Technology Enhanced Medical Education International Conference (THEME 2019)
Más datosSleep problems are often found in post-stroke patients. Even though the correlation between sleep quality and stroke had been hugely proven, yet its relationship to diabetes mellitus (DM) has not been stated. This study was aimed to compare the sleep quality of patients after stroke, with and without type 2 DM.
MethodThis was a comparative study with a cross-sectional approach, involving 40 ischemic stroke patients with less than six months of onset. Samples were divided into DM and non-DM group. Sleep quality was assessed through the Pittsburgh Sleep Quality Index (PSQI). Data were analyzed by the Mann–Whitney Test and Chi-Square Test.
ResultPSQI scores in ischemic stroke patients with DM were higher than without DM, with a significant correlation between PSQI scores and DM (p<0.05).
ConclusionSleep quality is worse in an ischemic stroke patient with DM compared to those without DM.
Stroke is classically defined as a neurological deficit caused by acute focal injury of the central nervous system (CNS) by vascular causes, including cerebral infarction, intracerebral hemorrhage (ICH), and subarachnoid hemorrhage (SAH), and are the main causes of disability.1
Every year, around 800,000 people in the United States suffer a stroke, and 80% are the first attacks. Based on the results of the Basic Health Research (Riskesdas) in 2013, the highest prevalence of stroke was found in South Sulawesi (17.9%), and in 2018 the prevalence of stroke in Indonesia increased from 7% to 10.9%.2
Strokes are a significant public health problem throughout the world, and great efforts are being made to increase long-term expectations for patients. However, as a major potential contributor to stroke, sleep is not currently fully considered. For example, the recently revised guidelines for stroke rehabilitation issued by the National Institute of Clinical Excellent (NICE) provide detailed explanations of the medical, physical, and psychological needs that must be met through stroke care for inpatient and outpatient care, but these guidelines do not discuss the problem of sleep.3
Stroke and sleep disorders have a critical two-way relationship. Sleep disorders modify vascular risk factors and increase stroke risk. Strokes can also cause or worsen underlying sleep disorders.3
Sleep problems often occur after a stroke. More than half of stroke sufferers experience some type of sleep problem. The primary sleep disorders defined in the International Classification of Sleep Disorders Classification, Third Edition (ICSD-3) are Sleep-Related Breathing disorders (SRBDs), insomnia, hypersomnias of central origin, circadian rhythm sleep disorders, parasomnias, and sleep-related movement disorders.4
Treating sleep problems after stroke can improve quality of life, potentially reducing morbidity and mortality in many cases. The consequences of untreated sleep disorders can inhibit stroke rehabilitation, prolong hospital stay, and affect stroke outcomes and recurrence.3,5
Although the relationship between sleep quality and stroke is now widely proven and even its factors in overweight adolescents have also been studied,6 its association with diabetes mellitus has not been much studied. In the United States, according to The National Diabetes Statistics Report released in 2017, the prevalence rate of diabetes mellitus in 2014 was around 30, 3 million, or 9.4% of the population.
Diabetes mellitus is an independent risk factor for stroke, and several studies have also shown an increased risk of diabetes mellitus in people who have less sleep duration.7,8
This study aims to look at differences in sleep quality in ischemic stroke patients with and without type 2 diabetes mellitus (T2DM).
Research methodsA comparative study with a cross-sectional approach to 40 ischemic stroke patients onset for less than six months at the neurological clinic of RSUP. Dr. Wahidin Sudirohusodo Makassar from April to May 2019. The study sample was determined by consecutive sampling that met the inclusion criteria including 18–65 years of age, first stroke with less than six months of onset, exclusion criteria including aphasia, history of psychiatric disorders, drinking hypnotic and sedative drugs are routine and have previous sleep disorders. Subjects were divided into two groups, namely DMT2 and without DMT2. The diagnosis of ischemic stroke is made by computed tomography (CT) scan of the head, and the diagnosis of DMT2 is based on the HbA1C value. Sleep quality was measured using the Indonesian version of the Pittsburgh Sleep Quality Index (PSQI). The data of this study were analyzed by the Mann Whitney test and Chi-Square test.
ResultIn the study carried out from April to May 2019 in the Polyclinic of the Nervous Hospital of Wahidin Sudirohusodo, 40 samples were obtained. The study sample consisted of 20 ischemic stroke patients with T2DM and 20 ischemic stroke patients without T2DM. This study uses a comparative method to see differences in sleep quality in ischemic stroke patients with T2DM and without T2DM in RSUP. Dr. Wahidin Sudirohusodo.
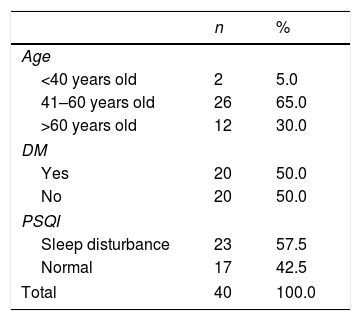
Table 1 shows the distribution of respondent characteristics. Age characteristics, the highest proportion of age 41–60 years, were 26 respondents (65.0%), and the lowest proportion of age<40 years were two respondents (5.0%). Subjects who experienced T2DM and did not experience T2DM were 20 respondents or 50.0%. While the characteristics of PSQI, who experience sleep disorders as many as 23 respondents (57.5%) and 17 respondents (42.5%), are normal.
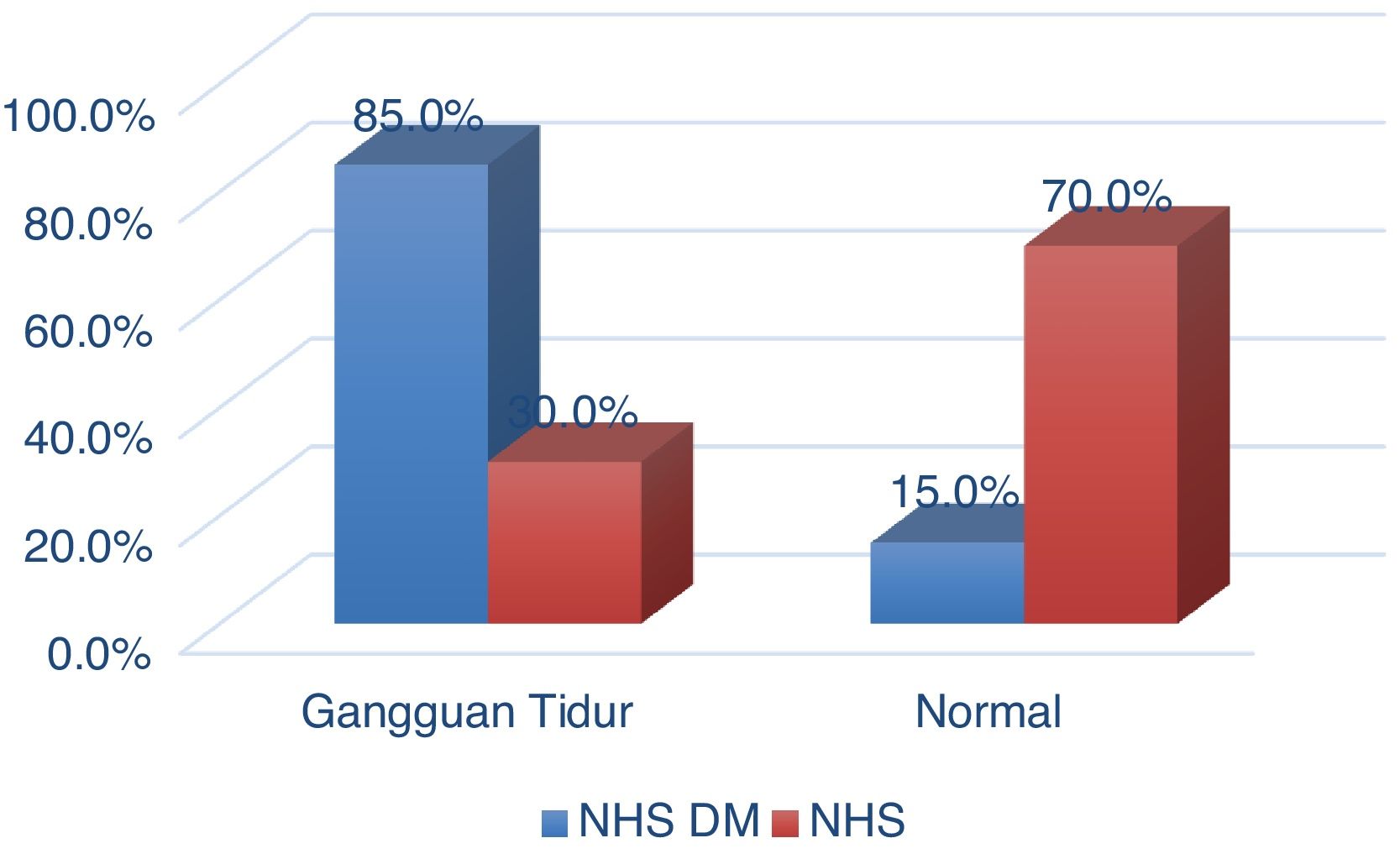
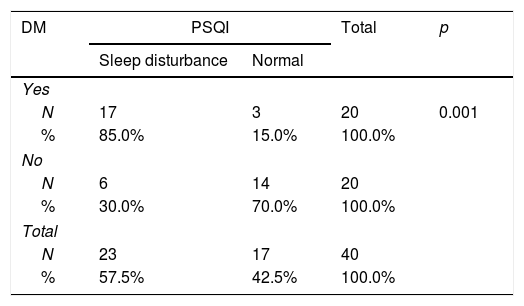
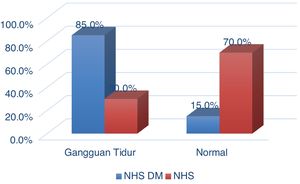
Table 2 shows the relationship between T2DM and PSQI. Twenty respondents experienced T2DM, including 17 respondents (85.0%) who had sleep disorders, and three respondents (15.0%) were healthy. While those who did not experience T2DM were 20 respondents, including those who experienced sleep disorders as many as six respondents (30.0%) and as many as 14 respondents (70.0%) were normal. Statistical test results obtained p-value (0.001) <0.05, which means there is a relationship between T2 DM and PSQI.
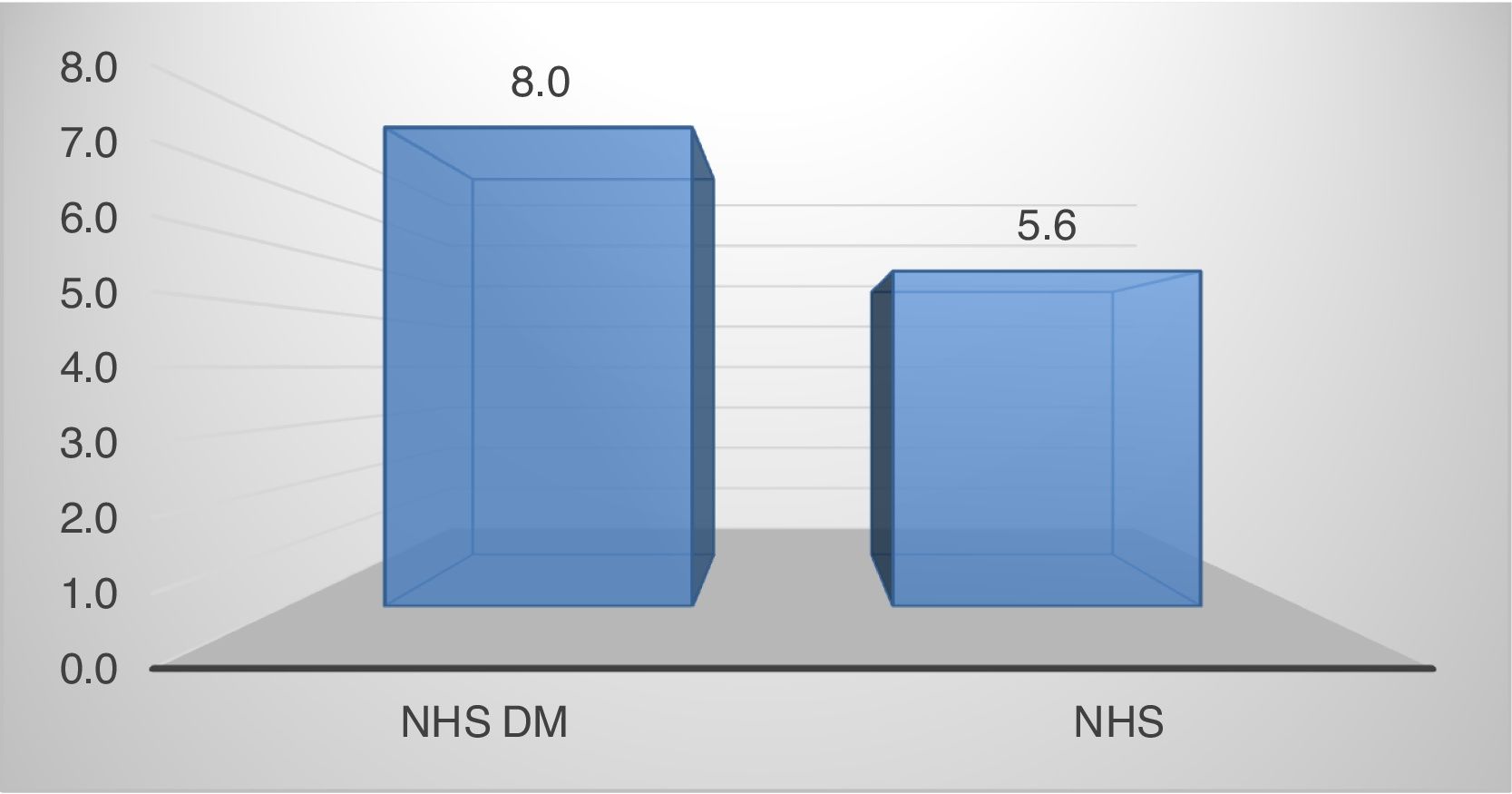
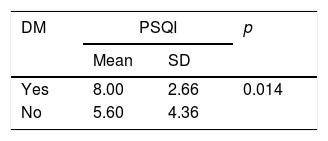
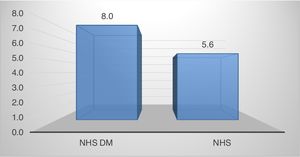
Table 3 shows the difference in PSQI scores between those who experienced DM T2 and those who did not. Those who experienced T2DM, the mean PSQI score was 8.00, while those without T2DM were 5.60. From the statistical test results obtained p-value (0.014) <0.05 which means there is a difference in the PSQI score between those who experience T2DM and those who do not experience T2DM (Figs. 1 and 2).
The results of this study found an association or difference in sleep quality between ischemic stroke patients with and without T2DM. The results of this study are in line with the research of Suh et al. (2014), which shows that diabetes mellitus is associated with disruption of nighttime sleep quality in post-stroke patients. Nighttime sleep disturbances in people with diabetes can occur due to activation of the hypothalamic-pituitary-adrenocortical axis and the sympathetic system to release extra glucocorticoids. As a result, glucose production increases while consumption decreases, thus affecting glycemic control which can cause hyperarousal and shorter sleep duration.9
In other studies, more than half of DMT2 patients tended to report “lack of sleep,” according to a poll on research conducted at the University of Pittsburgh. Patients with T2DM are more likely to have poor sleep quality.10
Patients with T2DM may experience polyuria, nocturia that interfere with sleep hygiene. Besides, psychosocial burdens due to chronic illness can disrupt emotional balance, which leads to extraordinary effects on the patient's sleep cycle. Nocturia in patients with T2DM can occur concerning polyuria, and the mechanism is solute diuresis, but it can also be associated with sleep breathing disorders, such as obstructive sleep apnea (OSA). It has been postulated that in patients with OSA, negative intrathoracic pressure, and myocardial stretching release atrial natriuretic peptide (ANP). It, in turn, causes vasodilation and inhibits aldosterone which results in excretion of excess sodium and water.10,11
ConclusionThere is a significant difference in PSQI scores in ischemic stroke with T2DM compared to ischemic stroke without T2DM. Sleep quality in patients with T2DM is worse than without T2DM.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the Technology Enhanced Medical Education International Conference (THEME 2019). Full-text and the content of it is under responsibility of authors of the article.