Technology Enhanced Medical Education International Conference (THEME 2019)
Más datosThis study was aimed to see the impact of sleep quality on the cognitive function of a patient with acute ischemic stroke.
MethodThis was an observational study with a cross-sectional approach involving 45 samples taken through the consecutive sampling method between April and May 2019. Sleep quality was assessed through the Pittsburgh Sleep Quality Index (PSQI), while the cognitive function was assessed through the Mini-Mental State Examination (MMSE). Data were analyzed by Chi-square test.
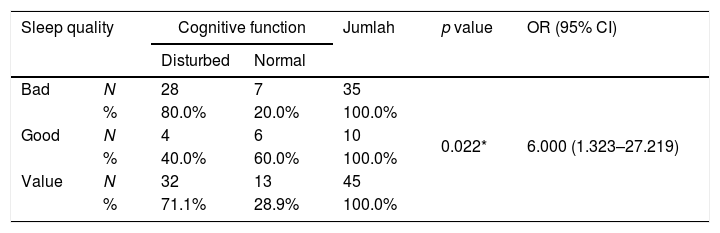
ResultAccording to a statistical analysis done in the study, the p-value for the effect of sleep quality and cognitive function was 0.022 (OR 6.0, confidence interval 1.323–27.219).
ConclusionPoor quality of sleep correlated to cognitive function 6 times higher than good sleep quality.
Stroke is the leading cause of death in most hospitals in Indonesia by 14.5%. The highest prevalence of stroke based on the diagnosis of health and symptoms was found in South Sulawesi (17.9%), Yogyakarta (16.9%), Central Sulawesi (16.6%), and East Java (16%).1
Besides mortality, disability due to stroke can occur in the form of impaired noble functions, including cognitive function, depression, and emotions.2 Increased sleep disorders are associated with significant negative impacts on stroke outcomes.3 Poor sleep quality can affect the degree of disability in stroke patients.4 Thalamic injury can cause arousal disorders, hypersomnolence, and cognitive injury.5
Research has shown that poor sleep is associated with more reduced general cognitive function as well as disorders in specific cognitive domains. A meta-analysis concluded that people with insomnia symptoms showed a decline in cognitive function in episodic memory, working memory, and executive function.6
Therefore, this study aimed to find out the relationship between sleep quality and cognitive function, whether there is an effect of Sleep Quality on Cognitive Function in Acute Ischemic Stroke Patients.
MethodResearch locationThe research was conducted in an outpatient unit of Dr. Wahidin Sudirohusodo's General Hospital in Makassar.
Types and sources of dataThe study sample is an affordable population that meets the criteria of inclusion and exclusion. Inclusion criteria in this study All patients with acute ischemic stroke as evidenced by head CT-scan, onset ≤14 days, first attack, GCS patients 15, aged over 18–65 years, patients who agreed to be included in the study. Exclusion criteria are patients who are unable to read and write, patients with structural abnormalities in the brain such as brain tumors, head trauma, brain abscesses, history of alcohol dependence, history of psychiatric illnesses, routine use of hypnotic and sedative drugs, previous post-stroke patients.
Data collection techniquesData were collected from samples that met the inclusion criteria by filling in the PSQI and MMSE questionnaires. It was processed using Microsoft Excel and SPSS 22.0, with a Chi-square test.
ResultThis research was conducted at Wahidin Sudirohusodo's General Hospital for Education and all network hospitals in April–May 2019. In this study, a total sample of 45 people was obtained who had met the inclusion criteria.
The relationship between sleep quality and cognitive function. A total of 35 respondents with poor sleep quality, including 28 respondents with poor sleep quality with disturbed MMSE (80.0%), seven respondents with poor sleep quality with normal MMSE (20.0%), and good sleep quality of 10 respondents, including four respondents (40.0%%) with MMSE being interrupted, six respondents (60.0%) with normal MMSE. Statistical test results obtained p-value (0.022) <0.05, which means there is a relationship between PSQI and MMSE, with an OR value of 6,000, which means that people who have poor sleep quality six times have MMSE disturbed compared to those with good sleep quality. Described in Table 1.
DiscussionSleep disorders often occur in stroke patients. Sleep problems are associated with all types of strokes, and poor sleep quality is associated with critical adverse effects on stroke outcomes, one of which is cognitive injury.4
A recent study shows that beta-amyloid accumulation results in decreased and fragmented sleep and lack of sleep for one week increases the beta-amyloid burden, showing a two-way relationship between sleep and cognition.7 Sleep disturbance correlates with cognitive impairment in people, adult males, and females. β-amyloid peptides have been linked to neurodegenerative diseases, causing learning and memory disorders. In vivo mouse studies have found that cleansing β-amyloid occurs through the brain's lymphatic system. The study further revealed that interstitial space increases during sleep, results in a striking increase in convective exchange of cerebrospinal fluid with interstitial fluid, and finally increases the rate of β-amyloid cleansing during sleep. Sleep deprivation reduces the convective exchange of cerebrospinal fluid with interstitial fluid and reduces the rate of β-amyloid clearance, which correlates with cognitive impairment.8 Locus coeruleus is essential for arousal regulation, and there is evidence for its contribution to cognitive performance, the latter possibly related to neuronal projections from the coeruleus locus to the prefrontal cortex. A recent animal study showed that lack of sleep could result in a loss of neurons in the locus coeruleus, which can cause negative cognitive consequences.7
As many as 35 respondents with poor sleep quality, including 28 respondents whose sleep quality was poor with MMSE disturbed (80.0%), seven respondents who had poor sleep quality with normal MMSE (20.0%), and those who had good sleep quality were ten respondents, including four respondents (40.0%) with disturbed MMSE, six respondents (60.0%) with normal MMSE. Statistical test results obtained p-value (0.022) <0.05, which means there is a relationship between sleep quality and cognitive function, with an OR value of 6,000, which means people with poor sleep quality six times have impaired cognitive function compared to those with good sleep quality.
However, this contradicts research by Kyle et al. (2017) showing that people with cognitive impairments are more than three times more likely to have sleep problems than cognitively healthy controls, even after adjusting for MMSE, so it is said that sleep problems are not associated with decreased function cognitive. However, sleep disorders can reflect ongoing neurodegenerative processes.6 It is according to a study by Mecca et al. (2018) reporting no relationship between sleep disorders and cognitive decline. Although sleep and memory disorders increase over time, a slowdown and imbalance considered for patient improvement and poor recovery from ischemic stroke patients indicate early treatment interventions.5
ConclusionIn this study, sleep quality was associated with decreased cognitive function in patients with acute ischemic stroke. Poor sleep quality affects cognitive function six times higher compared to good sleep quality.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the Technology Enhanced Medical Education International Conference (THEME 2019). Full-text and the content of it is under responsibility of authors of the article.