Autoimmune polyglandular syndrome is a rare disease with a low incidence worldwide. We present the case of an adult male with a history of parietal antibody-positive gastritis, central retinal vein obstruction and transverse myelitis. The patient was admitted for exacerbation of myelitis symptoms. The thyroid profile was positive for antibodies, indicating the presence of euthyroid autoimmune thyroid disease. The patient was finally diagnosed with autoimmune polyglandular syndrome type 3B. In the absence of adequate response to methylprednisolone and immunoglobulin, we started treatment with cyclophosphamide and later maintenance therapy with azathioprine. At one year of follow-up, the patient presented paraparesis as sequel, did not present new relapses and control tests were negative for another associated disease.
El síndrome poliglandular autoinmune es una enfermedad rara con baja incidencia a nivel mundial. Presentamos el caso de un varón adulto con antecedentes de gastritis parietal con anticuerpos positivos, obstrucción de la vena central de la retina y mielitis transversa. El paciente ingresó por exacerbación de los síntomas de mielitis. El perfil tiroideo fue positivo para anticuerpos, lo que indica la presencia de enfermedad tiroidea autoinmune eutiroidea. El paciente fue finalmente diagnosticado de síndrome poliglandular autoinmune tipo 3B. Ante la falta de respuesta adecuada a metilprednisolona e inmunoglobulina, se inició tratamiento con ciclofosfamida y posteriormente terapia de mantenimiento con azatioprina. Al año de seguimiento, el paciente quedó con paraparesia secuelar, no presentó nuevas recaídas y las pruebas de control fueron negativas para otra enfermedad asociada.
Autoimmune polyglandular syndrome (APS) is a disease with a low prevalence worldwide and is defined as the coexistence of at least two autoimmune endocrinopathies.1 Neufeld and Blizzard classified this entity into four types. Type 1 APS is the least frequent with an estimated prevalence of 1 per 100,000 inhabitants, while the other types together have a prevalence of approximately 1 per 20,000.2,3 Type 3 APS manifests together with autoimmune thyroid disease and two other associated conditions, with neurological manifestations being the least frequent.3 We present the case of a Peruvian patient with autoimmune polyglandular autoimmune syndrome type 3 with associated transverse myelitis. This manuscript was prepared following the CARE guidelines for case reports4 and the patient's consent was obtained for publication of the article.
Case reportWe describe the case of a 59-year-old male from Lima, Peru. The patient had no significant family history but did have a personal history of parietal antibody-positive chronic gastritis, central retinal vein obstruction of the left eye with sequelae amaurosis and transverse myelitis of idiopathic etiology diagnosed in October 2018. After ruling out systemic autoimmune, infectious, neoplastic and demyelinating causes including anti-acuaporin-4 and anti-MOG dosing, the physicians concluded that the disease was idiopathic. The patient presented partial response to plasma exchange (7 sessions) and was discharged with mild paraparesis and subsequent neurogenic bladder.
In April 2020, 18 months after the first myelitis event, the patient presented symptom flare-up. After 2 days of illness, the patient was admitted to a private clinic. Clinical examination showed paraplegia and bilateral Babinski. Then, he was treated with 1g of methylprednisolone intravenously for 5 days. In the absence of clinical improvement, he was referred to a more complex hospital one week later.
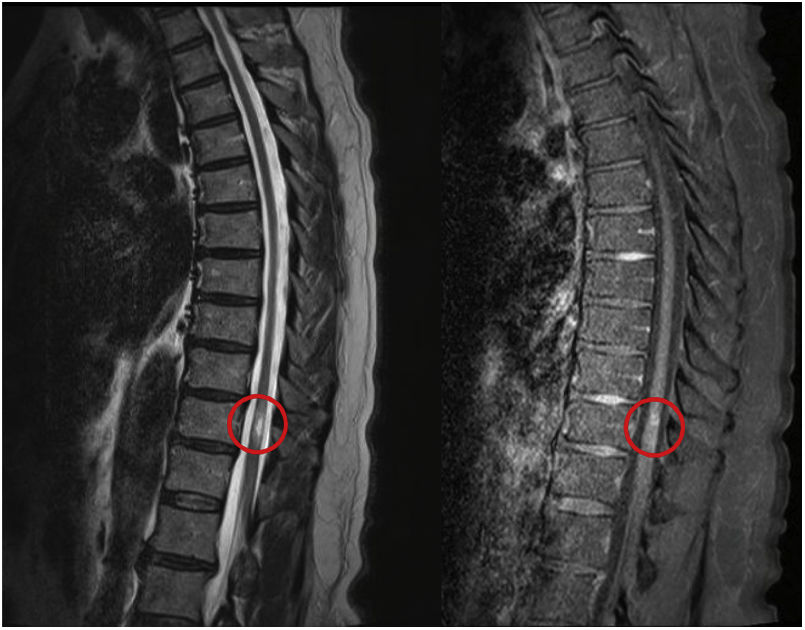
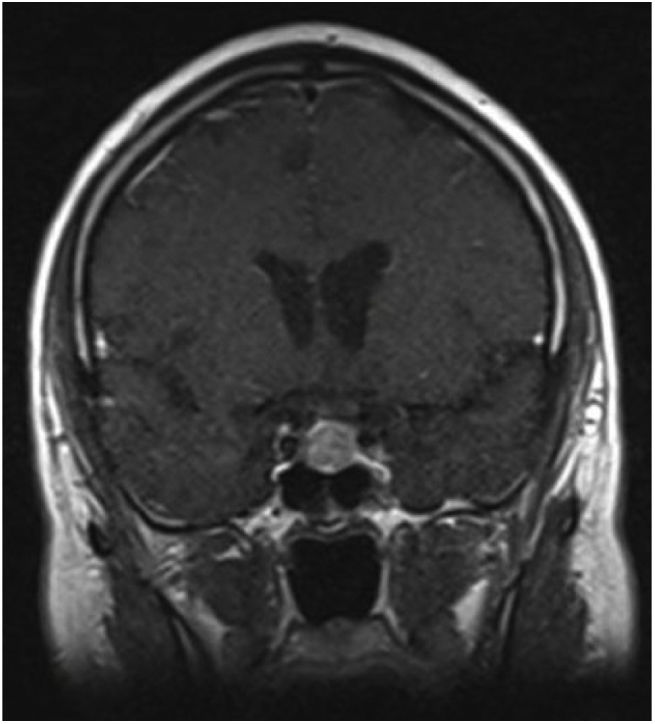
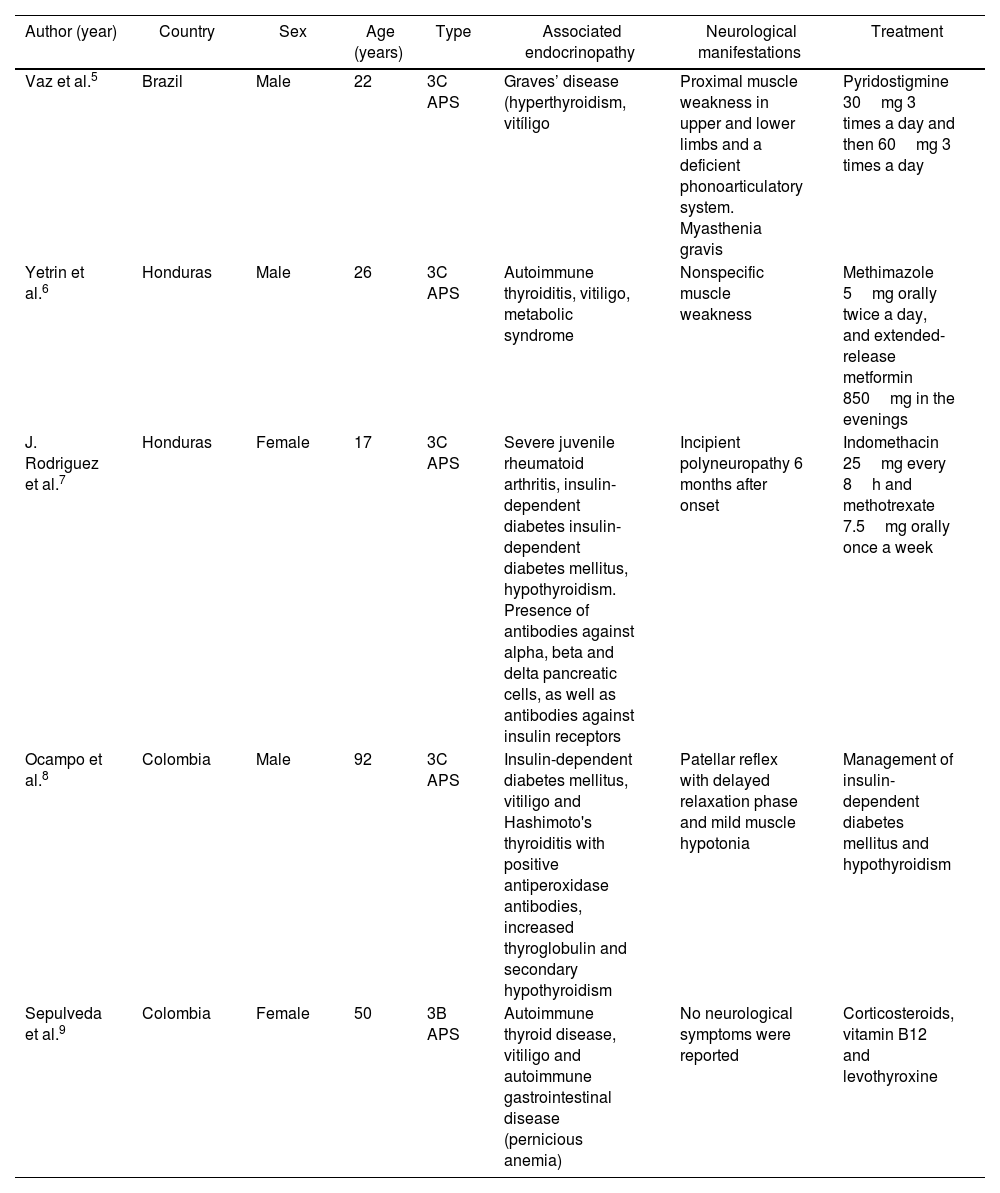
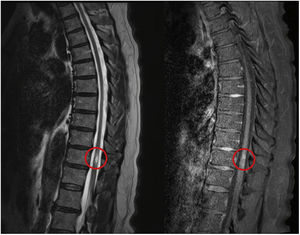
Magnetic resonance imaging of the brain and spine showed a focal hypersignal of 2.2cm with central location involving the distal dorsal medulla at the level of D11, with marginal preservation of the medullary signal, and mild-moderate contrast enhancement (Fig. 1). Due to the central morphological involvement and contrast uptake, a diagnosis of progressive transverse myelitis was suggested, and a low contrast-enhancing pituitary lesion of 14mm was found with preservation of the usual signal of the optic chiasm (Fig. 2). Whole body tomography found no solid neoplasms.
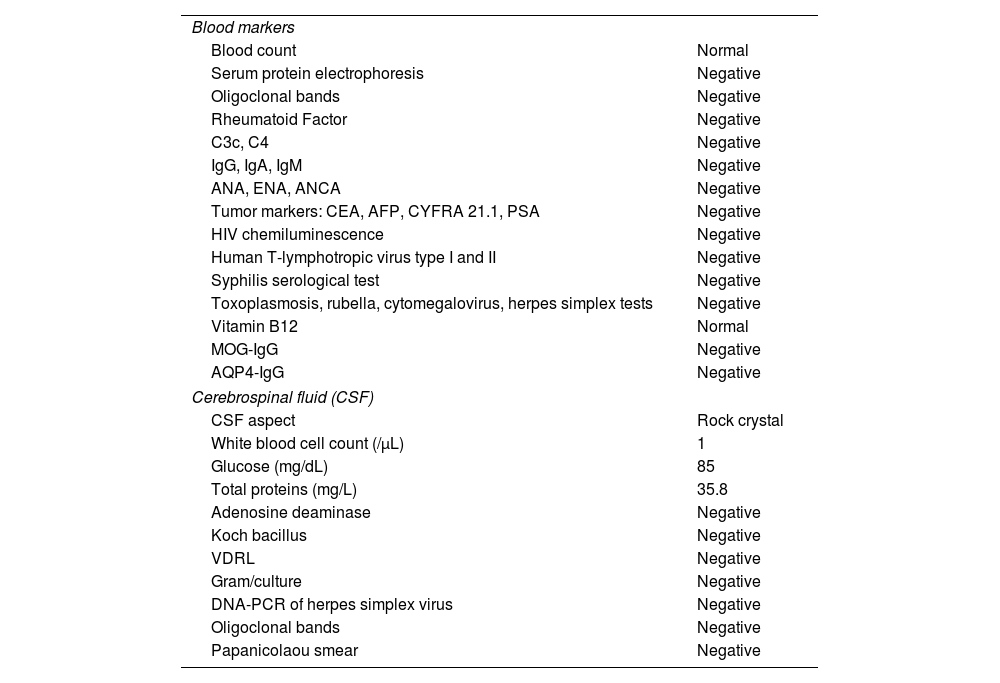
Laboratory and cerebrospinal fluid tests were negative for infectious, demyelinating, collagenopathy and neoplastic disease (Table 1). The thyroid profile was unaltered, but the antibodies were positive (anti-thyroglobulin antibodies: 64IU/mL and anti-thyroperoxidase: 62IU/mL), leading to a diagnosis of euthyroid autoimmune thyroid disease. Lupus anticoagulant was positive but anticardiolipin and B2-glycoprotein were negative. Taking into account the pituitary lesion, we performed adrenal axis tests, which were negative; however, it should be noted that these tests were performed after receiving corticosteroid treatment (prolactin: 14ng/mL; adrenocorticotropic hormone: 8.55pg/mL; luteinizing hormone: 2. 87mlU/mL; follicle stimulating hormone: 6.59mlU/mL; cortisol at 8am: 2.48μg/dL; insulin-like growth factor type I – somatomedin C: 143ng/mL; free triiodothyronine: 2.57pg/mL; free thyroxine: 1.1ng/dL; thyroid stimulating hormone: 3.42mIU/mL).
Laboratory markers findings in the patient.
| Blood markers | |
| Blood count | Normal |
| Serum protein electrophoresis | Negative |
| Oligoclonal bands | Negative |
| Rheumatoid Factor | Negative |
| C3c, C4 | Negative |
| IgG, IgA, IgM | Negative |
| ANA, ENA, ANCA | Negative |
| Tumor markers: CEA, AFP, CYFRA 21.1, PSA | Negative |
| HIV chemiluminescence | Negative |
| Human T-lymphotropic virus type I and II | Negative |
| Syphilis serological test | Negative |
| Toxoplasmosis, rubella, cytomegalovirus, herpes simplex tests | Negative |
| Vitamin B12 | Normal |
| MOG-IgG | Negative |
| AQP4-IgG | Negative |
| Cerebrospinal fluid (CSF) | |
| CSF aspect | Rock crystal |
| White blood cell count (/μL) | 1 |
| Glucose (mg/dL) | 85 |
| Total proteins (mg/L) | 35.8 |
| Adenosine deaminase | Negative |
| Koch bacillus | Negative |
| VDRL | Negative |
| Gram/culture | Negative |
| DNA-PCR of herpes simplex virus | Negative |
| Oligoclonal bands | Negative |
| Papanicolaou smear | Negative |
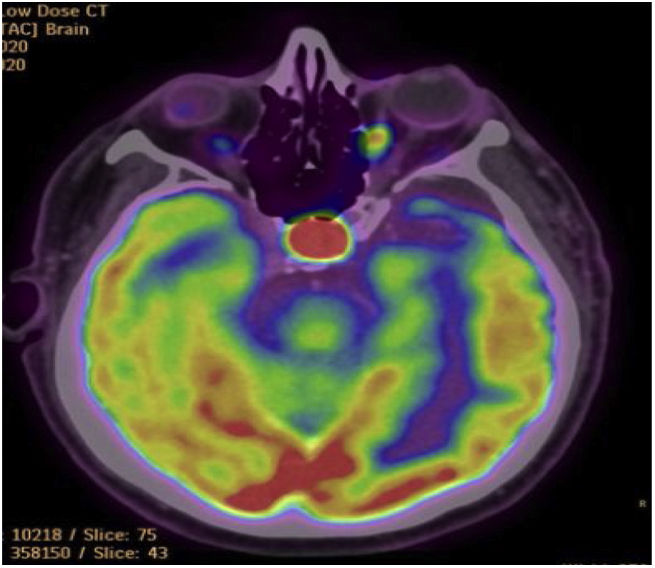
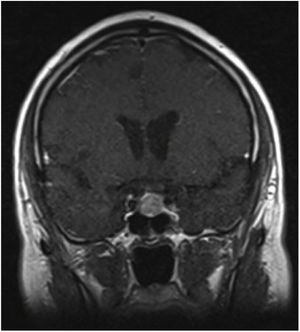
We performed a whole body 18F-FDG PET/CT study to identify any occult neoplasm, finding that the metabolism was normal and symmetrical in both cerebral hemispheres. In addition, the scan showed a hypermetabolic pituitary hypermetabolic lesion slightly lateralized to the left with discrete enhancement of the contrast of 14mm with a SUVmax of 28.4 suggestive of sellar tumor with increased hypermetabolism (Fig. 3). The rest of the study showed no hypermetabolic lesions suggestive of active tumoral disease.
We indicated treatment with intravenous immunoglobulin at a dose of 0.4g/kg/day for 5 days, without satisfactory response after three weeks. The patient presented asymptomatic bacteriuria due to Enterococcus faecalis and Escherichia coli and was administered ampicillin and nitrofurantoin before receiving any immunosuppressive treatment.
Considering the findings described above, the patient was diagnosed with autoimmune polyglandular syndrome type 3B, with manifestation of chronic gastritis due to anti-parietal cell antibodies, euthyroid autoimmune thyroid disease and transverse myelopathy. Treatment was initiated with 750mg/m2 of cyclophosphamide intravenously monthly for 6 months. At medical discharge, physical therapy, and oral treatment with 5mg of oxybutynin every 12h, 0.4mg per day of tamsulosin, 300mg of gabapentin every 8h and 0.5mg per day of clonazepam were indicated.
Considering the autoimmune endocrinopathy and the pituitary lesion, the tests were repeated at 3 months in the absence of corticosteroid treatment, and the antiphospholipid syndrome profile was also repeated due to the finding of lupus anticoagulant. In the ambulatory control at one year of follow-up, the patient did not present clinical relapse. He presented sequelae paraparesis and the control APS profile and the pituitary axis tests were negative for any other associated disease. After completing treatment with cyclophosphamide, azathioprine was continued as maintenance immunosuppressive treatment.
DiscussionAPS is a rare entity and estimates of its frequency have been made from case reports and small cohorts of patients. The diagnosis is clinical and can be complemented with serological and functional screening tests such as the detection of autoantibodies.3
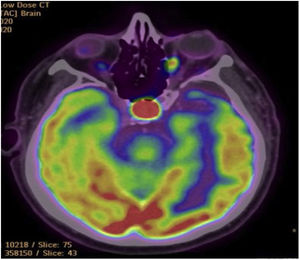
In the last 5 years, about 50 cases of APS have been reported in Latin America, of which only 5 were case reports of type 3 APS.5–9 Regarding subtypes, type 3C APS has been reported in Brazil,5 Honduras6,7 and Colombia,8 while subtype 3B is considered one of the least studied10 and has been reported only in Colombia.9 To our knowledge, no cases of this subtype have been reported in Peru.
Each type of APS has specific clinical characteristics. Type 3 is polygenetic, and presents during adulthood, with autoimmune thyroid disease and other associated autoimmune conditions, endocrinological or otherwise.11 In the case of our patient, APS was classified as type 3 due to the association of autoimmune thyroid disease and was subclassified as type B by the presence of pernicious anemia due to anti-parietal cell antibodies.
In relation to the spectrum of neurological entities associated with APS type 3, previous cases in the literature include polyneuropathy, neurocognitive disorder, optic neuropathy, demyelinating disease and movement disorders of central cause.5,11 Thus, the present case is the first report of recurrent transverse myelitis associated with polyglandular syndrome type 3B in Latin America (Table 2). Moreover, since the study of the hormonal axis did not indicate any type of associated pituitary endocrinopathy, we suggest that the sellar lesion was likely an incidental finding of a non-functional hypophysis.
Reported cases of autoimmune polyglandular syndrome type 3 in Latin America.
| Author (year) | Country | Sex | Age (years) | Type | Associated endocrinopathy | Neurological manifestations | Treatment |
|---|---|---|---|---|---|---|---|
| Vaz et al.5 | Brazil | Male | 22 | 3C APS | Graves’ disease (hyperthyroidism, vitíligo | Proximal muscle weakness in upper and lower limbs and a deficient phonoarticulatory system. Myasthenia gravis | Pyridostigmine 30mg 3 times a day and then 60mg 3 times a day |
| Yetrin et al.6 | Honduras | Male | 26 | 3C APS | Autoimmune thyroiditis, vitiligo, metabolic syndrome | Nonspecific muscle weakness | Methimazole 5mg orally twice a day, and extended-release metformin 850mg in the evenings |
| J. Rodriguez et al.7 | Honduras | Female | 17 | 3C APS | Severe juvenile rheumatoid arthritis, insulin-dependent diabetes insulin-dependent diabetes mellitus, hypothyroidism. Presence of antibodies against alpha, beta and delta pancreatic cells, as well as antibodies against insulin receptors | Incipient polyneuropathy 6 months after onset | Indomethacin 25mg every 8h and methotrexate 7.5mg orally once a week |
| Ocampo et al.8 | Colombia | Male | 92 | 3C APS | Insulin-dependent diabetes mellitus, vitiligo and Hashimoto's thyroiditis with positive antiperoxidase antibodies, increased thyroglobulin and secondary hypothyroidism | Patellar reflex with delayed relaxation phase and mild muscle hypotonia | Management of insulin-dependent diabetes mellitus and hypothyroidism |
| Sepulveda et al.9 | Colombia | Female | 50 | 3B APS | Autoimmune thyroid disease, vitiligo and autoimmune gastrointestinal disease (pernicious anemia) | No neurological symptoms were reported | Corticosteroids, vitamin B12 and levothyroxine |
APS: autoimmune polyglandular syndrome.
Timely diagnosis and management of APS is essential to avoid greater morbidity and mortality in people with this disease. Likewise, it is worth mentioning that the treatment lies in managing the different glandular insufficiencies independently.12 Cellular immunity plays a fundamental role, due to the loss of self-tolerance in autoimmune disease; therefore, immunosuppressive maintenance therapies produce beneficial results in these patients.13 Since our patient did not present adequate response to first line therapy with methylprednisolone or immunoglobulin, we opted for management with cyclophosphamide and later azathioprine.
In conclusion, to our knowledge the present report is the first case of atypical neurological manifestation of severe recurrent transverse myelitis associated with polyglandular syndrome type 3B in Latin America. Timely diagnosis and maintenance immunosuppressive management are important for avoiding clinical relapses and achieving a better prognosis.
Authors’ contributionsMAV, MMP, RJOR, LCBC, JCAM, DUP and MVE treated the patient, interpreted the neuroradiologic imaging and laboratory markers. All authors participated in the design, writing and critical review and approved the final version of the manuscript.
Ethical approval and informed consentAll authors consent to the publication of this manuscript.
Data availability statementThe original contributions described in the case report are included in the article. Further inquiries can be directed to the corresponding author.
FundingThe study was self-funded.
Conflict of interestNone.
We thank the Universidad Científica del Sur for the English editing support.