Idiopathic intracranial hypertension is a disorder characterised by increased intracranial pressure without evidence of an expansive intracranial process or cerebrospinal fluid cytochemical alterations.
Patients and methodWe reviewed the medical records of patients with idiopathic intracranial hypertension admitted to our hospital between 1999 and 2009 and who met the modified Dandy criteria. We collected the following data: age, body mass index (BMI), outlet pressure of cerebrospinal fluid, cardiovascular history, imaging studies, treatment, and outcome.
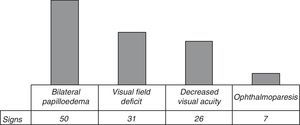
ResultsWe analysed 61 patients (19 males and 42 females) with a mean age of 35.38 years. A BMI above the normal range was determined for 72.13% of the patients, although 47.37% of males showed normal weight. Fifty per cent of patients had a cardiovascular risk factor, especially dyslipidaemia, hypertension, and contraceptive drugs in women. Headache was the main presenting symptom, followed by visual field defects and other visual disturbances. Bilateral papilloedema was present in 81.96% of the patients.
ConclusionsThe approximate incidence is 1.2/100 000 individuals/year. The condition is more common in young women with higher body weight and it is also associated with contraceptive drugs. Headache with bilateral papilloedema and impaired visual acuity stand out as the main symptoms. An interesting finding from this study is that male patients had a lower BMI, a lower incidence of headache and increased visual impairment.
La hipertensión intracraneal idiopática es una entidad caracterizada por el aumento de la presión intracraneal sin evidencias de proceso expansivo intracraneal o alteraciones citoquímicas del líquido cefalorraquídeo.
Pacientes y métodoSe revisaron las historias clínicas de los pacientes con hipertensión intracraneal idiopática ingresados en nuestro hospital entre 1999 y 2009, y que cumplían los criterios modificados de Dandy. Se recogieron datos de edad, índice de masa corporal (IMC), presión de salida de líquido cefalorraquídeo, antecedentes cardiovasculares, pruebas de imagen, tratamiento y evolución.
ResultadosSe analizaron 61 pacientes (19 hombres y 42 mujeres), con una media de edad de 35,38 años. El 72,13% de los pacientes mostraban aumento del IMC. Cabe destacar que el 47,37% de los varones mostraban normopeso. El 50% de los pacientes presentaban algún factor de riesgo cardiovascular, destacando la dislipidemia, la hipertensión arterial y el tratamiento con anticonceptivos en las mujeres. La cefalea era el principal síntoma de presentación, seguido de las alteraciones campimétricas y otros defectos visuales. El 81,96% de los pacientes presentaban edema de papila bilateral.
ConclusionesLa incidencia aproximada es de 1,2/100.000 habitantes/año, siendo más frecuente en mujeres jóvenes con aumento de peso y asociado a la toma de tratamiento anticonceptivo. Destaca la cefalea, con edema de papila bilateral y alteraciones de la agudeza visual como síntomas principales. Un dato interesante aportado por este trabajo es el menor IMC que se muestra en el sexo masculino, así como la menor presencia de cefalea y mayor afectación visual.
Idiopathic intracranial hypertension (IIH) is a disorder characterised by an increase in intracranial pressure with no evidence of intracranial pathology. IIH was first described by Quincke. Dandy proposed the first diagnostic criteria for IIH in 1937 and Smith would later modify them in 1985.1,2 Diagnostic criteria are generally based on signs and symptoms of intracranial hypertension and on increased intracranial pressure with no anomalies in the cerebrospinal fluid (CSF) and normal neuroimaging scans.2,3
Annual incidence in the general population4 is 1-3 per 100 000 inhabitants aged between 15 and 44. This disorder is more frequent in young and obese women, with a male/female ratio of 1:8.3–7
The most frequently reported symptoms include headache (with no pathognomonic characteristics), nausea and vomiting, amaurosis fugax, visual field defects, diplopia, photopsia, and pulsatile tinnitus. Examination of the fundus of the eye normally reveals unilateral or bilateral papilloedema, and neurological examination usually yields normal results, with the exception of ophthalmoparesis of the sixth cranial nerve.4,8
There are cases of atypical pseudotumor cerebri; this is the term used for cases that fulfil each of the modified Dandy criteria in the absence of papilloedema.9,10
The aim of this study is to determine clinical and epidemiological characteristics of IIH among patients in our setting.
Patients and methodsWe performed retrospective analysis of medical records from patients diagnosed with IIH who were admitted to the neurology department at Hospital Universitario de Nuestra Señora de Candelaria, between January 1999 and 31 December 2009. This is a tertiary care hospital that covers a healthcare district containing approximately 500 000 inhabitants.
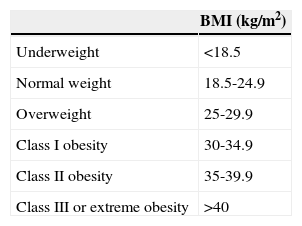
We selected patients who met the modified Dandy criteria2 (Table 1). For all patients, we collected data regarding age, sex, arterial hypertension, diabetes mellitus, dyslipidaemia, heart disease, tobacco use, relevant neurological history, and use of oral contraceptives. Since this was a retrospective analysis, no data regarding recent weight gain could be obtained. However, we were able to record presence/absence of obesity and patients’ body mass index (BMI) according to current WHO criteria (Table 2). We also estimated initial CSF opening pressure, measured in cmH2O. Cranial computed tomography was performed for all patients, and magnetic resonance imaging for 96.72%. Magnetic resonance angiography was necessary in 18.03% of the patients due to the atypical characteristics of the symptoms. Data for readmission, recurrence, resistance to treatment, and surgical treatment during subsequent follow-up were also included in the analysis.
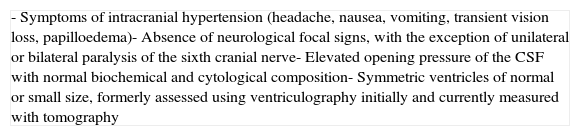
Modified Dandy diagnostic criteria
| - Symptoms of intracranial hypertension (headache, nausea, vomiting, transient vision loss, papilloedema)- Absence of neurological focal signs, with the exception of unilateral or bilateral paralysis of the sixth cranial nerve- Elevated opening pressure of the CSF with normal biochemical and cytological composition- Symmetric ventricles of normal or small size, formerly assessed using ventriculography initially and currently measured with tomography |
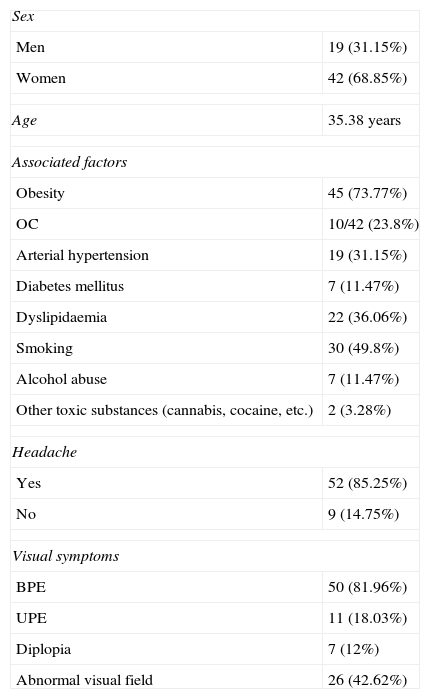
We analysed 61 patients of whom 19 were men (31.15%) and 42 were women (68.85%). Their mean age was 35.38 years, with no significant variations between sexes (Table 3).
General characteristics
| Sex | |
| Men | 19 (31.15%) |
| Women | 42 (68.85%) |
| Age | 35.38 years |
| Associated factors | |
| Obesity | 45 (73.77%) |
| OC | 10/42 (23.8%) |
| Arterial hypertension | 19 (31.15%) |
| Diabetes mellitus | 7 (11.47%) |
| Dyslipidaemia | 22 (36.06%) |
| Smoking | 30 (49.8%) |
| Alcohol abuse | 7 (11.47%) |
| Other toxic substances (cannabis, cocaine, etc.) | 2 (3.28%) |
| Headache | |
| Yes | 52 (85.25%) |
| No | 9 (14.75%) |
| Visual symptoms | |
| BPE | 50 (81.96%) |
| UPE | 11 (18.03%) |
| Diplopia | 7 (12%) |
| Abnormal visual field | 26 (42.62%) |
OC, oral contraceptives; BPE, bilateral papilloedema; UPE, unilateral papilloedema.
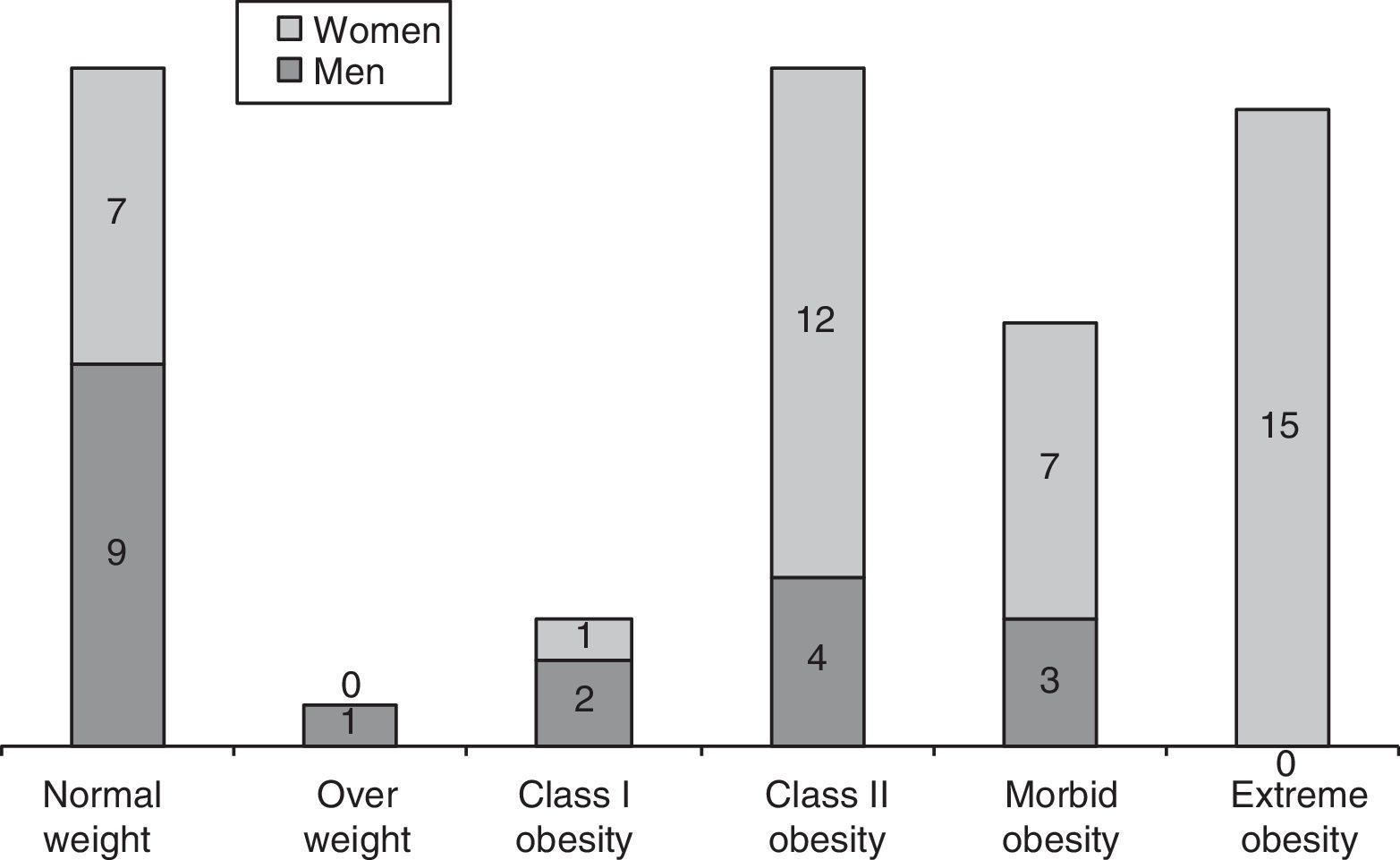
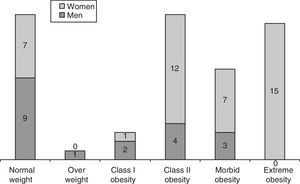
BMI > 25 was registered in 44 patients (73.77%). Among patients displaying a BMI>40, we found a male/female ratio of 1:7. Nine (47.37%) out of the 19 men were in the normal weight range, compared to only 7 (16.66%) out of the 42 women. Therefore, the male/female ratio in the normal weight group is 1:2.84 (Fig. 1).
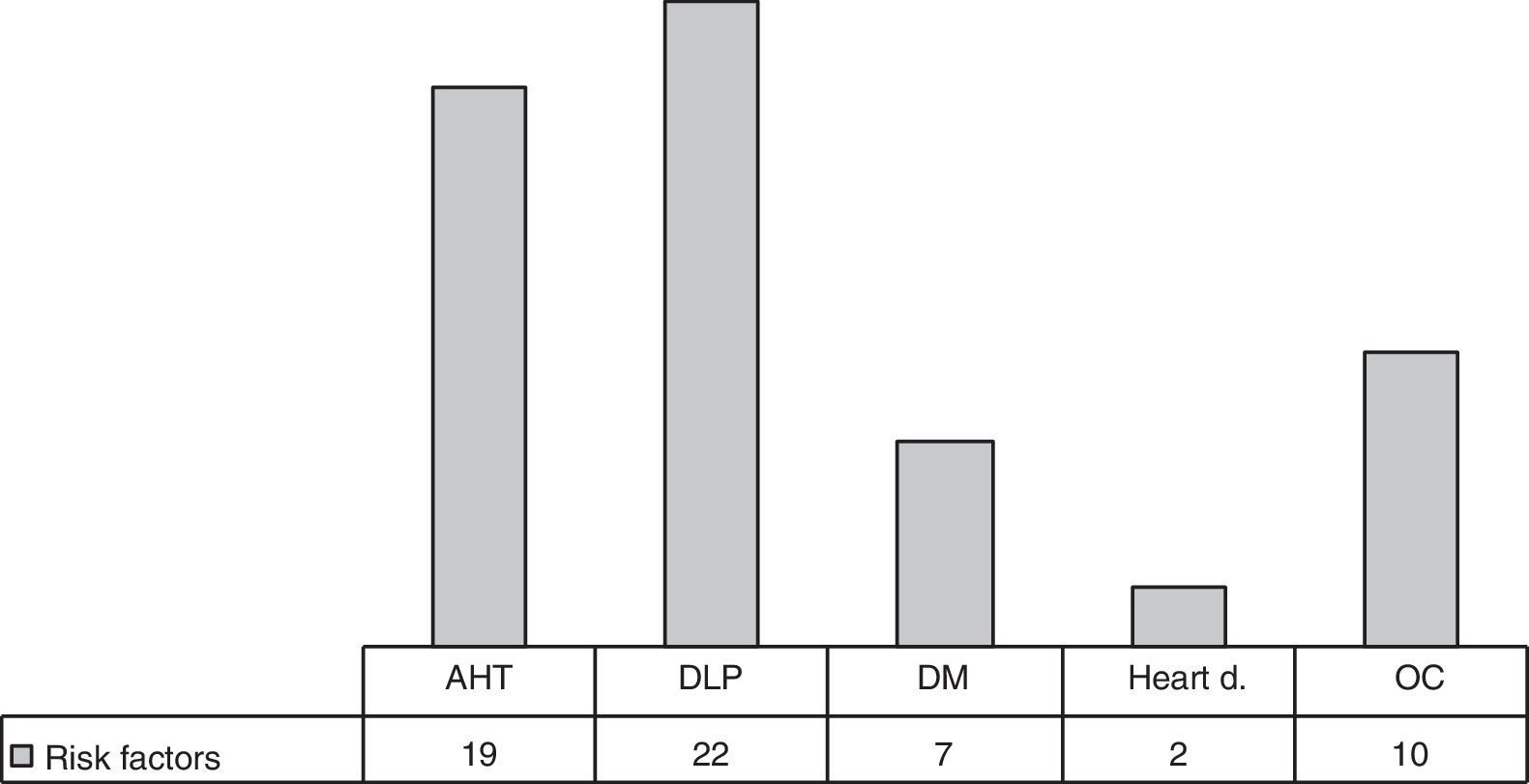
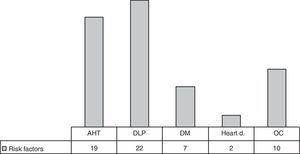
Among the 61 patients with IIH, 31 (50.81%) presented at least one cardiovascular risk factor, 22 (36.07%) had dyslipidaemia, 19 (31.15%) arterial hypertension, and 7 (11.5%) had diabetes mellitus. Hormonal contraception was recorded for 10 of the 42 women (23.81%) (Fig. 2).
CSF opening pressure was measured with patients in the lateral decubitus position, and the mean pressure value (meanP) was 33.05 cmH2O. No significant variations between sexes or significant differences between BMI groups were found.
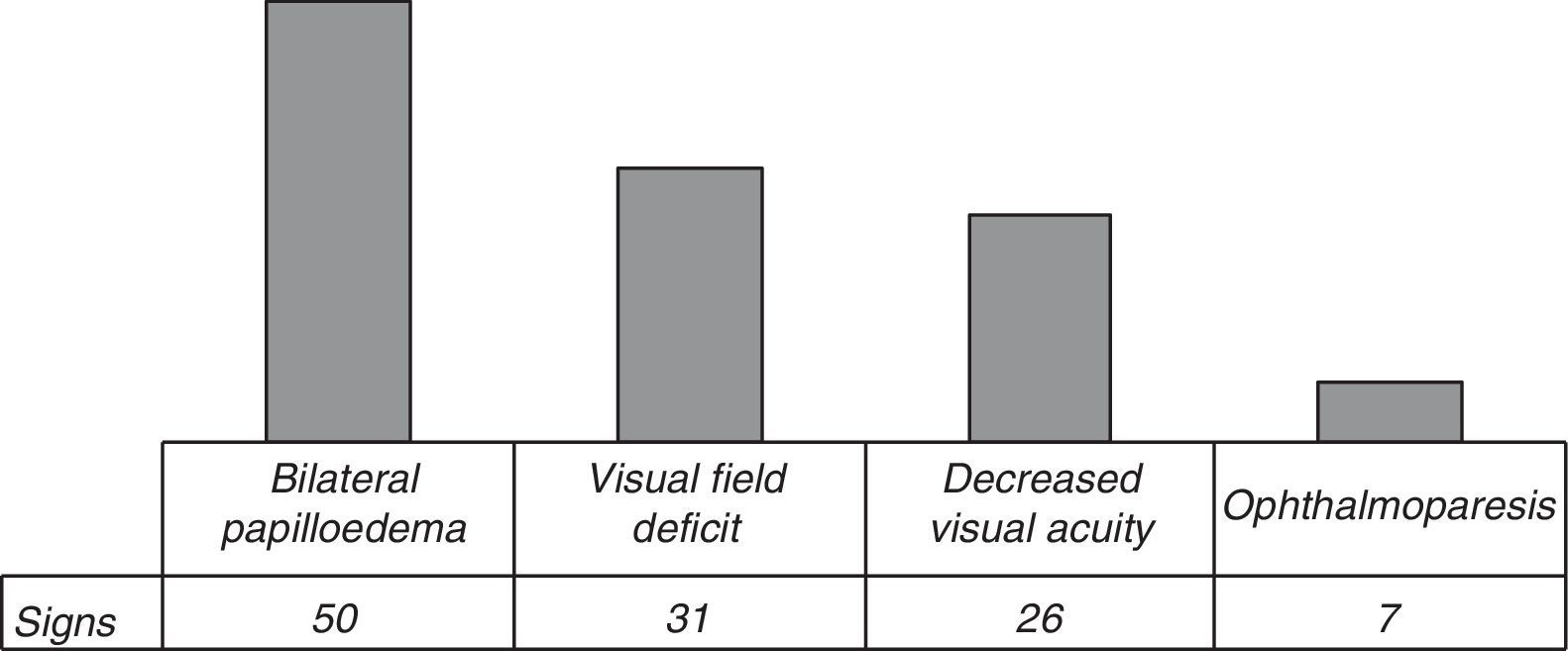
Clinical presentationFifty-two (85.25%) of the 61 patients with IIH presented headache. Abnormal visual field test results, visual disturbances –phosphenes– or decreased visual acuity were observed in 33 (59.01%) subjects. Ophthalmoparesis of the sixth cranial nerve was identified in 7 (11.5%) patients. On their ophthalmological examinations, 81.96% of the patients presented bilateral papilloedema (Fig. 3).
Cranial computed tomography was performed for all patients, and no lesions justifying IIH were observed. Magnetic resonance was performed for 59 (96.72%) patients. Furthermore, magnetic resonance angiography was performed for 11 of the 61 patients (18.03%) with signs of IIH.
Progression and treatmentDuring admission, 55 patients (90.16%) received treatment with acetazolamide dosed at 750 to 1500mg/day; corticosteroids (40-60mg/day for 2 weeks) were added in 5 cases (3.11%).
Among the 61 patients admitted with signs of IIH, 5 (8.2%) needed more aggressive treatments. Ventriculoperitoneal shunting was performed in 5 cases (4.91%), all of them being men. In the other 2 cases (3.27%), fenestration of the optic nerve was performed since the main problem was visual disturbance and there was no incapacitating headache. These 2 cases corresponded to women in the BMI > 40 group.
DiscussionIIH is present worldwide with an approximate incidence of 1 to 3/100 000 person/years. It is more frequent in obese women of childbearing potential, with women outnumbering men by a ratio of up to 9:1.4,11 In our study, approximate incidence is 1.2/100 000 person/years, which is a value similar to those described. The female/male ratio in our series was 2.2:1.6,11,12 However, these data should be interpreted with caution, since ours is a prospective study of hospitalised patients and IIH diagnosis could have been underestimated.
BMI analysis reveals a lower rate of obesity among men, showing a male/female ratio of 1:7 in the BMI > 40 group. Only a few earlier studies grouped patients according to their weight, and this makes it difficult to compare them with our series. However, Kesler highlighted these differences in BMI among men.13 Nonetheless, considering the small size of our sample, prospective studies are needed to identify BMI variations between the sexes and identify the relationship between BMI and CSF opening pressure.
Use of hormonal contraception was considered an important risk factor in 10 (23.8%) of the 42 women in our study. The percentage in our study was higher than that of other descriptive studies.4,8,14 Tobacco use was also an important risk factor for more than half of the patients.4,8,13,14
Headache, the most frequent symptom of IIH, was present in 75%-95% of the cases.4–8,12,15 In our series, headache symptoms presented in a percentage similar to the one previously reported (82.25%). This was also true of all other symptoms.
Suspicion of IIH is generally determined by the presence of papilloedema, but we have to keep in mind that there are cases of IIH patients with no papilloedema in the literature.9,10,15,16 In our series, all patients presented papilloedema, since they were strictly selected according to the modified Dandy criteria. Papilloedema associated with IIH is usually bilateral and asymmetrical, or else unilateral.4,8,14,22 Eleven of our 61 patients (18.03%) presented unilateral papilloedema. However, this percentage might be a low estimate since this is a prospective study in which subtle signs of incipient papilloedema may have been missed.
Diminished visual acuity was associated with papilloedema in more than half of the patients. According to several authors, impaired visual function is a severity marker that determines the indication for surgical treatment.4,8,18–20
CSF opening pressure (meanP: 33.05 cmH2O) is similar to that described in other series, with a normal biochemical composition for CSF and no significant differences in pressure between men and women (31.21 and 34.33 cmH2O, respectively).4,8 We found no differences in CSF opening pressure between patients grouped by BMI. Establishing the normal values for CSF pressure is therefore difficult. The current upper threshold is 25 cmH2O; however, values below that threshold in patients with low BMIs who meet the rest of the diagnostic criteria may also indicate IIH.
The most common and rapidly effective treatment option is acetazolamide. In our series, acetazolamide was administered to 55 out of 61 patients (90.61%), resulting in clinically favourable outcomes in more than 90% of the cases. This rate is similar to that obtained in previous studies.8,17–22
In patients in which medical treatment had failed, or those presenting significantly impaired visual function, surgical treatment was indicated (5/61). The selected surgical technique was fenestration of the optic nerve in 2 out of 19 men whose main symptom was visual disturbances with no incapacitating headache; lumboperitoneal shunting was performed in 3 out of 42 women. Although transverse sinus stenting is currently available as a treatment alternative, we did not use this technique with any of our patients, as this new procedure is not yet provided by our hospital. The small size of our sample does not allow us to identify the presence of a risk factor or predisposition by sex that could affect disease prognosis. Likewise, the sample is not reliable for assessing prognosis or the need for invasive treatment, since it consists of hospitalised patients and excludes any patients treated on an outpatient basis.
Men in our study presented an atypical profile with lower prevalence of headache and higher prevalence of visual impairment, which is in line with the results obtained by Kesler et al.13
We acknowledge the limitations of our study, which was conducted using retrospective data that has been retrospectively gathered. We should highlight that computed tomography yielded normal results in all patients and that results from the magnetic resonance scans were also normal in 98% of the cases. All selected patients met diagnostic criteria for IIH and responded to treatment. No other possible causes of the symptoms were identified.
We can conclude that IIH incidence is higher among young women with higher body weight and associated with the use of hormonal contraceptives. The main symptoms of IIH are headache with bilateral papilloedema and visual disturbances. One interesting finding from our study is the lower BMI observed among men, as well as less prevalence of headache and greater prevalence of visual disturbances. In conclusion, we believe that a detailed medical history that records atypical symptoms in men, such as visual disturbances, nausea/vomiting, diplopia, or tinnitus, is essential to help us orientate diagnosis.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Contreras-Martin Y, Bueno-Perdomo J.H. Hipertensión intracraneal idiopática: análisis descriptivo en nuestro medio. Neurología. 2015;30:106–10.