A nosocomial outbreak of coronavirus disease (COVID-19) occurred in the Toda Chuo General Hospital in Toda City, Saitama Prefecture, Japan in December 2020. The purpose of this study was to compare the accuracy of three prognostic indices for predicting the outcome of COVID-19 in patents with COVID-19 pneumonia.
Patients and methodsPatients in the Department of Urology and Transplant Surgery at Toda Chuo General Hospital with nosocomially acquired COVID-19 confirmed by a positive polymerase chain reaction test were included in the study. We used the COVID-GRAM, International Severe Acute Respiratory and Emerging Infections Consortium’s World Health Organization 4C Mortality Score, and COVID-19 Registry Japan to independently predict the prognoses of 10 patients and identify common prognostic factors. All three indices include age, dyspnea, and comorbidities as prognostic factors.
ResultsTen patients were included in the study, of which two patients died. According to the COVID-GRAM both patients were “high risk,” whereas the 4C Mortality Score predicted “high risk” and “very high risk.”
ConclusionThe prognostic scores of all three indices were useful for predicting illness severity.
En diciembre de 2020 se produjo un brote nosocomial de enfermedad por coronavirus (COVID-19) en el Hospital General Toda Chuo de la ciudad de Toda, prefectura de Saitama, Japón. El propósito de este estudio fue comparar la exactitud de tres índices pronósticos para predecir el resultado de COVID-19 en pacientes con neumonía por COVID-19.
MétodosSe incluyeron en el estudio pacientes del Departamento de Urología y Cirugía de Trasplantes del Hospital General Toda Chuo con COVID-19 adquirida por vía nosocomial confirmada por una prueba de reacción en cadena de la polimerasa positiva. Se utilizaron los índices COVID-GRAM, International Severe Acute Respiratory and Emerging Infections Consortium's World Health Organization 4C Mortality Score y COVID-19 Registry Japan para predecir de forma independiente el pronóstico de 10 pacientes e identificar factores pronósticos comunes. Los tres índices incluyen la edad, la disnea y las comorbilidades como factores pronósticos.
ResultadosSe incluyeron en el estudio 10 pacientes. Dos pacientes fallecieron. Según el COVID-GRAM ambos pacientes eran de "alto riesgo", mientras que el 4C Mortality Score predijo "alto riesgo" y "muy alto riesgo".
ConclusiónLas puntuaciones pronósticas de los tres índices fueron útiles para predecir la gravedad de la enfermedad.
Toda Chuo General Hospital is a 517-bed acute care general hospital in Toda City, Saitama Prefecture, with a dedicated ward for patients with coronavirus disease 2019 (COVID-19). On December 19, 2020, an infection was confirmed in one staff member, and simultaneously, six staff members and five patients were also confirmed to be infected. A cluster was consequently confirmed in the hospital, resulting in infections in 150 patients and 174 staff members, among which 45 deaths occurred. The outbreak occurred during the first wave of COVID-19 when no treatment was available. Ten cases of COVID-19 occurred in patients in our department during the outbreak. The purpose of this study was to compare the accuracies of three prognostic indices for predicting the outcome of COVID-19 in patents with COVID-19 pneumonia.
Materials and methodsStudy cohortTen patients in the Department of Urology and Transplant Surgery at Toda Chuo General Hospital with a positive polymerase chain reaction test and a confirmed diagnosis of COVID-19 were included in the study. They were infected at the Toda Chuo General Hospital between December 19, 2020 and January 5, 2021.
Prognostic scoringThe COVID-GRAM, International Severe Acute Respiratory and Emerging Infections Consortium’s (ISARIC) World Health Organization (WHO) 4C Mortality Score, and COVID-19 Registry Japan (COVIREGI-JP) were used as the prognostic scoring tools.
Ethics approvalThis study was approved by the committee of Toda Chuo General Hospital Institutional Review Board (0542).
Statistical analysisA simple descriptive analysis was conducted. In view of the small sample size, no inferential statistics or hypothesis testing were employed.
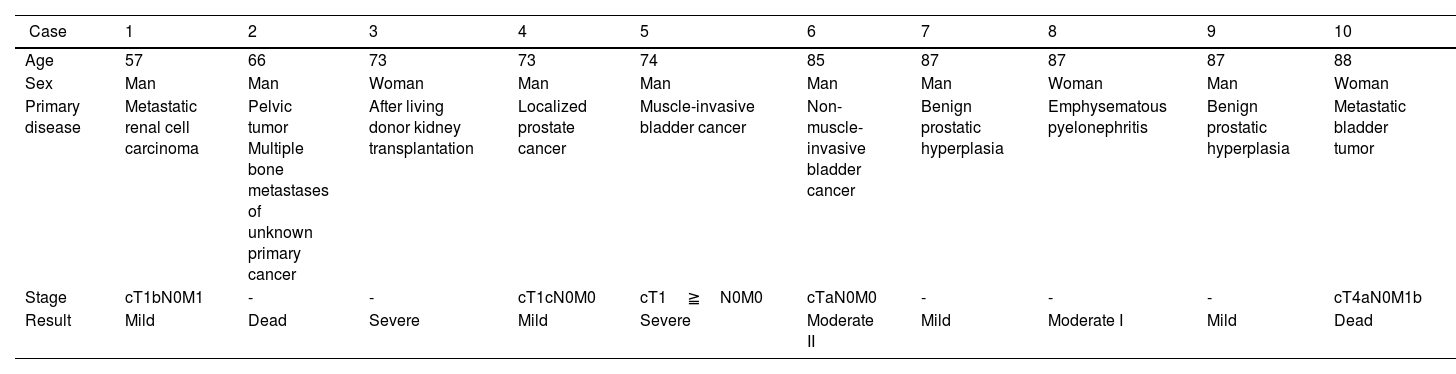
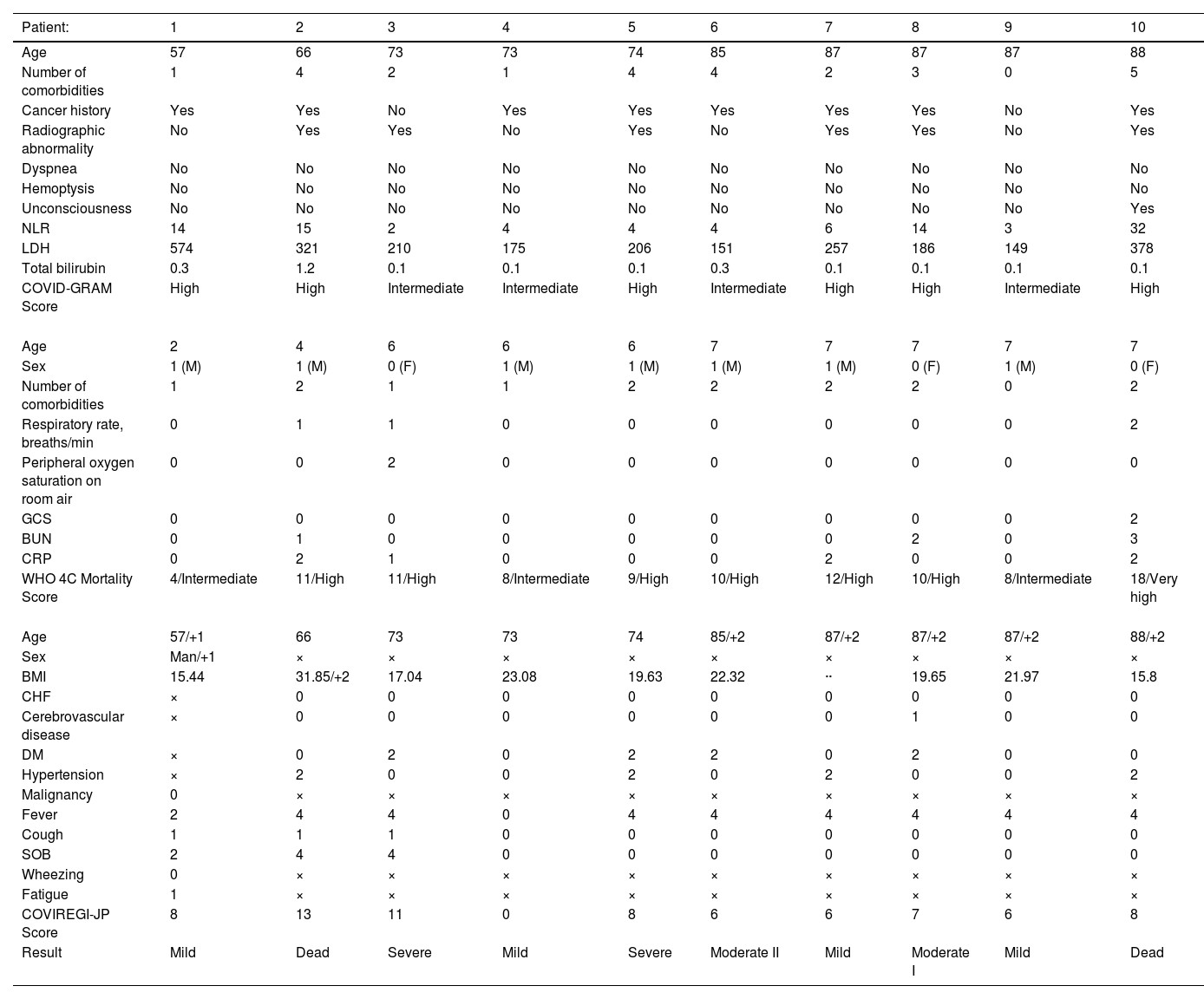
ResultsThe backgrounds of the 10 patients are shown in Table 1. Of the 10 patients, the COVID-GRAM score showed intermediate risk in four patients and high risk in six patients. The ISARIC WHO 4C Mortality Score showed intermediate risk in three patients, high risk in six patients, and very high risk in one patient. Nine patients in the COVIREGI-JP group were at a risk of requiring oxygen therapy (Table 2).
Patient characteristics.
| 【Case】 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Age | 57 | 66 | 73 | 73 | 74 | 85 | 87 | 87 | 87 | 88 |
| Sex | Man | Man | Woman | Man | Man | Man | Man | Woman | Man | Woman |
| Primary disease | Metastatic renal cell carcinoma | Pelvic tumor Multiple bone metastases of unknown primary cancer | After living donor kidney transplantation | Localized prostate cancer | Muscle-invasive bladder cancer | Non-muscle-invasive bladder cancer | Benign prostatic hyperplasia | Emphysematous pyelonephritis | Benign prostatic hyperplasia | Metastatic bladder tumor |
| Stage | cT1bN0M1 | - | - | cT1cN0M0 | cT1≧N0M0 | cTaN0M0 | - | - | - | cT4aN0M1b |
| Result | Mild | Dead | Severe | Mild | Severe | Moderate II | Mild | Moderate I | Mild | Dead |
Determination of the COVID-GRAM score, International Severe Acute Respiratory and Emerging Infections Consortium’s (ISARIC) World Health Organization (WHO) 4C Mortality Score, and COVID-19 Registry Japan (COVIREGI-JP).
| Patient: | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Age | 57 | 66 | 73 | 73 | 74 | 85 | 87 | 87 | 87 | 88 |
| Number of comorbidities | 1 | 4 | 2 | 1 | 4 | 4 | 2 | 3 | 0 | 5 |
| Cancer history | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Radiographic abnormality | No | Yes | Yes | No | Yes | No | Yes | Yes | No | Yes |
| Dyspnea | No | No | No | No | No | No | No | No | No | No |
| Hemoptysis | No | No | No | No | No | No | No | No | No | No |
| Unconsciousness | No | No | No | No | No | No | No | No | No | Yes |
| NLR | 14 | 15 | 2 | 4 | 4 | 4 | 6 | 14 | 3 | 32 |
| LDH | 574 | 321 | 210 | 175 | 206 | 151 | 257 | 186 | 149 | 378 |
| Total bilirubin | 0.3 | 1.2 | 0.1 | 0.1 | 0.1 | 0.3 | 0.1 | 0.1 | 0.1 | 0.1 |
| COVID-GRAM Score | High | High | Intermediate | Intermediate | High | Intermediate | High | High | Intermediate | High |
| Age | 2 | 4 | 6 | 6 | 6 | 7 | 7 | 7 | 7 | 7 |
| Sex | 1 (M) | 1 (M) | 0 (F) | 1 (M) | 1 (M) | 1 (M) | 1 (M) | 0 (F) | 1 (M) | 0 (F) |
| Number of comorbidities | 1 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 0 | 2 |
| Respiratory rate, breaths/min | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Peripheral oxygen saturation on room air | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| GCS | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| BUN | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 3 |
| CRP | 0 | 2 | 1 | 0 | 0 | 0 | 2 | 0 | 0 | 2 |
| WHO 4C Mortality Score | 4/Intermediate | 11/High | 11/High | 8/Intermediate | 9/High | 10/High | 12/High | 10/High | 8/Intermediate | 18/Very high |
| Age | 57/+1 | 66 | 73 | 73 | 74 | 85/+2 | 87/+2 | 87/+2 | 87/+2 | 88/+2 |
| Sex | Man/+1 | × | × | × | × | × | × | × | × | × |
| BMI | 15.44 | 31.85/+2 | 17.04 | 23.08 | 19.63 | 22.32 | ·· | 19.65 | 21.97 | 15.8 |
| CHF | × | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cerebrovascular disease | × | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| DM | × | 0 | 2 | 0 | 2 | 2 | 0 | 2 | 0 | 0 |
| Hypertension | × | 2 | 0 | 0 | 2 | 0 | 2 | 0 | 0 | 2 |
| Malignancy | 0 | × | × | × | × | × | × | × | × | × |
| Fever | 2 | 4 | 4 | 0 | 4 | 4 | 4 | 4 | 4 | 4 |
| Cough | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| SOB | 2 | 4 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Wheezing | 0 | × | × | × | × | × | × | × | × | × |
| Fatigue | 1 | × | × | × | × | × | × | × | × | × |
| COVIREGI-JP Score | 8 | 13 | 11 | 0 | 8 | 6 | 6 | 7 | 6 | 8 |
| Result | Mild | Dead | Severe | Mild | Severe | Moderate II | Mild | Moderate I | Mild | Dead |
BUN, blood urea nitrogen; BMI, body mass index; CHF, congestive heart failure; CRP, C-reactive protein; DM, diabetes mellitus; GCS, Glasgow Coma Scale; LDH, lactate dehydrogenase; NLR, neutrophil-lymphocyte ratio SOB, shortness of breath
Of the ten study patients, two (Patients 2 and 10) died, and two (Patients 3 and 5) experienced severe outcomes. The COVID-GRAM predicted Patient 3 to have intermediate risk, whereas the ISARIC WHO 4C Mortality Score predicted a high risk. Patient 5 was scored as high risk using both these prognostic tools. Patient 2 was also scored as high risk by both these tools, whereas Patient 10 was scored as high risk using the COVID-GRAM and very high risk using the ISARIC WHO 4C Mortality Score. Furthermore, six of the nine patients in the COVIREGI-JP group required supplemental oxygen.
DiscussionThere are several prognostic factors for COVID-19. Currently, vaccination and new oral medications can prevent severe disease; however, at the time of this study, neither vaccination not oral medications were available. We compared the predictive accuracies of three prognostic factor indices, i.e., the COVID-GRAM, the ISARIC WHO 4C Mortality Score, and COVIREGI-JP.1–3 Prognostic factors shared by all three indices included age, dyspnea, and comorbidities. Level of consciousness was common to the COVID-GRAM and the ISARIC WHO 4C Mortality Score, whereas sex was common to the ISARIC WHO 4C Mortality Score and COVIREGI-JP.
SARS-CoV-2 infection following kidney transplantation has been reported to be associated with a higher mortality rate (28%) than that in the general population or in patients older than 70 years.4 Within our patients, Patient 3 had undergone a kidney transplantation and had a severe outcome. In the COVID-GRAM scale, high risk was more common due to the presence of malignancy. Within the 4C mortality scores, the proportion of high risk was high due to the high score due to age. The 4C Mortality Score was more accurate in predicting outcomes than the COVID-GRAM scale.
Patients with perioperative COVID-19 infections have a significantly higher risk of postoperative complications, especially in men older than 70 years.5,6 Postoperative pulmonary complications occurred in half of the patients with COVID-19 infections diagnosed from within seven days pre-operation to 30 days post-operation and were associated with a high mortality rate.5 Patient 5, a man aged over 70 years, experienced severe complications on the eighth postoperative day.
Patients 2 and 10 died. Patient 2 had a pelvic tumor of unknown origin with bone metastasis, and Patient 10 had a metastatic bladder tumor with uterine invasion and lung metastasis. Metastases may contribute to severe disease and death. Old age is the most important risk factor for severe disease, and in an analysis using COVIREGI-JP, the fatality rate was 3.9% in patients aged 60 years or older with no underlying disease and 12.8% in patients aged 60 years or older with underlying disease.3,7 Although the number of cases in this study was small, the patients with underlying conditions, such as metastatic cancer and an immunosuppressed status, tended to develop more severe COVID-19 pneumonia. In addition, several meta-analyses have shown that men are at a higher risk of severe illness and death than women.8 With the development of vaccination and treatment methods, new prognostic factors should be evaluated in the future.
In conclusion, all three prognostic scoring systems were useful for predicting illness severity.
Funding sourceThis research received no external funding.
Approval by institutional review boardThis study was approved by the committee of Toda Chuo General Hospital Institutional Review Board (0542).
Informed consentWritten informed consent was obtained from the patient for publication of this report.
Author contributionsY.K. and T.S.: writing – original draft preparation; H.T., S.I., M.I and T.T.: writing – review and editing.
The authors would like to thank Editage (www.editage.jp) for English language editing.