Technology Enhanced Medical Education International Conference (THEME 2019)
Más datosTo find out the correlation between sleep quality and the drug compliance of antiepileptic drugs in epilepsy patients.
MethodThis was an analytic observational study with a cross-sectional approach. The sample was taken from the interview process to epilepsy patients in Wahidin Sudiohusodo and its networking hospital. Primary data was done through PSQI (Pittsburgh Sleep Quality Index), while secondary data was obtained from medical records. Data were analyzed using Chi-Square.
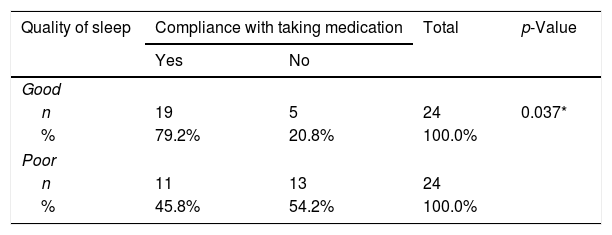
ResultThis study involved 48 samples, 24 samples with good quality of sleep, and 24 others with bad ones. There were 19 samples with good quality of sleep and drug compliance, five samples with good quality of sleep yet inadequate drug compliance, 11 with bad quality of sleep yet proper drug compliance, and 13 with bad quality of sleep and drug compliance.
ConclusionThere was a significant correlation between sleep quality and drug compliance of antiepileptic drugs in a patient with epilepsy.
Epilepsy is a brain disorder characterized by a tendency to cause continuous epileptic seizures, with neurobiological, cognitive, and social consequences, while epileptic seizures occur for a momentary sign and symptom due to abnormal and excessive neuronal activity in the brain.1,2 Epilepsy is a chronic disease that found in 0.5–1% of the total population. According to WHO, an estimated 50 million people worldwide have epilepsy. The prevalence and incidence of epilepsy in Indonesia are not known with certainty. The results of the Epilepsy Study Group of the Indonesian Neurologist Specialist Association in several hospitals in 5 major islands in Indonesia (2013) found 2288 people with epilepsy with 21.3% new patients. The most common age is the productive age, with the most common etiology of epilepsy is a head injury, central nervous system infections, strokes, and brain tumors. A history of febrile seizures was obtained in 29% of patients, of which most (83.17%) were partial epilepsy with aura.
The incidence of epilepsy is still high, especially in developing countries, which reaches 114 per 100,000 population per year. Sleep quality is a person's ability to be able to maintain sleep, get enough hours of sleep, and feel the darkness in his sleep. Epilepsy patients have a relationship with sleep, and vice versa, sleep can affect the occurrence of attacks in epilepsy patients, so there is a reciprocal relationship between the two and affect the sleep quality of people with epilepsy. The sleep quality of epilepsy patients was measured by the Pittsburgh Sleep Quality Index (PSQI) and the Insomnia Severity Index (ISI) questionnaires that had been studied as qualified. Many things affect the sleep quality of epilepsy patients, including sleep disorders, where sleep disorders of epilepsy patients are 2–3 times more frequent than the general population. No studies are comparing the sleep quality of epilepsy patients to adherence to taking anti-epileptic drugs.
Recent research shows that the global effects of epilepsy are quite high. Surveys show that patients with epilepsy have the opportunity to have a lower quality of life than the general population. Sleep disorders in people with epilepsy are 2–3 times more frequent than in the general population.3,4 Sleep disorders often occur in epilepsy patients and can be treated. Epilepsy and its treatment, including epilepsy drugs consumed, can affect sleep orgasm and contribute to daytime sleepiness, insomnia, sleep disorders, and OSA, while the accompanying sleep disorder treatment can control seizures, daytime alertness and both. Based on the description above, the researcher wants to conduct a study that examines the relationship of sleep quality in epilepsy patients with adherence to taking anti-epilepsy drugs.5,6
MethodResearch designThis research is an observational study with a cross-sectional approach, which is an observational study that seeks the relationship between independent variables and dependent variables by measuring at one time.
Time and research locationThe study population was epilepsy sufferers at the Nerve Poly Wahidin Sudirohusodo Education General Hospital and Network Hospital. The sample of this study was epilepsy sufferers who used OAE while undergoing treatment in April–May 2019.
Research samples and sampling techniquesThe study was conducted at the Neurology Polyclinic at Wahidin Sudirohusodo General Hospital and Network Hospital, in April–May 2019.
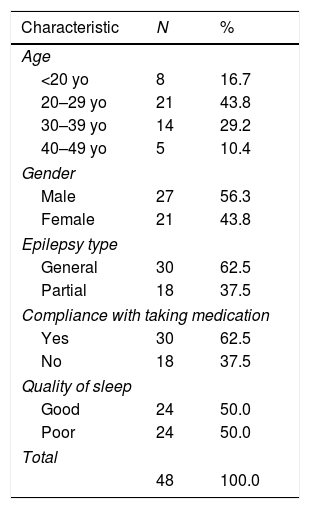
ResultCharacteristics of samplesThe total research subjects who met the inclusion criteria were 48 people. Table 1 shows, baseline data from the research subjects showed that the male and female gender composition in this study was predominantly male, where there were 27 men (56.3%) and 21 women (43.8%), with the highest age distribution at age<20 years as many as eight subjects (16.7%), then aged 20–29 years were 21 subjects (43.8%), aged 30–39 as many as 14 people (29.2%) and ages 40–49 as many as five people (10.4%). There were thirty subjects (62.5%) with generalized epilepsy and 18 subjects (37.5%) with partial epilepsy.
Demographic data of research samples.
| Characteristic | N | % |
|---|---|---|
| Age | ||
| <20 yo | 8 | 16.7 |
| 20–29 yo | 21 | 43.8 |
| 30–39 yo | 14 | 29.2 |
| 40–49 yo | 5 | 10.4 |
| Gender | ||
| Male | 27 | 56.3 |
| Female | 21 | 43.8 |
| Epilepsy type | ||
| General | 30 | 62.5 |
| Partial | 18 | 37.5 |
| Compliance with taking medication | ||
| Yes | 30 | 62.5 |
| No | 18 | 37.5 |
| Quality of sleep | ||
| Good | 24 | 50.0 |
| Poor | 24 | 50.0 |
| Total | ||
| 48 | 100.0 | |
Of 48 research subjects, 30 people (62.5%) had adherence to taking drugs, while as many as 18 people (37.5%) research subjects did not have adherence to taking anti-epileptic drugs. The quality of sleep with poor quality of sleep means the value of filling out the PSQI questionnaire>5. Of the total 48 subjects, 24 people (50%) had good sleep quality, and 24 people (50%) had poor sleep quality.
PSQI component characteristicsTable 2 shows that in this study 48 samples fulfilled inclusion criteria, 24 with good sleep quality and 24 with poor sleep quality, consisting of 19 adherent drug samples with good sleep quality, 11 adherent drug samples with poor sleep quality, five samples non-adherent drug with good sleep quality, and 13 samples of non-adherent drug with poor sleep quality. Subjects obtained by using a non-random sampling method. Data analysis using the Chi-Square test obtained p-value=0.037 (p<0.05) from the results of sleep quality with medication adherence.
DiscussionSleep quality of subjects on the PSQI that had a questionnaire value>5 out of a total of 21 was said to have poor sleep quality. There is no further explanation regarding the reduced level of sleep quality difference between patients with PSQI>5. In this study, 48 samples met inclusion criteria, 24 with good sleep quality and 24 with poor sleep quality, consisting of 19 adherent drug samples with good sleep quality, 11 adherent drug samples with poor sleep quality, five non-adherent drug samples with sleep quality was good, and 13 samples did not comply with drugs with poor sleep quality. Data analysis using the Chi-Square test obtained p-value=0.037 from the results of sleep quality with medication adherence. Which states there are differences in sleep quality between epilepsy patients who adhere to medication and those who do not comply with anti-epileptic drugs.6
ConclusionThere is a statistically significant difference in the quality of sleep in epilepsy patients with adherence to taking anti-epileptic drugs. Where in patients who have adherence to taking drugs, have better sleep quality compared to patients who are not compliant taking anti-epileptic drugs.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the Technology Enhanced Medical Education International Conference (THEME 2019). Full-text and the content of it is under responsibility of authors of the article.