown previously.2 The final third set of components in the PCA analysis outcomes in Table 2 shows the association between staff motivational engagement, hospital performance (waiting time, staffing levels, general treatment with respect and dignity), and CQC rating as an indicator of organisational performance. A weaker link with patients having confidence in doctors (question 24) and being given adequate information (question 36) was also detected here with PCA. Table 3 gives a summary overview of the significant results obtained with both Spearman (#) and PCA (◊) analyses – as shown in Tables 1 and 2 and Fig. 1 – with the full text for each in-patient survey question listed. Table 4 illustrates the magnitude in difference between top and bottom performing hospital Trusts using a representative NHS National in-patient survey question, number 59, which asks the question: ‘Were you given clear written or printed information about your medicines?’.
Spearman analysis to explore in-patient survey questions that may link with the degree of research activity and staff motivational engagement in NHS Trusts.
| Research activity quotient, rho (p-value) | Staff motivational engagement, rho (p-value) | |
|---|---|---|
| Research activity quotient | n/a | 0.14 (0.11) |
| Trust CQC rating | 0.27 (0.002) | 0.31 (<0.001) |
| Trust SHMI mortality | −0.36 (<0.001) | −0.19 (0.032) |
| Q9 | 0.23 (0.008) | 0.26 (0.003) |
| Q23 | 0.34 (<0.001) | 0.18 (0.040) |
| Q24 | 0.35 (<0.001) | 0.20 (0.022) |
| Q29 | 0.29 (0.001) | 0.37 (<0.001) |
| Q36 | 0.28 (0.001) | 0.20 (0.022) |
| Q58 | 0.25 (0.004) | 0.10 (0.29) |
| Q59 | 0.34 (<0.001) | 0.21 (0.015) |
| Q60 | 0.26 (0.004) | 0.11 (0.21) |
| Q62 | 0.38 (<0.001) | 0.20 (0.022) |
| Q63 | 0.31 (<0.001) | 0.23 (0.010) |
| Q67 | 0.26 (0.003) | 0.25 (0.004) |
| Q69 | 0.48 (<0.001) | 0.13 (0.14) |
List of in-patient survey questions where a significant [etc] (minimum rho of 0.25 and p-value<0.005) with either research activity or staff motivational engagement was identified. See Table 3 for full description of in-patient survey questions.
Principal component analysis to establish the relationship between in-patient survey questions, hospital outcome measures and staff thriving (through research activity and motivational engagement).
| Variable | Component | ||
|---|---|---|---|
| 1, CQC and in-patient survey | 2, Research activity and in-patient survey | 3, Staff engagement and in-patient survey | |
| Trust SHMI mortality | −0.78 | ||
| Trust CQC rating | 0.45 | 0.51 | |
| Trust research activity quotient (research activity/clinical staff total) | 0.72 | ||
| Staff motivational engagement | 0.82 | ||
| Q9 | 0.60 | 0.50 | |
| Q23 | 0.81 | 0.23 | |
| Q24 | 0.82 | 0.26 | |
| Q29 | 0.59 | 0.54 | |
| Q36 | 0.84 | 0.22 | 0.20 |
| Q58 | 0.80 | 0.30 | |
| Q59 | 0.58 | 0.40 | |
| Q60 | 0.86 | ||
| Q62 | 0.79 | 0.29 | |
| Q63 | 0.75 | ||
| Q67 | 0.75 | 0.46 | |
| Q69 | 0.44 | 0.64 | |
For full description associated with each in-patient question, see Table 3.
Scree plot for principal component analysis (rotated component matrix) to accompany results displayed in Table 2.
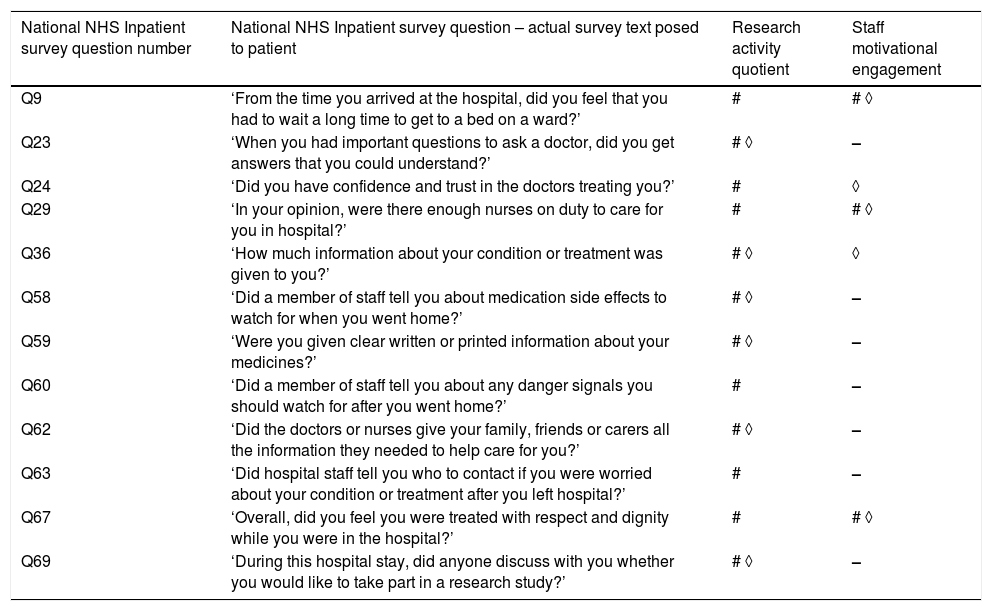
Overview of inpatient survey questions significantly positively associated with either research activity and/or staff engagement.
| National NHS Inpatient survey question number | National NHS Inpatient survey question – actual survey text posed to patient | Research activity quotient | Staff motivational engagement |
|---|---|---|---|
| Q9 | ‘From the time you arrived at the hospital, did you feel that you had to wait a long time to get to a bed on a ward?’ | # | # ◊ |
| Q23 | ‘When you had important questions to ask a doctor, did you get answers that you could understand?’ | # ◊ | – |
| Q24 | ‘Did you have confidence and trust in the doctors treating you?’ | # | ◊ |
| Q29 | ‘In your opinion, were there enough nurses on duty to care for you in hospital?’ | # | # ◊ |
| Q36 | ‘How much information about your condition or treatment was given to you?’ | # ◊ | ◊ |
| Q58 | ‘Did a member of staff tell you about medication side effects to watch for when you went home?’ | # ◊ | – |
| Q59 | ‘Were you given clear written or printed information about your medicines?’ | # ◊ | – |
| Q60 | ‘Did a member of staff tell you about any danger signals you should watch for after you went home?’ | # | – |
| Q62 | ‘Did the doctors or nurses give your family, friends or carers all the information they needed to help care for you?’ | # ◊ | – |
| Q63 | ‘Did hospital staff tell you who to contact if you were worried about your condition or treatment after you left hospital?’ | # | – |
| Q67 | ‘Overall, did you feel you were treated with respect and dignity while you were in the hospital?’ | # | # ◊ |
| Q69 | ‘During this hospital stay, did anyone discuss with you whether you would like to take part in a research study?’ | # ◊ | – |
#, Spearman with cut off of rho 0.25 and p-value 0.005; ◊, PCA analysis with Research Activity Quotient related inpatient questions (cut-off value 0.2); –, not significant.
Top and bottom eight scoring hospital trusts for survey question 59 (‘information on medicines’), to illustrate significant association in-patient feedback score with research activity.
| Hospital Trust organisation code (size) | Q59 score, mean | Research activity quotientb | Motivational engagement score, mean | SHMI mortality scorea | CQC rating |
|---|---|---|---|---|---|
| RVR (Large) | 8.23 | 1.53 | 0.71 | 0.98 | Good |
| RTH (Academic) | 8.19 | 4.06 | 0.72 | 0.92 | Requires improvement |
| REF (Large) | 8.17 | 0.84 | 0.70 | 0.95 | Requires improvement |
| RJC (Small) | 8.09 | 0.68 | 0.76 | 1.00 | Outstanding |
| RD3 (Medium) | 8.03 | 2.92 | 0.72 | 0.91 | Good |
| RTF (Large) | 8.02 | 1.42 | 0.75 | 1.02 | Outstanding |
| RA2 (Medium) | 8.01 | 1.74 | 0.74 | 0.80 | Good |
| RKE (Medium) | 8.01 | 0.94 | 0.69 | 0.79 | Good |
| RW6 (Large) | 6.92 | 0.95 | 0.69 | 1.03 | Good |
| RJE (Large) | 6.92 | 0.71 | 0.68 | 1.00 | Requires improvement |
| RN3 (Medium) | 6.90 | 0.82 | 0.72 | 0.89 | Requires improvement |
| RAJ (Medium) | 6.72 | 0.43 | 0.68 | 1.07 | Requires improvement |
| RQ8 (Medium) | 6.71 | 0.48 | 0.67 | 1.14 | Requires improvement |
| RJL (Large) | 6.69 | 0.15 | 0.67 | 1.17 | Requires improvement |
| RFR (Medium) | 6.56 | 0.36 | 0.67 | 1.14 | Requires improvement |
| RBK (Small) | 6.52 | 0.39 | 0.67 | 1.09 | Requires improvement |
Hospital Trusts are complex organisations and the nature of healthcare means that the performance of said organisations is highly dependent on human performance.20 Finding ways to optimise staff performance may give hospital Trusts gains in patient outcomes. Here, using a different more recent dataset, we confirm that more NIHR-recognised clinical trial activity in a hospital Trust is associated with more favourable in-patient feedback.7 The overriding theme associated with this trend is information provision to patients by staff. Furthermore, on this occasion staff motivational engagement levels were also measured against the in-patient survey. For that variable, more generic survey questions related organisational characteristics – waiting times and staffing levels – showed a significant association.
A new survey question asking in-patients if they have been approached for participation in research also significantly links with an increase in Trust research activity quotient, effectively validating the methodological approach for using the research activity quotient where NIHR-supported research (number of patients recruited into interventional studies) is divided by the whole-time equivalent staff size for each NHS hospital Trust included in the analyses.2,3 The high rho score of 0.48 for the question on research participation is remarkable since not every single patient is approached for research and arguably more patients are approached for research as an out-patient, for example for chronic conditions.2 Limitations of this study include the retrospective cross-sectional nature of the analysis, where a prospective longitudinal study may provide results with a higher degree of confidence. The methodology for the national staff and in-patient surveys was performed by those who devised and analysed those surveys, and therefore the shortcomings around converting some binary or ordinal questions into a mean score falls outside the remit of this study's setup and covered elsewhere.18,19 An example of such a question is number 63, ‘Did hospital staff tell you who to contact if you were worried about your condition or treatment after you left hospital?’, where the possible answers are Yes/No/Don’t know.
Extrapolating conclusions from data analyses involving more than a hundred NHS hospital Trust that each are different from each other can introduce bias and confounding. Academic hospitals often have more advanced diagnostic, medical and surgical facilities. Although these can be used by smaller hospitals through patient referral, this in itself does mean a potential delay in patient care for a patient in the non-academic hospital. This also links in with the optimal size of a hospital, with smaller (<200 beds) and very large hospitals (>600 beds) being sub-optimal.21 In terms of staffing there may potentially to be an element of ‘success breeds success’: Trusts who can offer positions to doctors with a research element in the job description receive more applicants when those jobs are advertised.22 A study in the USA showed the positive effect of employing degree nurses with 30-day mortality in hospitals reducing 5% for every 10% increase in bachelor-level educated nurses.23 Nonetheless, Table 4 shows that both small district hospitals and large university hospitals can be associated with both good and less optimal patient outcomes.
Since this concerns a follow-on study regarding the association between research activity levels and in-patient survey feedback, a comparison can be made to determine if the present results form a trend. Indeed, a number of questions has now shown a significant positive link twice, with each time a significant association using both Spearman and PCA statistical methods.7 These are in-patient survey questions Q36 (‘How much information about your condition or treatment was given to you?’) and Q58 (‘Did a member of staff tell you about medication side effects to watch for when you went home?’). Similar results were obtained for more questions, but not to the same degree as for Q36 and Q58. Overall, there is a very strong link between better and more thorough information provision to in-patients in research-active hospitals. It is a novel finding that staff involvement in clinical trials may drive wider improved performance and care around information provision to patients. Due to the anonymous nature of the datasets used in this study we cannot drill down to patient level. However, a prospective study comparing patient feedback for those who were enrolled in clinical trials and patients who were not would allow for a more detailed appraisal, akin to a study done in colorectal cancer patients.24 At that point it could also be assessed if research participants are more likely to engage in completing a national NHS in-patient survey. The notion of patient education leading to improved clinical outcome is an established one; in for example diabetes care, patients admitted to hospital who are educated about their condition can be discharged earlier and have better post-discharge outcomes.25
An association study between staff motivational engagement levels and in-patient feedback has to our knowledge not been performed previously. Strong links – i.e. demonstrated with both Spearman and PCA methods – between specific staff behaviours and better patient feedback could not be detected. Engagement appears to be linked with higher organisation level issues such as waiting times and nurse staffing levels, as well as general higher levels of respect and dignity shown by staff. This may part-explain why motivational engagement shows strong links with CQC rating.3,10 For the improved staff behaviour associated with research activity in a hospital Trust a certain ‘cause and effect’ direction can be attributed. On the other hand, as shown in a previous study comparing staff motivational engagement levels and SHMI in hospital Trust, the causative direction for the associations seen here with engagement levels and in-patient survey scores is less clear.17 It is feasible that increased nurse staffing levels improves motivational engagement amongst staff, rather than the other way around. The inclusion of both SMHI scores and CQC ratings for hospitals in this sample shows a trend previously reported with this dataset: increased research activity is mainly associated with reduced SHMI mortality, whereas increased staff motivational engagement is associated primarily with improved CQC ratings.3
The results from this study on staff motivational engagement offers very limited defined insight for interventions to use increased engagement to achieve a change in staff behaviour to improve in-patient experience. Changes on an organisational level may aid in improving engagement levels and thereby patient outcomes and hospital performance. For research activity and related patient outcomes there does appear to be scope. Good clinical practice in daily practice is essential for achieving favourable patient outcomes in healthcare. In addition, Good Clinical Practice (GCP) training – devised by the International Committee for Harmonisation – is an essential educational module for staff who wish to conduct clinical trials involving medicinal products.26 Since GCP focuses a lot on the collation and recording of clinical information, as well as patient consent and keeping a patient abreast of developments throughout a clinical trial, the skills obtained from this training may actually be able to positively influence standard clinical care; conducting research would not have to be a prerequisite. Good practice shown by staff in research active hospitals is present at multiple stages of an in-patient journey. For example, there may be an interplay between staffing levels, the degree of information provision and the timing of patient discharge from hospital. Studies have demonstrated that lower nursing staff levels, patient discharge at night, and higher in-patient turnover are all linked with an increase in mortality rates.27,28 Bad habits and resistance to feedback by staff may compound matters and contribute to a poorer patient experience and increased risk of mortality.29 Staff in research active hospitals appear to be more thorough in telling patients about danger signals (Q60), informing patients and wider family and carers about care needs (Q62), and who to contact in case of issues post-discharge (Q63); this may potentially aid in reducing unintended patient deterioration upon discharge from hospital. Further prospective research on discharge practice and policy differences between hospitals could further explore this specific theme.
In order to observe the positive (in)direct effects of clinical research on clinical practice, healthcare professionals need to engage in the research process. Historically, this has not been without challenges. Research has shown that the main drivers for NHS staff to become involved are professional development opportunities (learning new skills, recognition in professional communities) and the potential positive impact of research on clinical practice, rather than monetary motives.30 However, funding for research staff is an important element and a lack of it may have an adverse impact; as an example, a survey involving UK-based consultant paediatricians found that 20% of them had one or more sessions in their job plan, but they got paid for less than half of that planned time.31 In the UK, the introduction of the NIHR to support, fund and orchestrate clinical research delivery has improved matters, and various Schemes – such as the Associate Principal Investigator Scheme to nurture future lead researchers - have been introduced to boost staff engagement in clinical research and level the playing field for all NHS hospital Trusts, regardless of historic research activity levels at said hospitals.32
Staff thriving is a concept that encapsulates both continuous learning (here assumed, but not validated – through engagement in clinical research) and staff vitality (supporting staff motivational engagement) together form the concept of staff thriving,8,9 and are associated with a more positive experience for patients admitted to hospital plus a better hospital performance. This study demonstrates that staff involvement in clinical research, rather than motivational engagement, is significantly linked with improved clinical outcomes for patients and better hospital performance. Sufficient and appropriate information provision to patients is a good habit exhibited by staff in research active hospitals, but importantly it spreads beyond the confines of clinical research activity and therefore may be one mode of action for the improved performance of research-active hospitals. Ways to optimise such traits in clinical staff should be considered by healthcare providers.
FundingNone to declare.
Conflict of interestsBoth LJ and SJF are in receipt of NIHR funding through their regional Clinical Research Network for delivery of NIHR national portfolio studies.
None to declare.