Whipple disease is a multisystem disease caused by bacterial infection with Tropheryma whipplei. It was first described by George H. Whipple in 1907 as an “intestinal lipodystrophy” in a patient with weight loss, polyarthritis, diarrhoea, malabsorption, and mesenteric lymphadenitis.1 Presence of neurological symptoms in the absence of systemic manifestations is rare.2
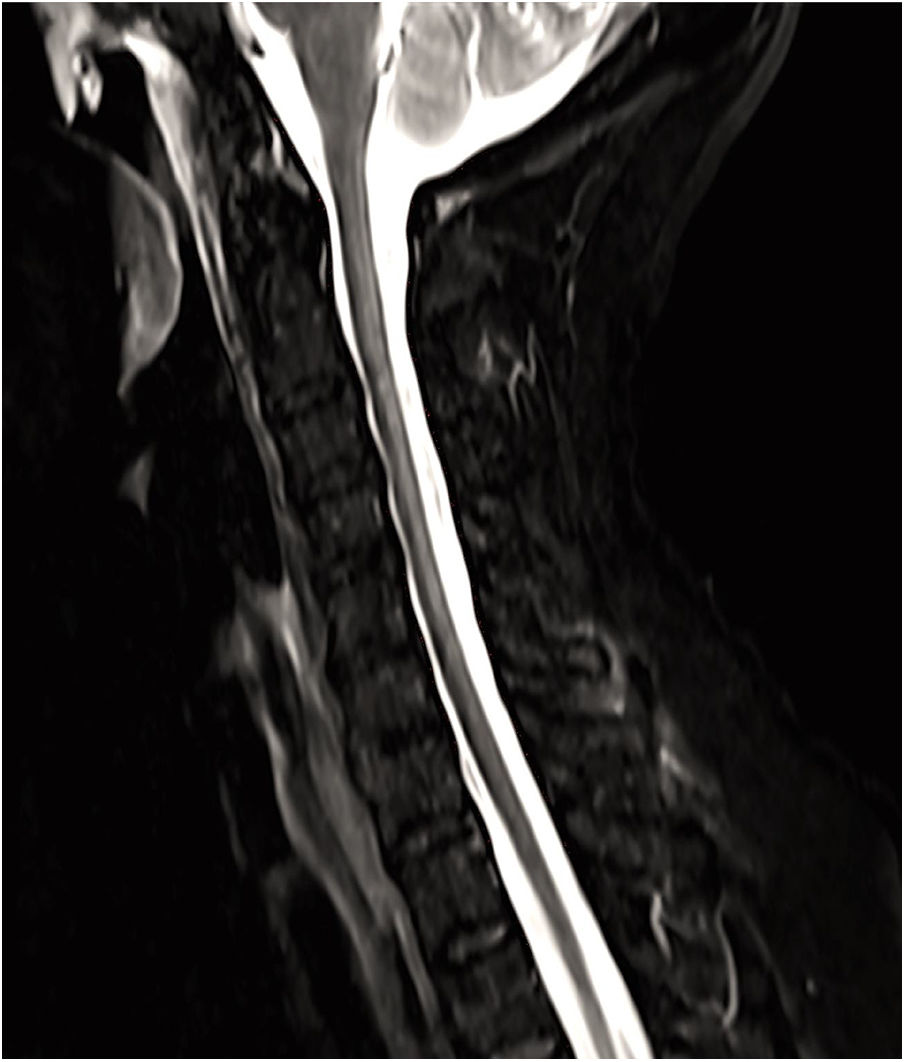
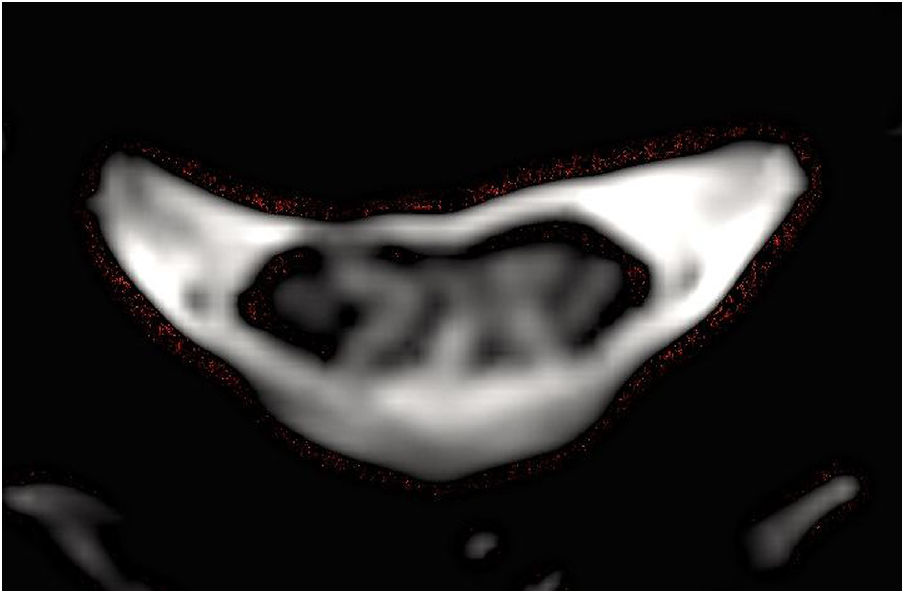
We present a case of Whipple disease manifesting with isolated symptoms of spinal cord involvement. Our patient was a 66-year-old woman who consulted due to a one-year history of gait alterations, with no associated symptoms. The neurological examination revealed decreased deep sensitivity in the lower limbs, with no pyramidal signs; results were normal for all other areas. A somatosensory evoked potentials study revealed injury to the somatosensory pathway at the level of the posterior column. A non-contrast, T2-weighted spinal cord MRI scan performed to rule out myelopathy revealed a hyperintense lesion in the posterior column between C2 and T1, with no associated oedema (Figs. 1 and 2); no brain lesions were identified. A blood analysis including a complete biochemistry study and immunological tests found no evidence of autoimmune, systemic, or metabolic diseases, nutritional deficiencies, etc. Given that differential diagnosis includes viral and bacterial infections, we requested a microbiological analysis of a blood sample; PCR findings were positive for T. whipplei. Biochemical, microbiological, immunological, and cytological analyses of the CSF yielded normal results, with the exception of positive PCR results for T. whipplei. The pathogen was not detected in the faeces or saliva. An additional PCR test performed 15 days later also yielded positive results for T. whipplei. The patient received intravenous ceftriaxone for 14 days, showing good clinical response. Long-term treatment with oral trimethoprim-sulfamethoxazole achieved marked improvements in gait. An MRI scan performed several months later revealed stability of the spinal cord lesion. Subsequent blood and CSF PCR tests yielded negative results.
Whipple disease is an infectious disease associated with multisystem manifestations, most frequently affecting the gastrointestinal system and joints. Although the precise incidence is unknown,3 central nervous system involvement is frequent, appearing in 43% of cases4; however, presence of neurological symptoms in isolation occurs in only 5% of patients.5
Neurological symptoms are nonspecific and highly variable, ranging from impaired consciousness to cognitive impairment, epileptic seizures, myoclonus, cerebellar or hypothalamic involvement, cranial and peripheral neuropathies, and extrapyramidal symptoms.5,6 Oculomasticatory myorhythmia and oculofacial-skeletal myorhythmia are pathognomonic of Whipple disease.7,8
Although some cases have been described of myelopathy associated with other inflammatory lesions in different parts of the central nervous system (eg, the brain, optic chiasm, posterior fossa), as in the patient described by Kremer et al.,9 presentation in the form of isolated myelopathy is even rarer. The first case was reported by Clarke et al.10 in 1998 in a 62-year-old patient; Messori and Salvolini11 and Messori et al.12 subsequently described the case of a 65-year-old patient with relapsing-remitting cervico-thoracic myelopathy due to Whipple disease who subsequently developed brain lesions. In 2005, Schröter et al.13 described the case of a 50-year-old patient with a cervical spinal cord lesion extending from the cervicomedullary junction to the upper thoracic region, without cerebral involvement; the patient responded well to antibiotic therapy against T. whipplei, which was detected in a blood PCR test. To our knowledge, our patient is the fourth reported case (and the first in Spain) of Whipple disease manifesting as isolated myelopathy affecting the posterior column. The cases described bear certain similarities, including age of presentation (between the sixth and seventh decades of life), symptoms of chronic progressive myelitis, extensive cervical spinal cord involvement with MRI hyperintensity, and marked improvement with antibiotics.
Differential diagnosis should include other bacterial, viral, and parasitic infections; such demyelinating diseases as multiple sclerosis, neuromyelitis optica, and acute disseminated encephalomyelitis; vascular disease (ischaemia, haemorrhage); tumours or paraneoplastic syndromes; and systemic (eg, systemic lupus erythematosus, Behçet disease, Sjögren syndrome, sarcoidosis) or deficiency diseases (vitamin deficiency).
The limited published evidence on the topic and the nonspecific nature of the symptoms may hinder diagnosis and delay treatment. Neurological symptoms may constitute the initial manifestation of Whipple disease, with other more characteristic symptoms appearing at later stages.14 In any case, the lack of microbiological confirmation should not delay treatment in cases of suspected Whipple disease. Targeted antibiotic therapy for bacterial infection is recommended before spinal cord biopsy is performed.
In conclusion, symptoms of spinal cord involvement are infrequent in Whipple disease. Therefore, infection with T. whipplei should be considered in patients with isolated myelopathy of unknown cause, even in the absence of systemic symptoms; this requires a high level of clinical suspicion. Early diagnosis enables the provision of effective treatment able to resolve symptoms and even to prevent lesions from spreading to other organs or regions of the nervous system; Whipple disease is potentially fatal if the patient does not receive targeted treatment.
FundingThis study has received no specific funding from any public, private, or non-profit organisation.
Please cite this article as: Pérez Álvarez ÁI, Morís de la Tassa G. Mielopatía cervical como forma de presentación de la enfermedad de Whipple. Neurología. 2020;35:583–585.