Technology Enhanced Medical Education International Conference (THEME 2019)
Más datosHypersomnia/excessive daytime sleepiness post-stroke is a condition of prolonged daytime napping and nighttime sleep following a cerebrovascular accident. The incidence of sleep disorders occurs in more than 40% in the chronic phase and 70% in the acute phase. The incidence of hypersomnia increases in the first month after stroke.
MethodsBased on observations by Von Economo found that symptoms of excessive sleepiness are often found in individuals with lesions in the junction area between the posterior hypothalamus and mesencephalon. Drowsiness can be caused by the presence of a direct lesion in the Reticular formation, which located in the midline region of the diencephalic structure caused by the involvement of the fibers tract, which builds Ascending Reticular Activating System (ARAS). ARAS is a central nervous system that has functions as a promotor of the sleep-wake process. There have been few cases of the mesencephalon and cerebellar infarction that affect the ARAS, which causes excessive drowsiness and hypersomnia.
ResultsThis case will present a patient with ischemic stroke in the mesencephalon and cerebellar regions that affect the ARAS, thus providing symptoms of excessive drowsiness, nystagmus, multiple cranial nerve palsy and spastic hemiparesis due to the presence of several atherosclerotic plaques in the posterior circulations. This study used the Epworth Sleepiness Scale questionnaire to establish a diagnosis of hypersomnia. The administration of therapy depends on the underlying cause.
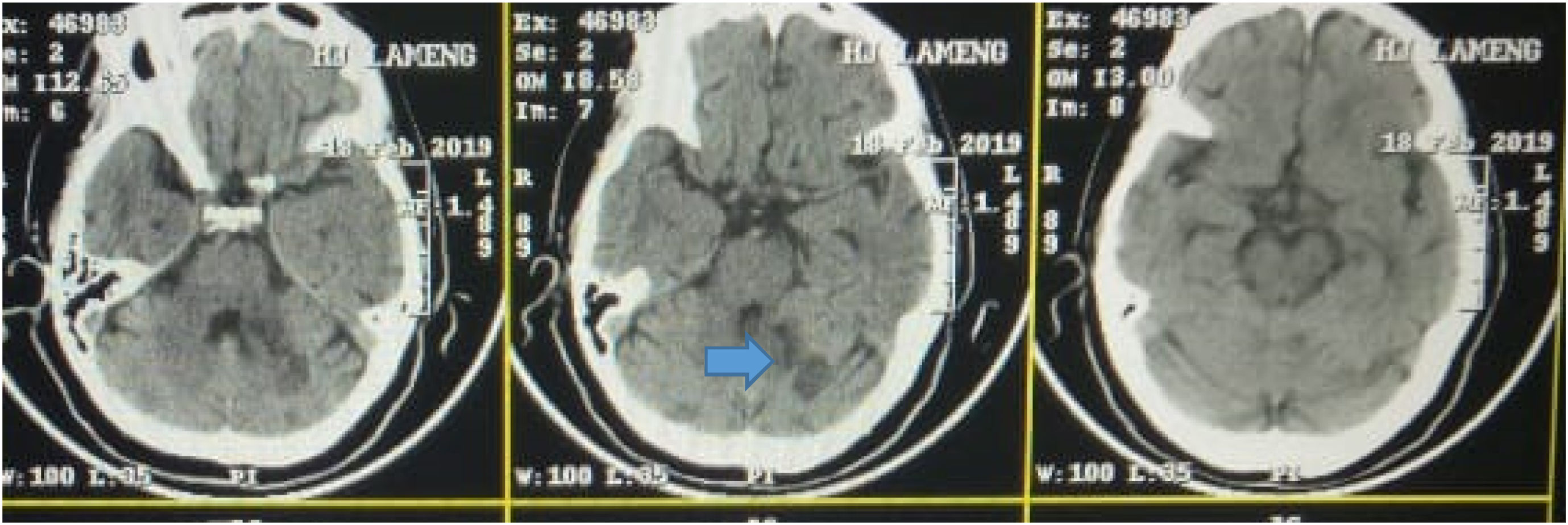
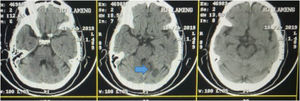
A woman, 63 years old, entered the hospital with complaints of weakness of the right of the body since two days earlier, suddenly, preceded by dizziness. There was no history of fever and head trauma, loss of consciousness, nausea, headache, and vomiting was present. Her systolic blood pressure was 170mmHg. Patients tend to sleep during the day, but according to the family, the night's sleep is sufficient. It found a history of hypertension and diabetes mellitus but does not seek any treatment. On physical examination, blood pressure was 140/90mmHg, pulse was 83 per minute regularly, breathing was 20 per minute, and body temperature was 36.6 centigrade. Glasgow coma scale was E4M6V5 (somnolence). The cortical function was within normal limits. There was vertical nystagmus, multiple cranial nerve palsy (facial palsy and right twelfth of nerve, third nerve palsy, and left the sixth nerve). Two-fifth motoric power on the right and left extremities, right hemihypesthesia, and Babinski positive bilateral. On the Epworth Sleepiness Scale examination, the score was 17. From the laboratory examination found significant results in blood sugar (GDS) of 155mg/dL, Fasting Blood Sugar (GDP) 151mg/dL, HbA1C: 7.7%, Total Cholesterol: 218mg/dL, HDL: 34mg/dL and LDL: 172mg/dL. From the head CT scan head without contrast, radiology concluded that there is a hypodense lesion in the left cerebellum (flocculonodular lobe area), but upon further observation, there was a hypodense lesion in the left mesencephalon (Fig. 1).
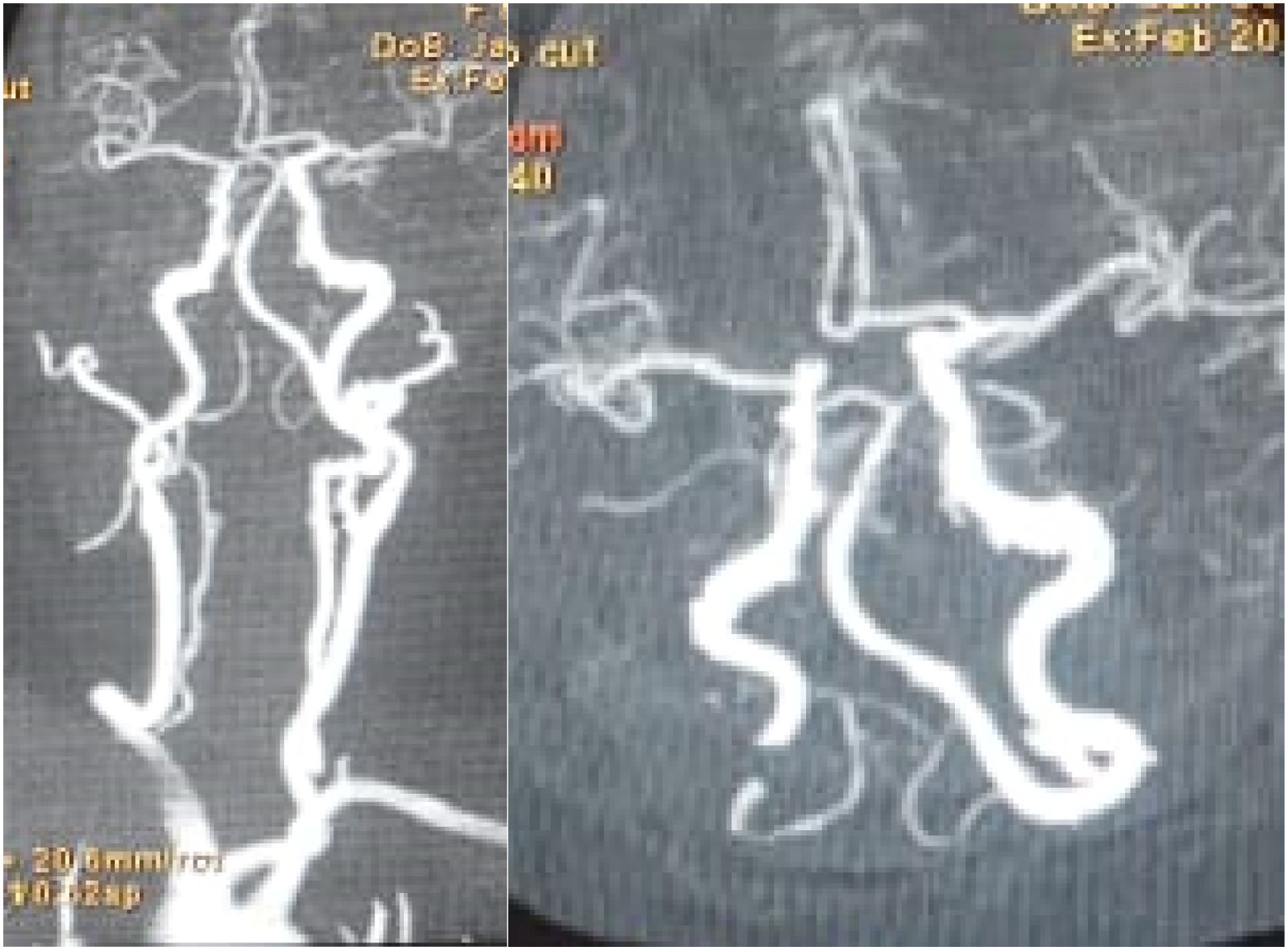
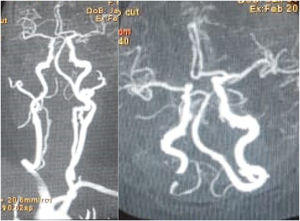
Then proceed with head and neck CT scan angiography with contrast obtained atherosclerotic plaque at several locations (Fig. 2).
The result of head and neck CT scan-angiography with contrast. There were multiple atherosclerotic plaque at Anterior Cerebral Artery dextra, Carotis Communis Artery Sinistra, Internal Carotid Artery Dextra et Sinistra, Vertebralis Artery, Basillaris Artery, and Posterior Cerebral Artery.
Based on the history, physical examination, laboratory examination, and radiological examination, the patient was diagnosed with ischemic stroke accompanied by excessive daytime sleepiness or hypersomnia. And given dual antiplatelet therapy, atorvastatin, and metformin.
DiscussionStroke was defined by the American Heart Association (AHA/ASA) as symptoms of neurological deficits due to acute brain function impairment both focal and global, caused by reduced or loss of blood flow in the brain, retinal or spinal cord parenchyma, which can be caused by blockage or rupture of arteries and veins, as evidenced by imaging and pathology. Ischemic stroke is an episode of neurological dysfunction caused by cerebral, spinal or retinal focal infarction.1–4
Hypersomnia is also referred to as EDS (excessive daytime sleepiness), which is a symptom that arises at any time from a tendency to get sleepy or to fall asleep when the intensity and expectations are to stay awake and wake up. In this case, EDS related neurological disorder is a condition of sleep drive caused by neurological disorders. Post stroke EDS is a condition of prolonged nap time and nighttime sleep phase followed by cerebrovascular disease depending on the degree, location of the lesion, and size.4–8
Ischemic stroke affects 70–85% of all stroke cases. The incidence of sleep disorders increases in the acute phase by around 70% and 40% in the chronic phase.9–12
In this case, the anatomy of the Ascending reticular activating system (ARAS) will be discussed. The mental stimulation of the nuclei in animals gives rise to “arousal reactions,” for example, animals that sleep become awakened. Pioneering research conducted by Moruzzi and Magoun (1949), and many subsequent studies conducted by other researchers, has provided compelling evidence that this system plays an important role in regulating the level of consciousness in humans and maintaining the wakeful sleep cycle. ARAS is a central nervous system that functions as a promoter of the sleep–wake process. This section is located in the reticular formation in the brain stem, which consists of several groups of cells and nuclei and a large number of interneurons and ascending and descending tracts that are interconnected with one another. Most of the reticular formation is located centrally or in the pectoral and mesencephalic tegmentum and extends to the medulla, hypothalamus, and thalamus. There are few cases of the mesencephalon and cerebellar infarction regarding ARAS that causes excessive sleepiness and hypersomnia. ARAS is associated with hypersomnia.4,13–15
The pathophysiology underlying ischemic stroke is the inadequate supply of oxygen to the brain tissue and glucose due to the blockage of blood vessels. Hypersomnia in stroke is classified as hypersomnia that occurs due to neurological disorders. Abnormalities underlying the occurrence of hypersomnia in stroke are not very clear, although several theories have been before. The most prevalent theory is the effect of proinflammatory cytokines that induce sleep as an evolutionary response to the promotion of rest and healing from disease, in this case, stroke. Besides, the ischemic stroke will occur mitochondrial dysfunction, associated with producing the energy needed to carry out a neuronal activity. This lack of energy can affect the work of neurotransmitters needed in the wake and awake processes, and decreased wakefulness underlies the occurrence of post-stroke hypersomnia.9,13,16–18
Bilateral lesions of the posterior region of the hypothalamus, left hemisphere, bilateral cerebral hemisphere (if the lesion is broad), tegmental mesencephalon (midbrain), thalamus, and anterior pectoral tegmentum underlie the occurrence of hypersomnolence due to involvement of the tract that forms ARAS even though only one lesion. The arousal system appears to be more related to medial lesions, and lateral lesions seem to affect the area of motor awareness. Direct lesions can cause drowsiness in the brain stem region of the reticular formation in the midline of the diencephalic structure.5,9,12,13,18
Several checks are needed, sleep quantity obtained from the history, and The Epworth Sleepiness Scale needed to diagnose hypersomnia. Treatment depends on the underlying cause. If the drowsiness persists after the basic illness was treated adequately, stimulant drugs can be given. Also, non-pharmacological therapies such as Behavioral Therapy (Sleep Hygiene) by creating quality sleep is the key to hypersomnolence therapy.
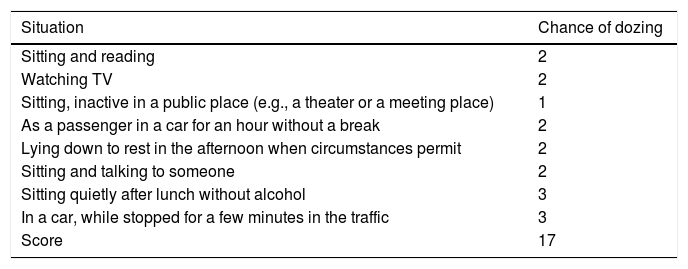
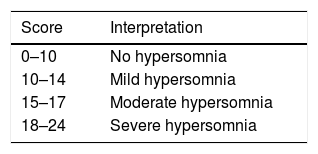
Based on this patient's Epworth Sleepiness scale of this patient on admission, the patient had a score of 17 (Table 1) meaning moderate hypersomnia (Table 2).
The result of Epworth Sleepiness Scale at admission.
| Situation | Chance of dozing |
|---|---|
| Sitting and reading | 2 |
| Watching TV | 2 |
| Sitting, inactive in a public place (e.g., a theater or a meeting place) | 1 |
| As a passenger in a car for an hour without a break | 2 |
| Lying down to rest in the afternoon when circumstances permit | 2 |
| Sitting and talking to someone | 2 |
| Sitting quietly after lunch without alcohol | 3 |
| In a car, while stopped for a few minutes in the traffic | 3 |
| Score | 17 |
Peer-review under responsibility of the scientific committee of the Technology Enhanced Medical Education International Conference (THEME 2019). Full-text and the content of it is under responsibility of authors of the article.