Stroke is acknowledged as a devastating complication post coronary artery bypass grafting surgery (CABG), that may reduce the quality of life and increase mortality. The incidence of post-CABG stroke results in more hospital mortality, longer times of hospital stays, and raises the costs of hospital and rehabilitative support. Having knowledge about risk factors of stroke after CABG could help to define the best approach to reduce post-CABG strokes.
Materials and methodsIn this study, we reviewed the risk factors associated with stroke after CABG and the strategies for reducing the risk of stroke.
ResultAccording to the evaluation of this study, the incidence rate of stroke after CABG was between 1.2% and 4.2%. The most prevalent risk factors for stroke after CABG are advanced age, previous stroke, atrial fibrillation, carotid artery disease, and diabetes mellitus.
ConclusionMoreover, off-pump coronary artery bypass graft and epiaortic ultrasonography have a positive effect on reducing the incidence of stroke post-CABG.
El accidente cerebrovascular se reconoce como una complicación devastadora posterior a la cirugía de injerto de derivación de la arteria coronaria (CABG), que puede reducir la calidad de vida y aumentar la mortalidad. La incidencia de accidente cerebrovascular posterior a la CABG da como resultado una mayor mortalidad hospitalaria, estancias hospitalarias más prolongadas y eleva los costos del apoyo hospitalario y de rehabilitación. Tener conocimiento sobre los factores de riesgo del accidente cerebrovascular después de la CABG podría ayudar a definir el mejor enfoque para reducir los accidentes cerebrovasculares posteriores a la CABG.
Material y métodosEn este estudio, revisamos los factores de riesgo asociados con el accidente cerebrovascular después de la CABG y las estrategias para reducir el riesgo de accidente cerebrovascular.
ResultadosDe acuerdo con la evaluación de este estudio, la tasa de incidencia de accidente cerebrovascular después de CABG fue de 1,2% a 4,2%. Los factores de riesgo más prevalentes para el accidente cerebrovascular después de la CABG son la edad avanzada, el accidente cerebrovascular previo, la fibrilación auricular, la enfermedad de la arteria carótida y la diabetes mellitus.
ConclusionesAdemás, el injerto de derivación de la arteria coronaria sin circulación extracorpórea y la ecografía epiaórtica tienen un efecto positivo en la reducción de la incidencia de accidente cerebrovascular después de la CABG.
In spite of the improvements in anesthesia and cardiac surgery techniques, stroke remains the most prevalent neurologic complication after coronary artery bypass grafting surgery (CABG).1 Stroke is acknowledged as a devastating complication post-CABG, that may reduce the quality of life and increase mortality.2 The prevalence of stroke after CABG is reported to vary from 1.5% to 5.2%.3 The incidence of post-CABG stroke result in more hospital mortality, longer times of hospital stays, and raises the costs of hospital and rehabilitative support. It was reported that stroke after cardiac surgery had 6-folds higher 30-day mortality.4
It was reported that the risk of post-CABG stroke peaked at the second post-operative day and stabilized to a constant hazard after the first-week post-CABG and up to 30 days. It was shown that about 69% of incidences of stroke are recognized during the first 2 days post-surgery. In addition, the rate of 2%–4% early stroke incidence was reported during the 30 days of the surgery.3 Most of the strokes happen during the first 48 h after surgery, however, delayed stroke can happen, typically in 30 days after surgery.5
Stroke might happen intraoperatively or afterward. Therefore, there are 2 stroke types with different mechanisms; the intraoperative or early stroke happens mainly due to aortic manipulation and atheroembolism, while the post-operative or delayed stroke is generally associated with post-operative cerebral vascular disease or atrial fibrillation.6 It was also shown that cardioembolic stroke and atherothrombotic stroke are the subtypes of ischemic infarct with the highest in-hospital mortality.7
It seems that hemorrhage and ischemia are the 2 mechanisms that are accountable for post-CABG stroke.3 Hemorrhage is related to hypertension as well as reperfusion of the infarcted zone. Ischemia may be a result of embolic events, systemic hypoperfusion, and thromboembolism of intra/extracranial vessels. The interaction between hypoperfusion and embolism is considered to be the main reason for post-operative stroke.3 Moreover, post-CABG disorder in the neuronal metabolism in the brain, which is possibly due to inflammatory processes activation, is reported in patients.8
Differences in the rate of stroke after cardiac surgery are probably related to variables, including older age, gender, comorbid diseases, the recent history of myocardial infarction, unstable angina, a previous history of stroke, and carotid diseases. Having knowledge about risk factors of stroke after CABG could help to define the most suitable pre- and post-operative evaluations and interventions to reduce post-CABG strokes and develop post-CABG management. In this review, we summarize the risk factors associated with stroke after CABG. Moreover, we evaluated the strategies for reducing the stroke risk after CABG.
MethodIn this review study, all articles on post-CABG stroke were examined from the year 1996 to March 2020. Articles were searched through databases such as PubMed, Web of Science, Scopus, Google Scholar, Science Direct, and Cochrane library using the keywords “Stroke”, “CABG”, “coronary artery bypass surgery”, and “post-CABG stroke”. A total of 153 articles were extracted in an initial search. After reviewing the abstract of these articles, finally, 62 articles that met the necessary criteria of the present review were selected and evaluated completely.
Epidemiology of stroke after CABGWith regard to the Society of Thoracic Surgeons CABG Adult Cardiac Surgery Database, the rate of stroke following CABG is 1.3%.9 In a recent study by Yamamoto et al. on 14 867 patients who underwent first coronary revascularization, the risk of stroke was defined as 2.13% after CABG and 0.96% after percutaneous coronary intervention (PCI), and the proportions of a major stroke at hospital discharge were defined 77% after CABG and 68% after PCI.10 In Mao et al.’s systematic review on 14 studies, the rate of stroke post-CABG was 1.1%–5.7% and almost 37%–59% of them happened early.11 In the Casto et al.’s study, the rate of stroke was 4.2% among 519 consecutive patients who underwent cardiac surgery.12 According to Bucerius et al.’s study on Jan Bucerius patients who underwent cardiac surgery, the incidence rate of stroke was 3.8% after CABG and 1.9% after beating-heart CABG.4
Risk factors for post-CABG strokeAdvanced ageThe incidence of stroke after CABG increases with age about 6-fold and advanced age is considered as an indicator of raised atherosclerotic burden. The post-CABG stroke risk is higher in older patients with cardiovascular disease than younger patients with no risk factors for cardiovascular disease.13 Mérie et al. reported a moderate increase in the risk of stroke after CABG with an age increase.14 In Yamamoto et al.’s study on patients from the CREDO-Kyoto PCI/CABG Registry Cohort-3, advanced age is reported as an independent risk factor of periprocedural stroke post-CABG and PCI.10 In a study by Aribox et al., congestive heart failure, chronic renal disease, previous cerebrovascular disease, and atrial fibrillation were significantly associated with ischemic stroke in 85 years old or older patients.15
Acute myocardial infarction (AMI)Studies have shown that undergoing CABG in the acute phase after AMI has been recognized as a risk factor for ischemic stroke. Besides, the risk of stroke was increased while the CABG was done later after AMI, however, the occurrence rate was noticeably lower with late CABG in comparison to early CABG.16 In another study by Anwar Shah et al., MI was related to the increased occurrence of stroke after CABG.17 In a study by Åström et al., in the early cohort, the rates of stroke were respectively 15.8% and 10.9% in patients with and without CABG, and in the late cohort, the rates were 4.0% and 2.3%, in patients with and without CABG, respectively.16 The increased risk of stroke after AMI seems to be related to pro-thrombotic factors, including inflammation, platelet, and sympathetic activation.18
Post-operative atrial fibrillationPost-operative atrial fibrillation happens in about 30% of CABG patients before they discharge from the hospital and is an important stroke predictor.19 A meta-analysis by Megens et al. reported that the risk of stroke in CABG patients with post-operative atrial fibrillation remained meaningfully higher during a 2 years follow-up in comparison to patients without post-operative atrial fibrillation.20 Lahtinen et al. study reported that post-operative atrial fibrillation associated with stroke after CABG occurred in around one-third of patients, and the meantime was 21 h.21 In another study by Kollar et al. from 6 CABG patients with AF, 3 strokes happened within 1 week after conversion to normal sinus rhythm. One patient with pre-operative and AF who underwent emergency CABG woke up with a stroke.22
Diabetes mellitusIn a study by Anwar Shah et al., diabetes mellitus was related to the increased occurrence of stroke after CABG.17 In another study by de Oliveira et al., it was shown that diabetes mellitus is an important factor of higher risk of stroke during the first 24 h after CABG.23 Casto et al. also showed that diabetes was a statistically significant (P = .04; OR 2.61) risk factor for stroke after CABG.12 Baker et al.’s study on 4380 patients who underwent CABG, diabetes was demonstrated as a risk factor for stroke after CABG.24 In another study by Bucerius et al., diabetes was determined as a predictor of stroke after cardiac surgery.4
Previous history of strokeThe occurrence of post-operative stroke in patients who underwent CABG and had a history of stroke was significantly higher than in patients who had no prior history of stroke.25 Mao et al. review study on 14 studies showed that prior cerebrovascular disease or stroke is a consistent independent predictor for stroke after CABG.11 Cao et al. showed that unstable angina, post-operative AF, post-operative hypotension, and left ventricular ejection fractions (LVEF)≤50% are independent risk factors for post-CABG recurrent stroke in patients with a former history of stroke.26
Atherosclerosis of the ascending aortaCardiac surgery commonly includes manipulation of the ascending aorta by arterial cannulation, cross-, and side-clamping and these may raise the chance of embolization of the atherosclerotic substances to the brain.27 Linden et al. demonstrated that patients who had atherosclerosis in the ascending aorta had an 8.7% occurrence of stroke after cardiac surgery and the risk is associated with the existence, place, and size of the disease.28 It was reported that atherosclerosis of the ascending aorta (ascending aortic wall thickness of ≥4 mm) was a risk factor for post-CABG strokes.29 In the Asenbaum et al.’s study, all patients with CABG-related stroke had atherosclerotic disease of the ascending aorta and the stroke rate was significantly related to the existence and degree of atherosclerotic disease.30
Cerebral artery atherosclerosisIn the Lee et al.’s study, it was found that cerebral atherosclerosis was closely associated with the incidence of stroke after CABG. It is an independent risk factor for strokes and the reason for a substantial proportion of it. They showed that intracranial, extracranial, and extracranial/intracranial cerebral atherosclerosis were significantly related to stroke.31
Low cardiac output syndromeLow cardiac output syndrome is a significant predictor of post-CABG stroke.32 In Likosky et al.’s study on 11 825 patients who underwent CABG, it was shown that low cardiac output syndrome augmented the stroke risk with an OR of 3.32 In Stamou et al.’s study on 16 528 patients who underwent CABG during 1989–1999, low cardiac output was associated with post-operative stroke.33
Carotid diseaseDashe et al. in their study revealed that the post-CABG stroke risk was raised in patients with severe extracranial carotid stenosis or occlusion and the stroke incidence had a positive association with the degree of carotid stenosis.34 Lescan et al. also suggested that asymptomatic contralateral carotid stenosis is a risk factor for stroke after cardiac surgery in patients who had carotid occlusion before cardiac surgery.35 Naylor et al. in a review study reported that the stroke risk raised to 3% in CABG patients with unilateral carotid stenosis, 5% in patients with bilateral carotid stenosis, and 7%–11% in those with carotid occlusion.36
Prolonged use of inotropesIn Likosky et al.’s study on patients who underwent CABG, it was shown that the long use of inotropes augmented the stroke risk with an OR of 5.32
Systemic arterial hypertensionIn de Oliveira's study, it was revealed that systemic arterial hypertension is a determinant factor of a higher risk of stroke during the first 24 h of the post-operative period after CABG.23 In another study by Kangasniemi et al., hypertension was reported as a risk factor for stroke after CABG.37 In Bucerius et al.’s study also, hypertension was defined as a predictor of stroke after cardiac surgery.4
Prolonged cardiopulmonary bypassIn a study, it was shown that cardiopulmonary bypass (CPB) for 90–113 min (OR = 1.59, P = .022) and for 114 min or more (OR = 2.36, P < .001) were a significant predictor for stroke after CABG.38 A systematic review by Mao et al. reported that prolonged cardiopulmonary bypass time, 2 h, had a consistent positive correlation with post-CABG stroke.11 Santos et al. reported that cardiopulmonary bypass for more than 110 min is a risk predictor for stroke after cardiac surgery.39 In another study by Bucerius et al. on 16 184 patients who underwent cardiac surgery, CPB time >2 h is a predictor for stroke after surgery.4
Platelet countsIn a Karhausen et al. study, the occurrences of post-CABG stroke were 1.09%, 1.50%, and 3.02%, respectively, for platelet counts more than 150 × 10/L, 100–150 × 10/L, and less than 100 × 10/L. Each 30 × 10/L reductions in platelet counts resulted in a 12% increase in the stroke rate. Also, 2-folds increase in the stroke rate was observed in patients with moderate to severe thrombocytopenia. In studies, it was reported that a significant relation between post-operative nadir platelet counts and the mortality rate after CABG surgery.40
BUNIn a recent study by Arnan et al., acutely raised post-operative BUN appeared as the most potent predictor of strokes after cardiac surgery including CABG (OR, 2.37 for every 25% rise in BUN, with ROC AUC of 0.855).41
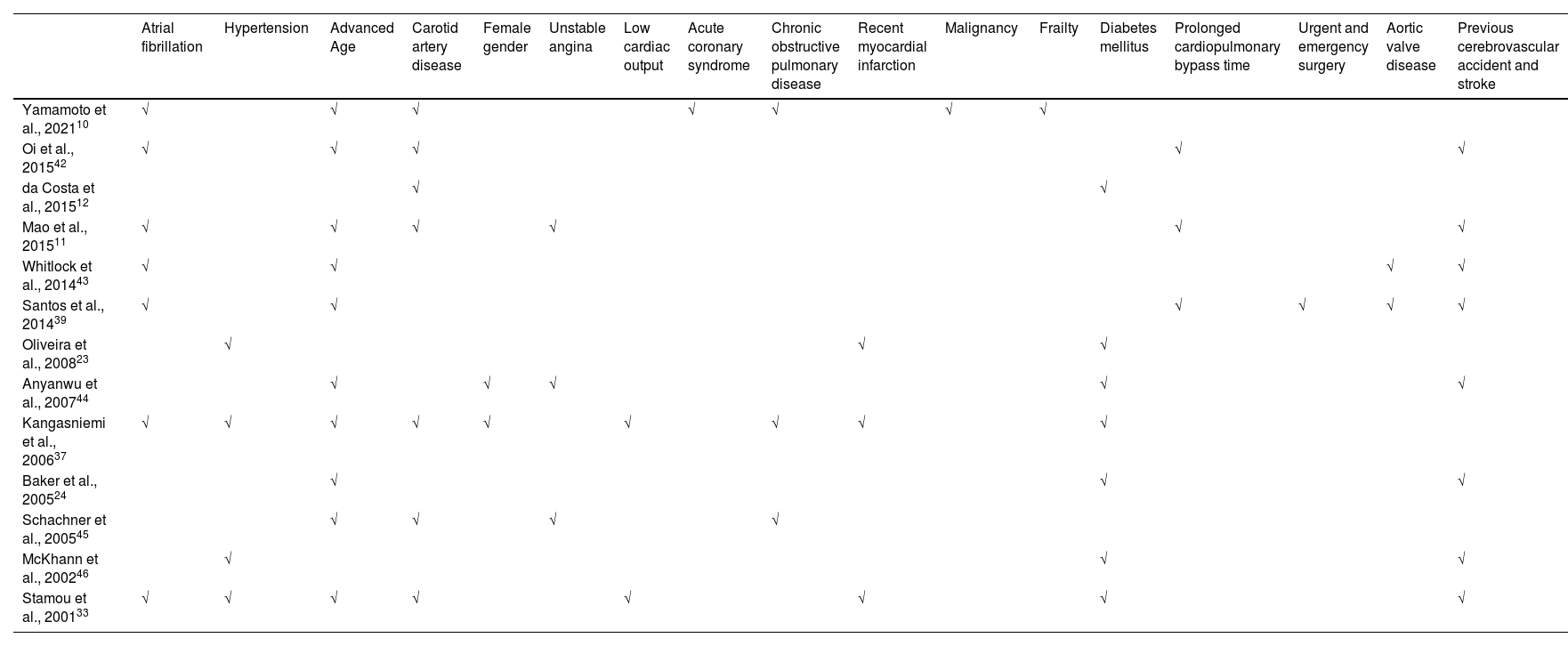
Table 1 shows the risk factors for stroke after CABG according to the search in the review, systematic review, and original published studies.
Risk factors for post-CABG stroke.
| Atrial fibrillation | Hypertension | Advanced Age | Carotid artery disease | Female gender | Unstable angina | Low cardiac output | Acute coronary syndrome | Chronic obstructive pulmonary disease | Recent myocardial infarction | Malignancy | Frailty | Diabetes mellitus | Prolonged cardiopulmonary bypass time | Urgent and emergency surgery | Aortic valve disease | Previous cerebrovascular accident and stroke | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yamamoto et al., 202110 | √ | √ | √ | √ | √ | √ | √ | ||||||||||
| Oi et al., 201542 | √ | √ | √ | √ | √ | ||||||||||||
| da Costa et al., 201512 | √ | √ | |||||||||||||||
| Mao et al., 201511 | √ | √ | √ | √ | √ | √ | |||||||||||
| Whitlock et al., 201443 | √ | √ | √ | √ | |||||||||||||
| Santos et al., 201439 | √ | √ | √ | √ | √ | √ | |||||||||||
| Oliveira et al., 200823 | √ | √ | √ | ||||||||||||||
| Anyanwu et al., 200744 | √ | √ | √ | √ | √ | ||||||||||||
| Kangasniemi et al., 200637 | √ | √ | √ | √ | √ | √ | √ | √ | √ | ||||||||
| Baker et al., 200524 | √ | √ | √ | ||||||||||||||
| Schachner et al., 200545 | √ | √ | √ | √ | |||||||||||||
| McKhann et al., 200246 | √ | √ | √ | ||||||||||||||
| Stamou et al., 200133 | √ | √ | √ | √ | √ | √ | √ | √ |
Risk factors for early stroke were including older age, high level of pre-operative creatinine, amount of aortic atherosclerosis, prior neurological event, and long CBP time.2 Risk factors related to delayed stroke are including female sex, post-operative atrial fibrillation, unstable angina, prior cerebrovascular disease, and inotropic support requirement.2 It was reported that prior neurological events, diabetes, combined endpoints of low cardiac output, and aortic atherosclerosis were also risk factors for delayed post-CABG stroke. In another study at age ≥70, chronic obstructive pulmonary disease, carotid artery disease, and a maximum rising aortic wall thickness of ≥4 were determined as the risk factors of late post-CABG stroke.45
Mechanisms of stroke after CABGEmbolization and hypoperfusion are considered as the mechanisms of neurological complications including stroke after CABG.
EmbolizationAtherosclerotic debris, air, fat, and surgical debris are considered as the origin of embolism in cardiac surgery. It was shown that micro-emboli that are defined by transcranial Doppler in the middle cerebral arteries are associated with neurological injuries after cardiac surgery. It is also shown that the quality of embolism has a role in brain injury and not its amount.47
Recently indirect pieces of evidence show that small capillary arteriolar dilations (SCADs), small lipid emboli, that found in the autopsy of patients who died after cardiac surgery, may be related to the neurological injuries after cardiac surgery. SCADs can be reproduced in canine models of cardiopulmonary bypass. SCADs are supposed to be originated from primarily lipid emboli during cardiopulmonary bypass procedure.48
Macro-emboli which were produced as a result of aortic atherosclerosis and atrial fibrillation suggested being associated with post-operative stroke.49
HypoperfusionSignificant blood pressure variations during surgery can raise the probability of post-operative neurological injuries and the risk of stroke. It was shown that a decrease in systolic blood pressure to ≤50 mm Hg for ≥10 min increased neurological complications after cardiac surgery.50 Since the cerebral perfusion pressures >50 mm Hg are tolerable for the brain.51 However, this may not be correct for patients with intra- or extracranial stenosis or in those with chronic hypertension. Pulse pressure, which is the vascular stiffness marker, was also recognized as a stroke predictor after cardiac surgery.52
It was theorized that embolization and hypoperfusion have a synergistic effect in neurological injury. Since hypoperfusion reduces the emboli washout, which leads to injury in the watershed areas of the brain.53
Reducing the risk of stroke after CABG by improvement in techniquesIn recent years, some techniques have been advanced to improve neurological complications after cardiac surgery.
Epiaortic ultrasonographyIt is believed that epiaortic ultrasonography reduces the neurological outcomes after cardiac surgery by decreasing cerebral embolization.54 Some studies have demonstrated a decrease in the incidence of stroke in patients who experienced surgical technique alterations according to the consequences of epiaortic scanning.55 Rosenberger et al. reported that in the CABG patients managed with Epiaortic ultrasonography showed a lower occurrence of stroke (1.4% vs. 1.6%).56 Zingone et al. also showed that the total and early stroke rate reduced in a CABG cohort after using the epiaortic imaging.57
Off-pump coronary artery bypass graftStudies have recommended a relation between off-pump CABG and reduction in stroke reduction. It is assumed that off-pump coronary artery bypass graft surgery reduces the risk for brain injury via decreasing cerebral embolization and inflammatory responses.54 In a study on more than 42 000 patients, a 35% decrease was seen in the stroke risk in patients treated with off-pump CABG in comparison to patients who were treated with on-pump CABG.58 Nishiyama et al.‘s study showed that off-pump CABG decreased the occurrence of stroke mostly by reducing early strokes; but, the delayed stroke risk was not different in patients who underwent off- and on-pump CABG.59 In contrast, some studies showed no difference between the risk of stroke in off- and on-pump CABG.60 Therefore, the result is controversial.
ConclusionAlthough there were methodological and clinical differences in the evaluated studies, according to the evaluation of the present study the most prevalent risk factors for stroke after CABG are advanced age, previous stroke, atrial fibrillation, carotid artery disease, and diabetes mellitus. In addition, off-pump coronary artery bypass graft and epiaortic ultrasonography have a positive effect on reducing the incidence of stroke post-CABG. These results may assist to advance the selection of patients for CABG and patient management after CABG.
LimitationsOne of the limitation of the present study was access to full text of some articles and they were removed from the study.