Despite the impact of cerebrovascular disease (CVD) on global health, its morbidity and time trends in Spain are not precisely known.
ObjectiveThe purpose of our study was to characterise the epidemiology and trends pertaining to stroke in Aragon over the period 1998-2010.
MethodsWe conducted a retrospective, descriptive study using the data of the Spanish health system's Minimum Data Set and included all stroke patients admitted to acute care hospitals in Aragon between 1 January 1998 and 31 December 2010. We present data globally and broken down by stroke subtype, sex, and age group.
ResultsThe number of cases increased by 13% whereas age- and sex-adjusted hospitalisation rates showed a significant decrease for all types of stroke (mean annual decrease of 1.6%). Men and women in younger age groups showed opposite trends in hospitalisation rates for ischaemic stroke. Case fatality rate at 28 days (17.9%) was higher in patients with intracerebral haemorrhage (35.8%) than in those with subarachnoid haemorrhage (26.2%) or ischaemic stroke (13%). CVD case fatality showed a mean annual decline of 2.8%, at the expense of the fatality rate of ischaemic stroke, and it was more pronounced in men than in women.
DiscussionUnderstanding stroke epidemiology and trends at the regional level will help establish an efficient monitoring system and design appropriate strategies for health planning.
A pesar de la relevancia sanitaria de la enfermedad cerebrovascular (ECV), su morbilidad en España y sus tendencias temporales no se conocen con precisión.
ObjetivoEl objetivo de nuestro estudio fue caracterizar la epidemiología del ictus en Aragón y su evolución en el periodo 1998-2010.
MétodosEstudio descriptivo retrospectivo a partir de una base de datos extraída del Conjunto Mínimo Básico de Datos, incluyendo todas las altas por ECV de los hospitales de Aragón en el periodo 1998-2010. Se presentan los datos de manera global y separada por tipo de ictus, sexo y franja etaria.
ResultadosEl número de casos aumentó un 13%, mientras que las tasas de hospitalización ajustadas por edad y sexo han mostrado un descenso significativo para el conjunto de los ictus (descenso medio anual del 1,6%). Hemos observado tendencias opuestas en las tasas de ictus isquémico entre varones y mujeres de los grupos de edad más jóvenes. La tasa de letalidad a los 28 días fue del 17,9%, y fue superior en los pacientes con hemorragia cerebral (35,8%) con respecto a los pacientes con hemorragia subaracnoidea (26,2%) e ictus isquémico (13%). La letalidad por ECV presentó un descenso medio anual del 2,8%, a expensas del descenso observado en el ictus isquémico, y fue más pronunciada en los hombres que en las mujeres.
DiscusiónEl conocimiento de la epidemiología del ictus a nivel regional y sus tendencias contribuirá a establecer un sistema eficiente de vigilancia y diseñar estrategias adecuadas de planificación sanitaria.
Cerebrovascular diseases (CVDs) are the second most frequent cause of death in Spain, after myocardial infarction.1 Some studies conducted in Spain estimate the incidence of CVDs at 120-350 cases per 100000 person-years.2,3 However, the incidence of CVDs and the associated mortality vary greatly between autonomous communities; this variability is mainly due to differences in the management of vascular risk factors, in socioeconomic status, and in healthcare.4 A north–south gradient has been described, with higher mortality rates in the southern half of Spain than in the rest of the country. Mortality due to CVD in Aragon is currently similar to the national mean.5 The region's population is particularly old, with 19.8% of inhabitants being older than 65 years (vs 16.6% in the Spanish population).6
CVDs constitute the first cause of disability in adults and account for 2% to 4% of national healthcare expenditure.7,8 The social and economic burden of CVDs is rapidly increasing due to population ageing: it is estimated that by 2025, 500000 people in Spain will have disability due to CVDs.9 Surprisingly, the morbidity and time trends of CVDs in Spain are not precisely known, despite their great impact on the healthcare system.
Much progress has been made on stroke prevention and treatment in recent years (especially in terms of thrombolysis, endovascular treatment, specialised neurological care, and stroke units); epidemiological surveillance tools are needed to evaluate the impact of the efforts and resources allocated to CVD prevention and treatment. At present, the only epidemiological data on CVD progression available in our setting is from mortality statistics and data drawn from the results of the Spanish hospital morbidity survey; although these data are relevant, they are insufficient for the epidemiological surveillance of CVDs. Data from international studies (as well as a limited number of studies conducted in Spanish populations) cannot be extrapolated to our setting as most incidence studies focus on small urban areas and are therefore not representative of the general population.
ObjectiveWe aimed to study the time trends of hospitalisation and in-hospital case fatality due to acute CVD in Aragon in 1998-2010, using the minimum basic dataset (MBDS).
Patients and methodsWe conducted a retrospective, descriptive study using hospital-based administrative data (MBDS).
Sample and inclusion/exclusion criteriaWe accessed a database of discharges of patients with CVD from the MBDS of all hospitals in the autonomous community of Aragon; the database included data from the period 1998-2010, from all patients whose main diagnosis at discharge was CVD (codes 430 to 438.9 of the International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM]).
Inclusion criteria- ∘
Discharges from public health centres from the health service of Aragon
- ∘
Main diagnosis:
- •
430: subarachnoid haemorrhage
- •
431: intracerebral haemorrhage
- •
433.x1: occlusion and stenosis of precerebral arteries, with cerebral infarction
- •
434.x1: occlusion of cerebral arteries, with cerebral infarction
- •
436: acute, but ill-defined, cerebrovascular disease
- •
- ∘
Date of admission:
- •
01/01/1998-31/12/2010
- •
- ∘
Discharges from recovery and rehabilitation centres
- ∘
Discharges from private health centres and ordered by insurance companies
- ∘
Main diagnosis:
- •
432: other and unspecified intracranial haemorrhage
- •
433.x0: occlusion and stenosis of precerebral arteries, without mention of cerebral infarction
- •
434.x0: occlusion of cerebral arteries without mention of cerebral infarction
- •
435: transient cerebral ischaemia
- •
437: other and ill-defined cerebrovascular disease
- •
438: late effects of cerebrovascular disease
- •
- ∘
Patients transferred between general hospitals: we identified duplicate cases by detecting coincidences in birth date, sex, type of stroke, and dates of discharge from the referring hospital and admission at the receiving hospital.
- ∘
Recurrence within 28 days
- ∘
Sex
- ∘
Age at admission
- ∘
Date of admission
- ∘
Date of discharge
- ∘
Main diagnosis (ICD-9-CM code)
- ∘
Age range. The study population was classified into 9 age groups: 0-14, 15-24, 25-34, 35-44, 45-54, 55-64, 65-74, 75-84, and ≥85 years.
- ∘
To analyse trends by age group, we used the following distribution: <55, 55-64, 65-74, 75-84, and ≥85 years.
- ∘
Stroke type. Strokes were classified according to the ICD-9-CM:
- •
430: subarachnoid haemorrhage
- •
431: intracerebral haemorrhage
- •
433.x1, 434.x1, and 436: ischaemic stroke
- •
- ∘
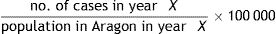
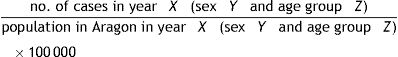
Formulas (global and specific for stroke type, sex, and age group):
- •
Hospitalisation rate:
- •
Age- and sex-specific hospitalisation rate:
- •
Early in-hospital case fatality rate (within 28 days of admission):
In this study, the term “case fatality” is always used to refer to in-hospital case fatality.
- •
Quantitative variables are expressed as means±SD and qualitative variables as percentages. We used the chi-square test to determine the association between 2 categorical variables and the t test for independent samples to determine the association between dichotomous and normally distributed quantitative variables. The association between polytomous and quantitative variables was determined using either one-way ANOVA (Snedecor's F) or the Kruskal–Wallis test, depending on whether the quantitative variable was normally distributed. We used an alpha level of .05. All tests were two-tailed.
Annual hospitalisation rates were calculated based on each year's population according either to the local census (1998-2004) or to the register of social security health card holders (2005-2010); these data were provided by the Department of Health of the Government of Aragon. We analysed hospitalisation trends by adjusting the hospitalisation rates to a reference population (population of Aragon in 2004).
For the time trend analysis, we studied the effect of time (year) on the hospitalisation rate (hospitalised patients/population), adjusted for age. To this end, we calculated the incidence rate ratio (IRR), adjusted for age, and the significance (P) and 95% confidence interval (95% CI) for each stroke type, each sex, and for both sexes. The IRR is the mean annual change in the incidence rate, expressed as a decimal. It is interpreted as a relative risk. The IRR is calculated using negative binomial regression, a model applicable to Poisson variables with extra-Poisson variation. The same methodology was used to study case fatality rate trends, by means of the case fatality rate ratio (CFRR).
We used SPSS® v.17 and Stata® v.11.1 for statistical analysis.
EthicsThe confidentiality of personal data was guaranteed in compliance with the Spanish Organic Law for the Protection of Personal Data. This study was approved by the Healthcare Ethics Committee of the regional government of Aragon.
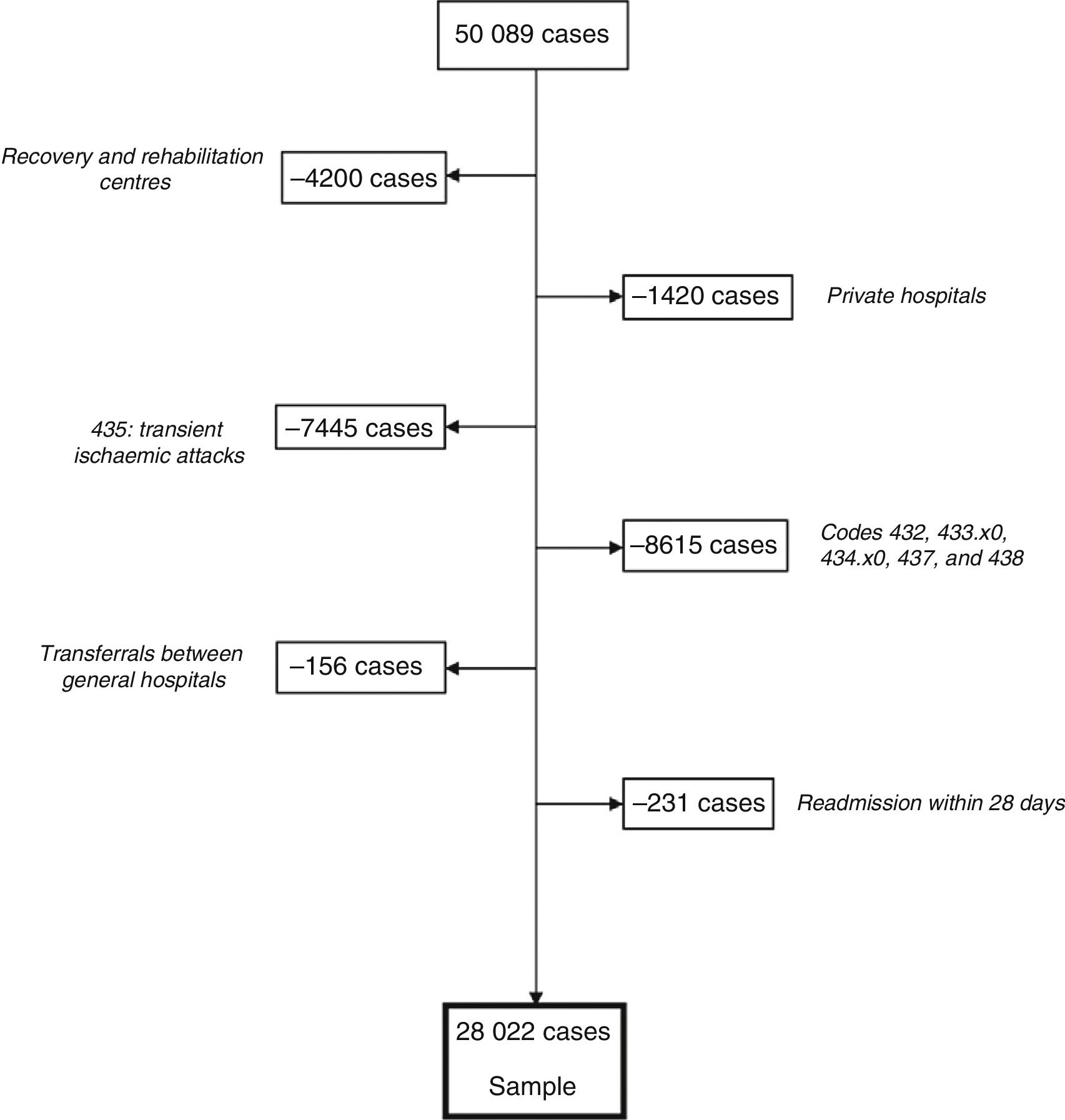
ResultsGeneral dataFig. 1 describes the process of patient inclusion and exclusion. The database included 50089 cases of CVD, 28022 of which met the inclusion criteria; 54.6% were men and 45.4% were women.
The mean age of our sample was 74±12.5 years: 72±12.4 years in men and 76.4±12.2 years in women. Around 81% of the cases occurred in patients older than 65.
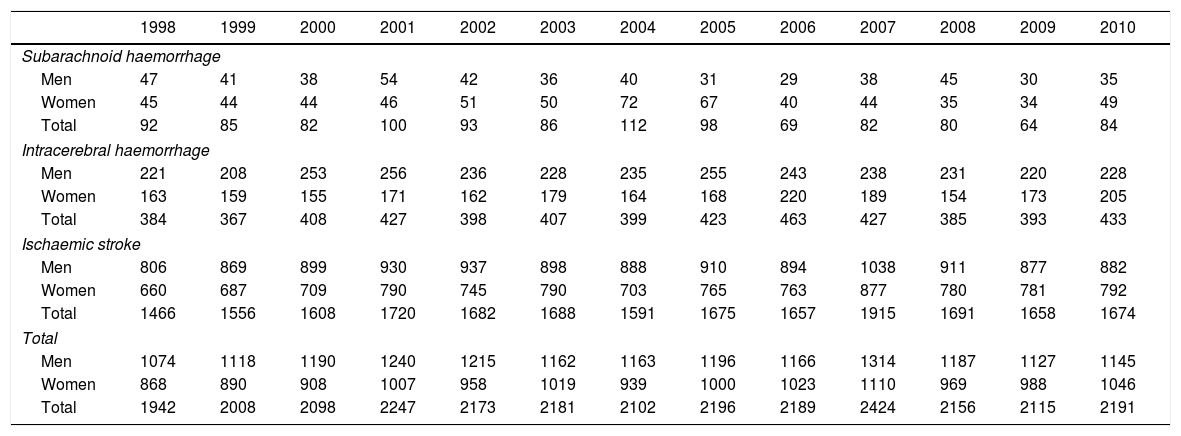
Seventy-seven per cent of the cases were ischaemic strokes, 19% were intracerebral haemorrhages, and the remaining 4% were subarachnoid haemorrhages. The absolute number of cases increased by 13% over the study period (6.6% in men and 20.5% in women). Table 1 shows the annual number of cases between 1998 and 2010, broken down by sex and stroke type.
Number of admissions due to acute cerebrovascular disease during the period 1998-2010, broken down by stroke type, age, and sex.
| 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Subarachnoid haemorrhage | |||||||||||||
| Men | 47 | 41 | 38 | 54 | 42 | 36 | 40 | 31 | 29 | 38 | 45 | 30 | 35 |
| Women | 45 | 44 | 44 | 46 | 51 | 50 | 72 | 67 | 40 | 44 | 35 | 34 | 49 |
| Total | 92 | 85 | 82 | 100 | 93 | 86 | 112 | 98 | 69 | 82 | 80 | 64 | 84 |
| Intracerebral haemorrhage | |||||||||||||
| Men | 221 | 208 | 253 | 256 | 236 | 228 | 235 | 255 | 243 | 238 | 231 | 220 | 228 |
| Women | 163 | 159 | 155 | 171 | 162 | 179 | 164 | 168 | 220 | 189 | 154 | 173 | 205 |
| Total | 384 | 367 | 408 | 427 | 398 | 407 | 399 | 423 | 463 | 427 | 385 | 393 | 433 |
| Ischaemic stroke | |||||||||||||
| Men | 806 | 869 | 899 | 930 | 937 | 898 | 888 | 910 | 894 | 1038 | 911 | 877 | 882 |
| Women | 660 | 687 | 709 | 790 | 745 | 790 | 703 | 765 | 763 | 877 | 780 | 781 | 792 |
| Total | 1466 | 1556 | 1608 | 1720 | 1682 | 1688 | 1591 | 1675 | 1657 | 1915 | 1691 | 1658 | 1674 |
| Total | |||||||||||||
| Men | 1074 | 1118 | 1190 | 1240 | 1215 | 1162 | 1163 | 1196 | 1166 | 1314 | 1187 | 1127 | 1145 |
| Women | 868 | 890 | 908 | 1007 | 958 | 1019 | 939 | 1000 | 1023 | 1110 | 969 | 988 | 1046 |
| Total | 1942 | 2008 | 2098 | 2247 | 2173 | 2181 | 2102 | 2196 | 2189 | 2424 | 2156 | 2115 | 2191 |
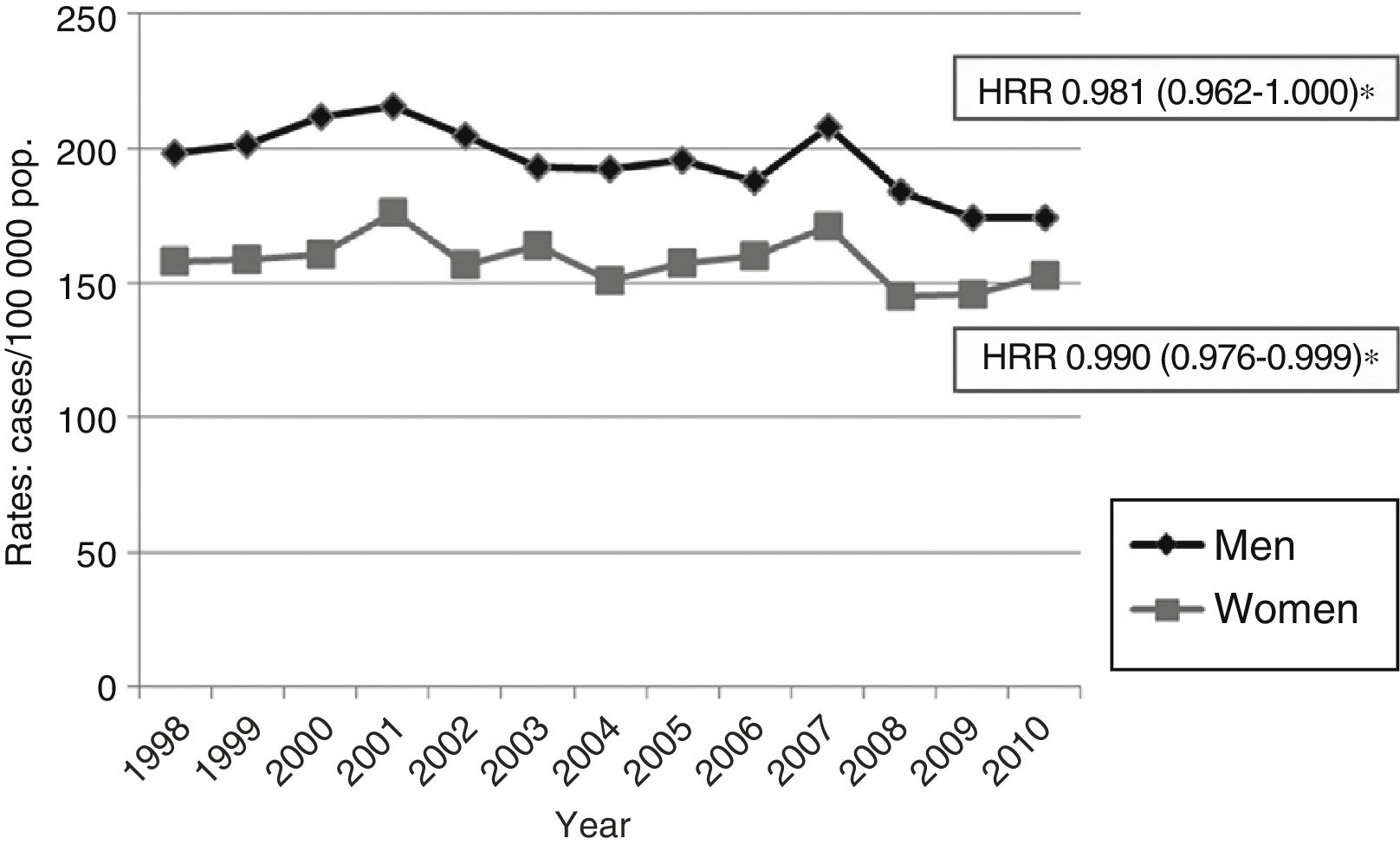
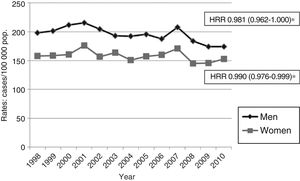
Age- and sex-adjusted hospitalisation rates for stroke decreased significantly over the study period (IRR=0.984, which results in a mean annual decrease of 1.6%) (Fig. 2). Hospitalisation rates decreased in all groups of male patients younger than 85 years; no significant changes in hospitalisation rates were observed in women, however.
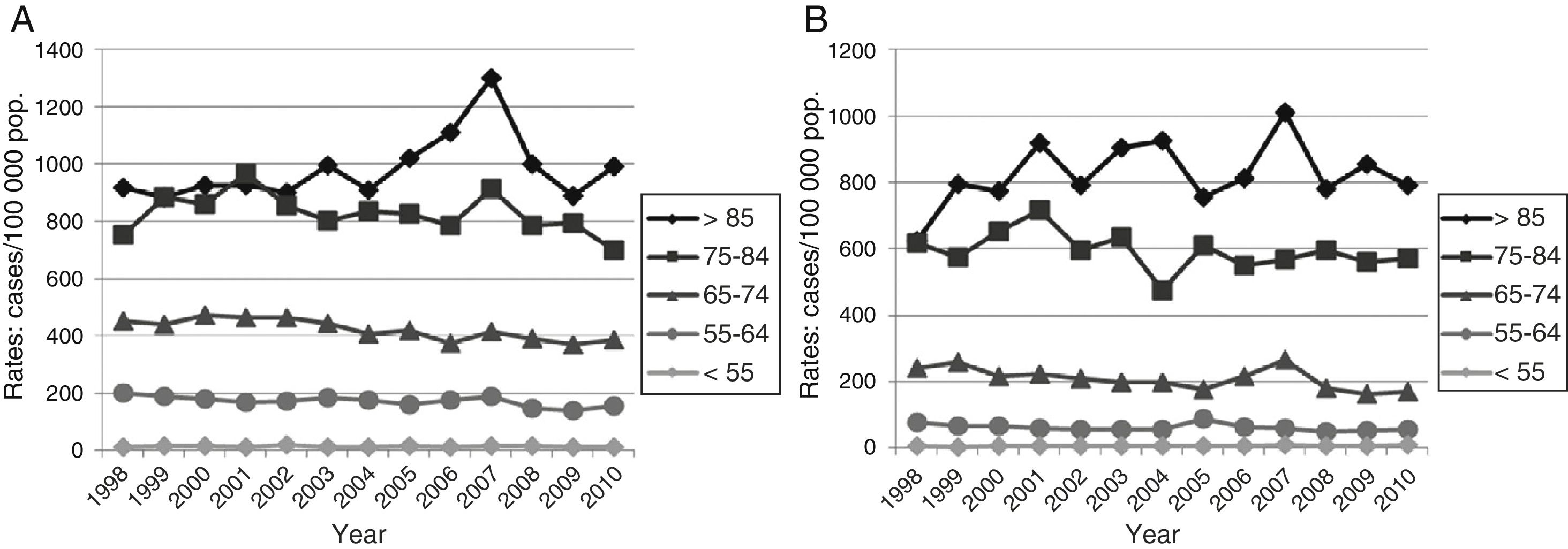
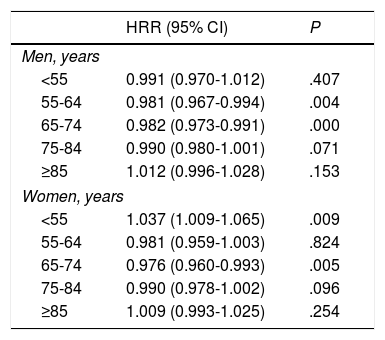
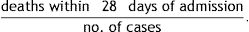
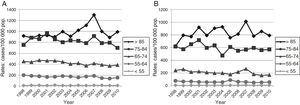
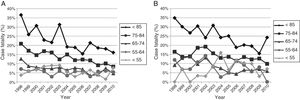
Hospitalisation rates associated with subarachnoid and intracerebral haemorrhages did not change significantly over the study period. The analysis of hospitalisation rates for ischaemic stroke by age group revealed the following (Fig. 3 and Table 2): (1) for women younger than 55 years, we observed an increase in hospitalisation rates, unlike men of the same age group, for whom no significant changes were observed over the study period; (2) for ages 55-64, we observed a mean annual decrease of 1.9% in men, and no significant differences in women; (3) for ages 65-74, hospitalisation rates decreased in both sexes, with a mean annual decrease of 2% in men and 2.4% in women; (4) for ages 75-84, similar variations were observed in both sex groups, with a mean annual decrease of 1%; this was not significant; and (5) no significant variations were observed in patients aged 85 years and older.
Hospitalisation rate ratio for ischaemic stroke in men and women for the period 1998-2010, broken down by age group.
| HRR (95% CI) | P | |
|---|---|---|
| Men, years | ||
| <55 | 0.991 (0.970-1.012) | .407 |
| 55-64 | 0.981 (0.967-0.994) | .004 |
| 65-74 | 0.982 (0.973-0.991) | .000 |
| 75-84 | 0.990 (0.980-1.001) | .071 |
| ≥85 | 1.012 (0.996-1.028) | .153 |
| Women, years | ||
| <55 | 1.037 (1.009-1.065) | .009 |
| 55-64 | 0.981 (0.959-1.003) | .824 |
| 65-74 | 0.976 (0.960-0.993) | .005 |
| 75-84 | 0.990 (0.978-1.002) | .096 |
| ≥85 | 1.009 (0.993-1.025) | .254 |
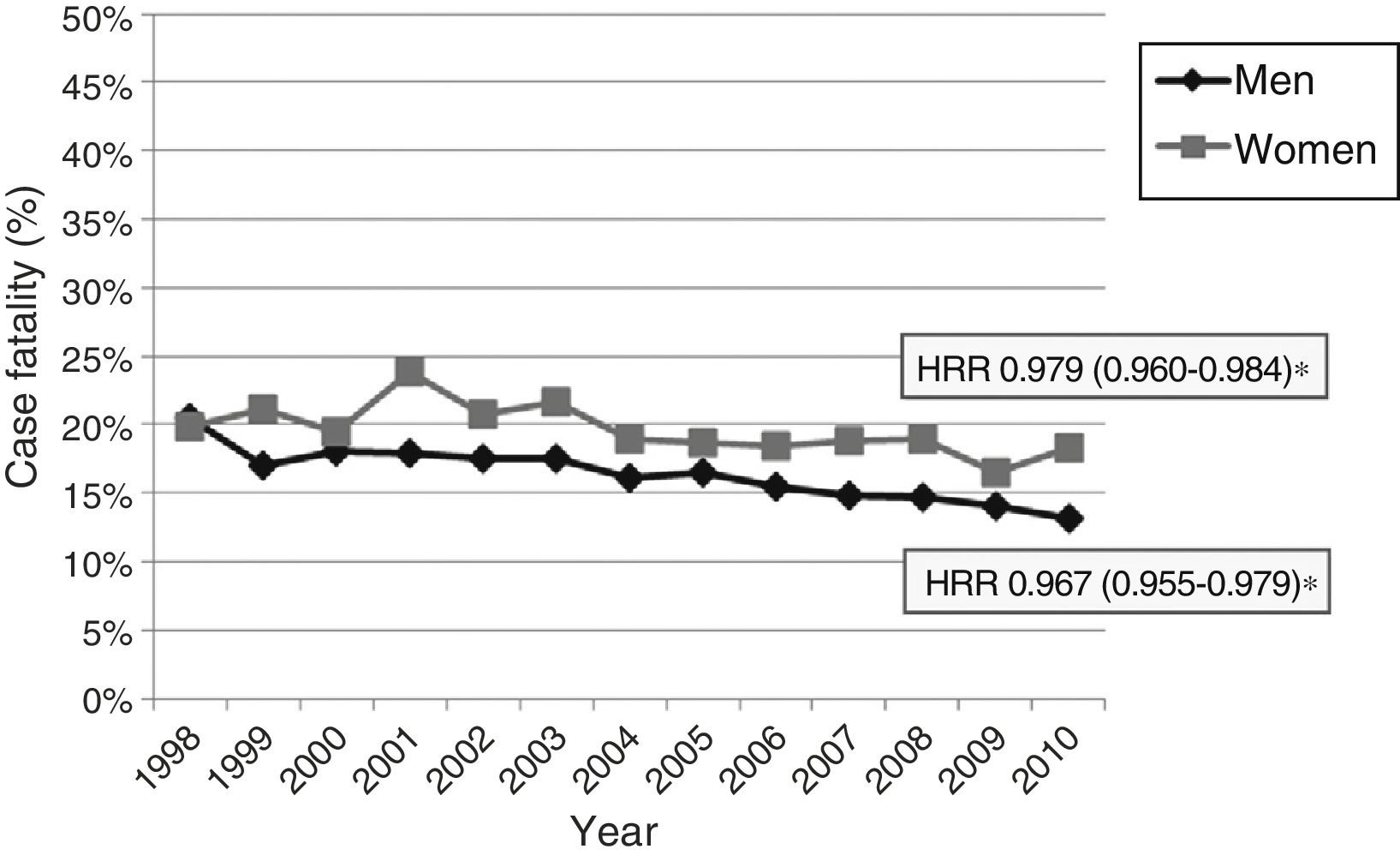
The case fatality rate at 28 days after admission was 17.9%. Mortality rates were highest among patients with intracerebral haemorrhage (35.8%), followed by patients with subarachnoid haemorrhage (26.2%) and ischaemic stroke (13%).
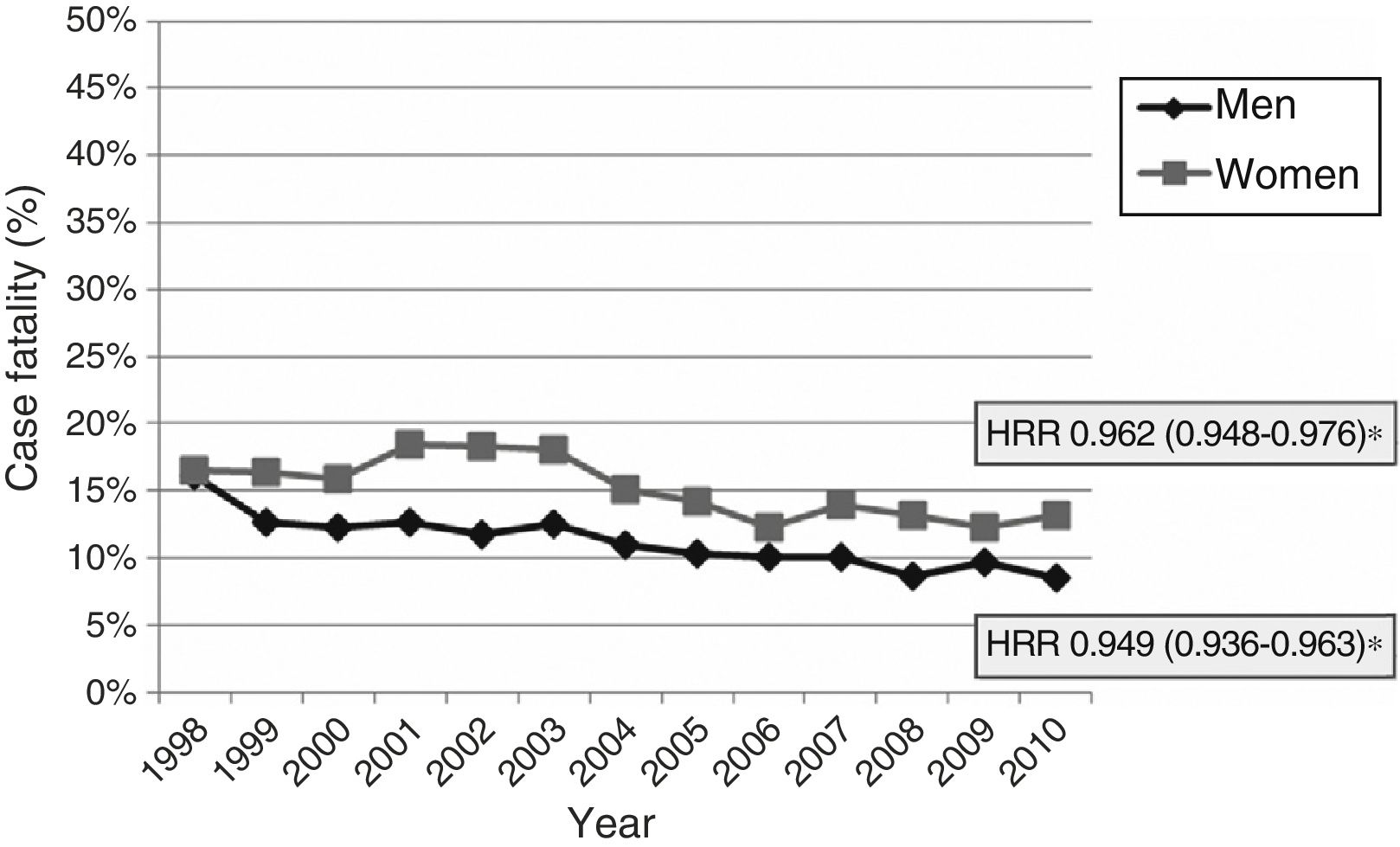
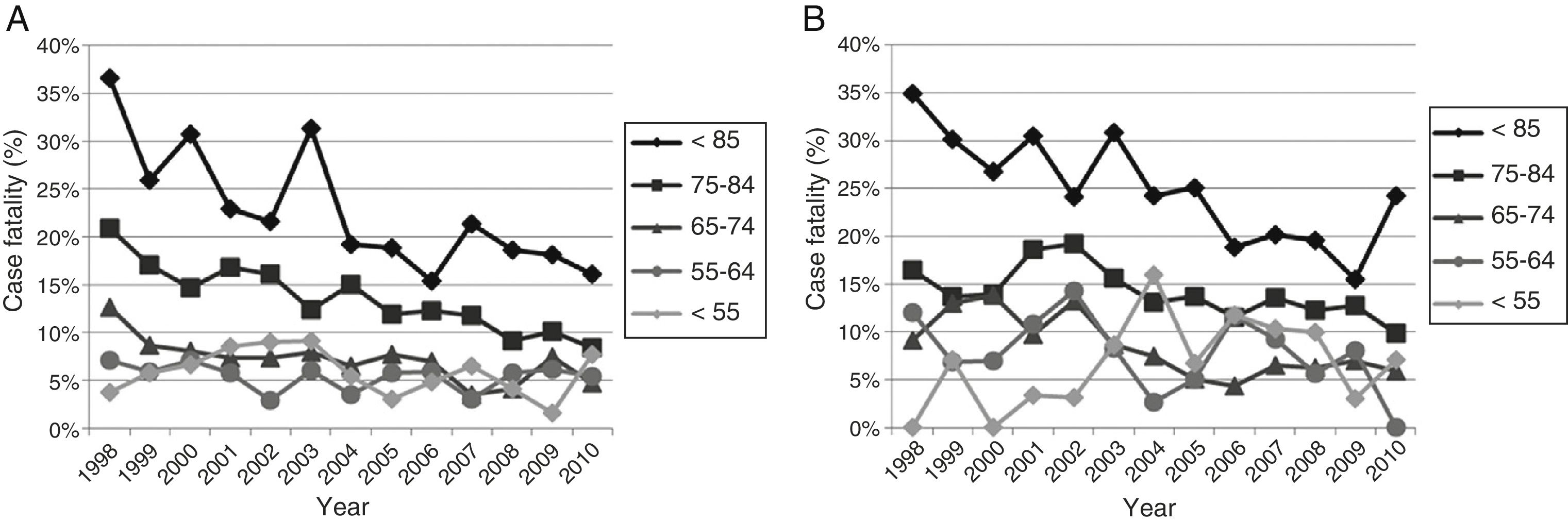
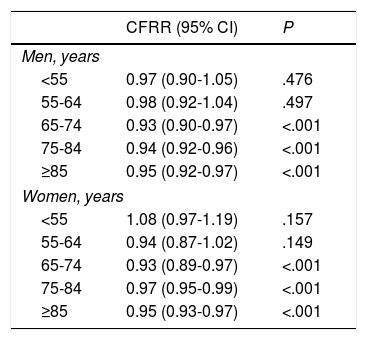
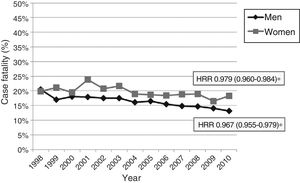
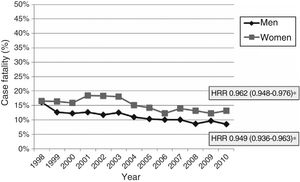
Early case fatality due to acute stroke showed a mean annual decrease of 2.8% (Fig. 4). No significant variations were observed in case fatality rates for subarachnoid haemorrhage or intracranial haemorrhage, either globally or by sex or age group. Case fatality due to ischaemic stroke decreased significantly over the study period; decreases were more marked in men than in women (mean annual decrease of 5.1% vs 3.8%) (Fig. 5). Analysis by age group revealed a significant decrease in case fatality due to ischaemic stroke in patients older than 65 for both sexes (Fig. 6 and Table 3).
Case fatality rate ratio (CFRR) for ischaemic stroke for the period 1998-2010, broken down by sex and age group.
| CFRR (95% CI) | P | |
|---|---|---|
| Men, years | ||
| <55 | 0.97 (0.90-1.05) | .476 |
| 55-64 | 0.98 (0.92-1.04) | .497 |
| 65-74 | 0.93 (0.90-0.97) | <.001 |
| 75-84 | 0.94 (0.92-0.96) | <.001 |
| ≥85 | 0.95 (0.92-0.97) | <.001 |
| Women, years | ||
| <55 | 1.08 (0.97-1.19) | .157 |
| 55-64 | 0.94 (0.87-1.02) | .149 |
| 65-74 | 0.93 (0.89-0.97) | <.001 |
| 75-84 | 0.97 (0.95-0.99) | <.001 |
| ≥85 | 0.95 (0.93-0.97) | <.001 |
Code 436 (acute, but ill-defined, cerebrovascular disease) accounted for 14.9% of diagnoses in 1998. This diagnosis decreased progressively at a mean annual rate of 21%, dropping to 0.6% in 2010.
DiscussionHospitalisation ratesThe number of admissions due to acute stroke increased by 13% over the study period, whereas the hospitalisation rate for acute stroke decreased at a mean annual rate of 1.6% from 1998 to 2010. No significant changes were observed in women. Men, in contrast, display diverging trends depending on the age group: hospitalisation rates decreased significantly among men younger than 85 years, and increased in patients aged 85 years and older (this increase is not significant, however). In line with observations made in most developed countries, our results show a decrease in stroke incidence rates. We should bear in mind, however, that data on stroke incidence time trends are limited: very few specific population registers with an appropriate methodology and long-term data are available. One of these is the register by Rothwell et al.,10 which shows a 29% decrease in the stroke incidence rate in Oxfordshire (United Kingdom); this was attributed to a significant decrease in tobacco use and untreated arterial hypertension and dyslipidaemia. Significant decreases have also been observed in other populations, including in Perth (Australia),11 Auckland (New Zealand),12 Oyaube (Japan),13 Joinville (Brazil),14 Finland,15 the United States,16 and Canada.17 Although most studies report decreases in the incidence of stroke, there are some exceptions. In our setting, Muñoz-Rivas et al.18 analysed hospitalisation and case fatality trends for ischaemic stroke from 2003 to 2012 in diabetic and non-diabetic patients using the Spanish MBDS, and reported a 2% increase in hospitalisation due to ischaemic stroke in diabetic patients and a 3% increase in non-diabetic patients. Increased stroke incidence rates have also been reported in other European countries, including Sweden (Malmö,19 Lund-Orup20) and Denmark.21 Incidence rates have stabilised in other regions, such as Dijon (France).22
Analysis by stroke type identified no significant differences in hospitalisation rates for subarachnoid and intracerebral haemorrhage. We found no statistically significant changes over time for ischaemic stroke; the analysis by age group does show noteworthy differences, however. Hospitalisation rates increased in women younger than 55 years old but showed no significant changes in men of that age range. Rates decreased in men aged 55-64, but not in women within the same age range. For ages 65-84, hospitalisation rates decreased in both sexes; non-significant increases were observed for both men and women aged 85 years and older. These inter-sex differences in incidence trends have been observed in other studies, which report more marked decreases in stroke incidence in men.23–25 The differences observed in the younger groups (<65 years) may be explained by inter-sex differences in the incidence of some classical risk factors for stroke, such as obesity and tobacco use. According to the Spanish National Health Survey, the prevalence of obesity has increased in all Spanish autonomous communities, especially in women (obesity is known to cause greater cardiovascular damage in middle-aged women).26 Tobacco use was also found to have increased among women older than 45 years, in contrast with a decrease observed in men in that age range. Furthermore, cardiovascular risk tends to be underestimated in women: only a small minority attains the optimal lipid levels defined by clinical practice guidelines.27
Case fatality ratesIn our sample, the case fatality rate at 28 days was 17.9%, a somewhat lower rate than those estimated for other developed countries (20%-30%).15,22,28–31 This may be due to the fact that our register did not include data on deaths outside the hospital (before admission or after discharge). Early case fatality due to CVD decreased at a mean annual rate of 2.8%; this may be largely explained by the healthcare improvements seen in the past decade. Decreases in both case fatality and incidence rates may have contributed to the progressive decrease in stroke mortality registered in our setting in recent years (a 36% decrease over the past 10 years).32 The MONICA project (Multinational Monitoring of Trends and Determinants in Cardiovascular Disease)33,34 was launched in the early 1980s at 32 centres in 21 countries to monitor cardiovascular disease time trends and to assess changes in risk factors over a 10-year period. This project aimed to determine the extent to which decreases in mortality were explained by decreases in case fatality and incidence of cardiovascular disease; according to the results, around two-thirds of the decrease in mortality rates were explained by decreases in case fatality, and the remaining one-third, by a decrease in the incidence rate.35
We observed significant changes in case fatality for ischaemic stroke, which explains the overall decrease in mortality. Our study is consistent with a majority of population studies, which report a downward trend in case fatality due to ischaemic stroke.30,31 The differences in the extent of the decrease in case fatality rates may be linked to differences in age and stroke type. Numerous studies have reported a greater incidence of cardioembolic stroke in women; this type of stroke is more severe and is therefore associated with higher case fatality rates.36,37 According to some recent studies, such as the one conducted by the Japan Standard Stroke Registry study group, cardioembolic stroke is more severe in women than in men.38 Studies based on administrative data, as is the case of the present study, cannot analyse stroke subtype; we are therefore unable to provide further information in this respect. Prospective hospital-based registers, such as the one conducted at Hospital Sagrat Cor in Barcelona37 and the Lausanne Stroke Registry (France),39 constitute the most adequate tool to assess this and other clinical aspects.
Use of code 436Although code 436 is non-specific, its validity for diagnosing acute stroke has been confirmed by multiple studies.40–42 This code may have been chosen by the person coding patient data due to inaccuracies in the discharge report: reports may lack detailed information about stroke type, aetiological subtype, or topographic classification; the code may even have been selected generically. We observed a significant decrease in the use of code 436 as the main diagnosis throughout the study period (from 14.9% in 1998 to 0.6% in 2010). This reflects the significant improvements seen in the quality and accuracy of diagnostic coding for CVD and in the quality of stroke assessment and diagnosis over the past 13 years in the hospitals of the autonomous community of Aragon. Continuing improvement in diagnostic coding in the hospitals of Aragon will provide more reliable hospital-based data for epidemiological research.
LimitationsThe reliability of our data depends entirely on the reliability and accuracy of diagnostic coding. No validation studies have been conducted into CVD diagnostic coding in Aragon or Spain; we should therefore be mindful that the diagnoses recorded may not be accurate, and that such inaccuracies may have fluctuated over the study period.
Given that our register is hospital-based, we were unable to include those patients with acute stroke who were not admitted to any hospital in Aragon. As a result, we did not estimate the incidence rate, but rather the hospitalisation rate. Hospitalisation rates depend on incidence, but the 2 concepts are not directly comparable. In any case, it is estimated that only 6% to 8% of cases are not admitted to hospital; hospitalisation and incidence rates are therefore likely to be very similar.43,44
As we have no data on whether events were first-ever strokes or stroke recurrences, we do not know whether the decreases observed in hospitalisation rates result from a decrease in the incidence rate, the recurrence rate, or both.
We are aware that our study does not cover the whole spectrum of acute CVDs. Despite their clinical and epidemiological relevance, we decided to exclude transient ischaemic attacks from our study, for 2 main reasons: (1) it is estimated that up to 50% of patients experiencing transient ischaemic attacks do not go to hospital, and (2) clinical practice guidelines for the management of this condition have achieved a substantial decrease in the rate of admission of these patients, who undergo basic diagnostic studies during their visit to the emergency department.45 Recent changes in the definition of transient ischaemic attack may also make it difficult to study the time trends of this type of stroke.
StrengthsUnlike in other studies analysing all the data from hospital-based administrative registers, our study filtered data drawn from the MBDS. This is essential to identify duplicate cases and to avoid including cases of conditions other than acute CVD. Discharges from rehabilitation centres correspond to patients transferred from general hospitals: including these cases would therefore result in data duplication. We decided to exclude cases from private health centres (these were nonetheless very few) due to insufficient data quality and the great year-on-year variability in the number of cases.
Our study provides novel data on CVD time trends in Aragon; as it includes data from the entire population of the region (from both urban and rural areas), it provides a more complete picture of CVD in Aragon. We analysed the data as a whole and by group to obtain CVD patterns and time trends in Aragon in general, and by stroke subtype, age, and sex.
ConclusionIncreasing our knowledge of the current burden of CVD and recent time trends in our setting will help us estimate the future burden of CVD, which will in turn contribute to designing suitable healthcare planning strategies. Population ageing is expected to lead to increases in the number of cases of CVD and of people with disability, the duration of hospital stays, and the need for institutionalisation. This will result in an increase in the global burden of stroke, turning CVDs into a true challenge for future generations.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Giménez-Muñoz A, Ara JR, Abad Díez JM, Campello Morer I, Pérez Trullén JM. Tendencia de las tasas de hospitalización y de letalidad hospitalaria de la enfermedad cerebrovascular aguda en Aragón en el periodo 1998-2010. Neurología. 2018;33:224–232.